-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2533-2536
doi:10.5923/j.ajmms.20241410.18
Received: Sep. 26, 2024; Accepted: Oct. 14, 2024; Published: Oct. 18, 2024

MRI Findings in Patients with Bilateral Anterior TMJ Disc Dislocation
Ulugbek Nuritdinov1, Ravshan Fattakhov2
1Samarkand State Medical University, Samarkand, Uzbekistan
2Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Ravshan Fattakhov, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents data on an MRI study of patients with bilateral anterior dislocations of the temporomandibular joint discs and changes occurring in the discs in comparison with healthy individuals. In patients with bilateral anterior TMJ disc dislocation, on the right side, the TMJ discs with the mouth closed are 0.17 mm longer and 0.04 mm narrower than with the mouth open; on the left side, with the mouth closed, they are 0.13 mm longer and 0.01 mm narrower than with the mouth open. Шn patients with bilateral anterior TMJ disc dislocation the TMJ discs with the mouth closed are longer and narrower than with the mouth open on both sides.
Keywords: TMJ, TMD, MRI
Cite this paper: Ulugbek Nuritdinov, Ravshan Fattakhov, MRI Findings in Patients with Bilateral Anterior TMJ Disc Dislocation, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2533-2536. doi: 10.5923/j.ajmms.20241410.18.
Article Outline
1. Introduction
- To identify “internal disorders of the TMJ”, a non-invasive, safe diagnostic method is mainly used - magnetic resonance imaging (MRI). This study makes it possible to obtain an accurate image of the periarticular tissues of the TMJ without radiation exposure, which makes its use particularly informative not only during direct examination. MRI provides additional information about the condition of the adjacent soft tissue structures of the head and neck [1,3].Use of MRI diagnostics has significant advantages in identifying organic or structural disorders even in muscle, fat and cartilage tissues [2,4]. This method allows you to successfully visualize the elements of the TMJ at all phases of joint movement in the closed and open mouth stage, identify pathologies of the articular disc, synovial membrane, intra-articular ligaments, bilaminar zone, ascertain the presence of exudative-proliferative, degenerative-dystrophic, destructive manifestations in cartilaginous and fibrous tissues. structures (Badel T. et al., 2009; Imanimoghaddam M. et al., 2016).
2. The Purpose of the Study
- The goal was study the topographic and anatomical features of TMJ disc dislocations using magnetic resonance imaging.
3. Materials and Methods
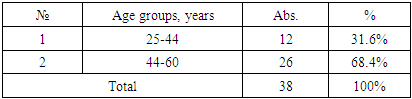
- This group of patients consisted of 38 individuals diagnosed with bilateral anterior TMJ disc dislocation. Their distribution by age is presented as follows (Table 1).
|
4. Results and Discussion
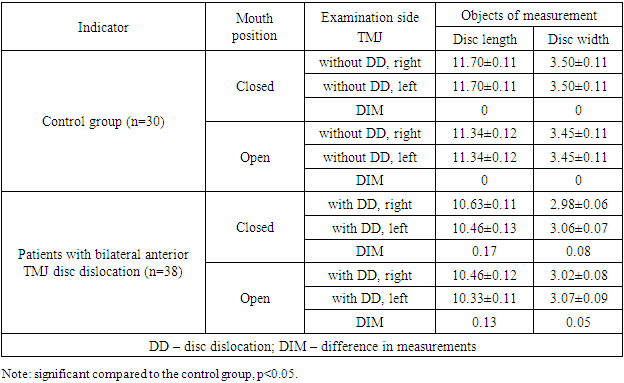
- Anterior displacement of the TMJ disc by half its length was found in 3 studies with the mouth closed: on the left side 2 studies (5.26% of patients in the group); on the right side 1 study (2.63%).In 21 studies (55.26% of the cases), on the right side with the mouth closed, a forward displacement of the TMJ disc by 2/3 of its length was found. On the left side with the mouth closed - in 26 studies (68.4% of the cases).Anterior displacement of the TMJ disc along its entire length was detected: on the right side with the mouth closed – in 14 studies (36.8% of the number of disc displacements on the right side with the mouth closed); on the right side with the mouth open – 2 studies (5.26% of the number of disc displacements on the right side with the mouth open); on the left side with the mouth closed – 9 studies (23.6% of the number of disc displacements on the left side with the mouth closed); with the mouth open on the left side – 1 study (2.63% of the number of disc displacements on the left side with the mouth open.Anterolateral complete displacement of the TMJ disc was detected with the mouth open on the left side - 2 studies (5.26% of the number of left-sided disc displacements with the mouth open.According to MRI study, it was revealed that the anatomical and topographic changes in the location of the TMJ disc in patients of this group have certain features that were observed in all 38 examined. The central location of the TMJ disc on the right side with a closed mouth was observed in 1 study - 2.63% of the total number of examined in the group, with an open mouth in 37 studies - 97.36% of those examined in the group; with a closed mouth on the left side was observed in 1 study - 2.63%, with an open mouth in 35 studies - 92.1% of those examined in the group.The anterior location of the TMJ disc on the right side with the mouth closed was observed in 37 studies - 97.36% of the total number of subjects in the group, with the mouth open in 1 study - 2.63% of the subjects in the group; with the mouth closed on the left side was observed in 37 studies - 97.36% of the total number of subjects in the group, with the mouth open in 3 studies - 7.9% of the subjects in the group.In 31 cases - 81.5% of the total number of this group examined subjects on the right side and in 30 studies - 78.9% on the left side, the shape of the discs remained unchanged. Changes in the shape of the disc (thinning) were determined in 6 studies - 15.8% on the right side, on the left side in 8 studies - 21.0%. Degenerative changes in the disc on the right and left sides were not observed.According to the results of the MRI study, the sizes of the TMJ articular discs were also measured and compared with the open and closed mouth in patients with bilateral anterior TMJ disc dislocation and the control group. It was found that with the closed mouth on the right side, patients with bilateral anterior TMJ disc dislocation had a decrease in disc length by an average of 1.07 mm compared to the disc length in the control group; with the closed mouth on the left side, a decrease in disc length by 1.24 mm was also observed compared to the disc length in the control group. With the open mouth on the right side, a decrease in disc length by 0.71 mm was observed compared to the disc length in the control group. With the open mouth on the left side, a decrease in disc length by 0.88 mm was observed compared to the disc length in the control group.Comparing the sizes of the TMJ articular disc widths in patients of the control group and patients with bilateral anterior TMJ disc dislocation, it was found that on the right side there was a decrease in the disc width by 0.52 mm, and it was 1.17 times smaller compared to the disc width in patients of the control group with the mouth closed. On the left side there was a decrease in the disc width by 0.44 mm, and it was 1.14 times smaller compared to the disc width in patients of the control group with the mouth closed. With the mouth open, on the right side there was a decrease in the disc width by 0.47 mm, and it was 1.14 times smaller compared to the disc width in patients of the control group. With the mouth open, on the left side there was a decrease in the disc width by 0.38 mm, and it was 1.12 times smaller compared to the disc width in patients of the control group.Analysing the data on the average sizes of the TMJ articular discs, it can be stated that in patients in the control group, the TMJ discs are longer and wider with the mouth closed than with the mouth open on both sides.Comparing the average sizes of the TMJ articular discs in patients with bilateral anterior TMJ disc dislocation, it was found that with the mouth closed, the left side had a 0.17 mm decrease in disc length compared to the right TMJ disc; with the mouth open, the left side had a 0.13 mm decrease in disc length compared to the right TMJ disc. At the same time, the right side of the TMJ had a 0.08 mm decrease in disc width compared to the left side of the TMJ with the mouth closed; with the mouth open, the right side had a 0.05 mm decrease in disc width compared to the left TMJ disc.In patients with bilateral anterior TMJ disc dislocation before treatment, on the right side, the TMJ discs with the mouth closed are 0.17 mm longer and 0.04 mm narrower than with the mouth open; on the left side, with the mouth closed, they are 0.13 mm longer and 0.01 mm narrower than with the mouth open.Analysing the data on the average sizes of the TMJ articular discs, it can be stated that in patients with bilateral anterior TMJ disc dislocation before treatment, the TMJ discs with the mouth closed are longer and narrower than with the mouth open on both sides.The sizes of the TMJ articular discs in the control group and in the group with bilateral anterior TMJ disc dislocation are shown in Table 2.
|
5. Conclusions
- Thus, summarizing the results of studies on the management of patients with bilateral anterior TMJ disc dislocation, which were covered in this section, it should be noted that the inclusion of general clinical studies and proposed additions in the diagnostic and therapeutic measures made it possible to achieve normalization of the ratios of the structural elements of the TMJ, a significant improvement in the clinical situation and quality of life. The proposed method of treating patients with bilateral TMJ disc dislocation made it possible to improve the clinical situation, which was reflected in the improvement of the overall quality of life in patients with unilateral TMJ disc dislocation by 95.3%, and the health status – by 91.6%, compared with data before treatment. After 6 months, all patients had no clinical symptoms.
Limitations
- There are some limitations to this study. Although the study was carried out during 3 years, the sample size was small. Future studies could consider broadening the recruitment range to account for potential influences of all factors on participants’ TMD. Even though a certain degree of bias exists in any randomized clinical trial, we tried to minimize major potential biases. In particular, an independent statistician who was not aware of the name of the participants and group assignment analyzed all our results.
Practical Implications
- The obtained research results, relevant for different age groups, can be used to analyze the development and treatment of TMJ disc dislocations.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML