Muborak Abdullaeva1, Feruza Chorieva1, Yadgarova Lola1, Nalibоyeva Dilorom1, Nurmamatzoda Otabek2, Dadajonova Ziyovuddin1
1Department of Neurological Diseases and Folk Medicine, Tashkent State Dental Institute, Makhtumkuli Str. 103, Tashkent, Uzbekistan
2Department of Surgery Dentistry and Detailed Implantology, Tashkent State Dental Institute, Makhtumkuli Str. 103, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The effect of low-intensity laser radiation in the treatment of acute and chronic pain has now been established in many studies. Trigeminal neuralgia is pain that passes through the branches of the nerve and its trigger is located in the skin or mucous membrane, which can lead to pain in the presence of a trigger stimulus. Branches of the trigeminal nerve are involved in the pain, which sometimes causes patients to seek treatment for several years. Currently, various treatments are used to relieve pain, most of which cause tolerance and various side effects. This article examines the effects of these types of lasers on trigeminal neuralgia, which is one of the most painful diseases known. In various studies, the effect of laser therapy has been compared with placebo irradiation or drug and surgical treatments. Low–intensity laser therapy (LILT) is a treatment strategy that uses a single wavelength light source. Laser radiation and monochromatic light can alter the function of cells and tissues. However, in most studies, laser therapy was associated with a significant reduction in pain intensity and frequency compared to other treatment strategies, and several studies showed that there was no significant difference between the laser group and the placebo group in terms of analgesic effect. Low-intensity laser therapy can be considered in the treatment of trigeminal neuralgia without any side effects.
Keywords:
Trigeminal nerve, Neuralgia, Laser, Low level
Cite this paper: Muborak Abdullaeva, Feruza Chorieva, Yadgarova Lola, Nalibоyeva Dilorom, Nurmamatzoda Otabek, Dadajonova Ziyovuddin, The Role of Laser Therapy in the Treatment of Trigeminal Neuralgia, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2522-2528. doi: 10.5923/j.ajmms.20241410.16.
1. Introduction
According to WHO, the incidence of trigeminal neuralgia is 3-5 cases per 100,000 population per year, with an average of 4.5:100,000.There are classic (primary) and secondary types of trigeminal neuralgia. Classic trigeminal neuralgia is characterized by short-term (from a few seconds to 2-3 minutes) unilateral attacks of excruciating pain like an electric shock. Most often, it is observed in the area of the second and third branches of the trigeminal nerve, and very rarely in the first branch (International classification of headache (3rd edition, beta version (MKGB-3), 2013)). The intensity and frequency of trigeminal neuralgia (TN) painful paroxysms cause mental and physical exhaustion of a person, deprive him of normal work and personal life, often make him leave work. [1]Nowadays, the debate on the pathogenesis of classic trigeminal neuralgia still continues. Some authors consider that narrowing of the exit holes of the trigeminal nerve is pathogenetic importance. In all the works devoted to classic trigeminal neuralgia, it is noted that the disease begins in the majority of elderly patients, but no explanation is given for this fact.In classic trigeminal neuralgia, 2 anatomical structures are involved in the neurovascular collision (NVC): the trigeminal nerve root (TNR) and artery (most often the superior cerebellar artery (SCA), less often the inferior anterior cerebellar artery (IACA) and the basilar artery (BA)). The emergence of NVC occurs with a sharp convergence of these structures and an increase in the traumatic effect of the artery on the neurovascular conflict. The neurovascular collision force of the artery obeys the physical laws of hydrodynamics. In old age, in a vessel that has lost its elasticity, the power of the pulse wave is used not to increase the diameter of the vessel, but to expand the arterial ring, the distal shoulder of which hits the neurovascular conflict with each systole, triggering the mechanism of demyelination.In turn, atherosclerotic vascular modification with increased rigidity of vascular walls is facilitated by endothelial dysfunction. In addition, there is swelling of the trigeminal nerve due to neurovascular conflict, as well as swelling of the conflicting artery walls, which contributes to the development of nerve damage by the compressed vessel, the increase in the number of demyelinated nerve fibers, and causes the emergence and maintenance of severe pain syndrome. [2]Once the cause is identified, treatment involves eliminating the cause. However, in idiopathic cases, different medical and surgical treatment options should be considered. Drug treatments include carbamazepine, phenytoin, baclofen, gabapentin, oxcarbazepine, lamotrigine, pimozide, and tizanidine hydrochloride. Although medication is the first line of treatment, tolerance may develop during treatment and the dose may need to be increased further, leading to more side effects. Approximately 50% of patients with TN will not respond adequately to drug therapy due to inadequate pain control or drug-related side effects. Drowsiness, fatigue, dizziness, nausea, nystagmus, memory loss, and fatigue are common side effects of carbamazepine and require seeking alternative treatment. [4]Low-intensity Laser Therapy (LILT) is a treatment strategy that uses a single wavelength light source. Laser radiation and monochromatic light can change the activity of cells and tissues.LILT is used in the treatment of trigeminal neuralgia without any side effects. The results of clinical studies show that low-intensity laser rays, as a result of the impact on the damaged nerve fiber, lead to the improvement of nerve fiber function and the activation of myelin production activity. Let's look at the results of our research with methods that include specific details of laser therapy.
2. Materials and Methods
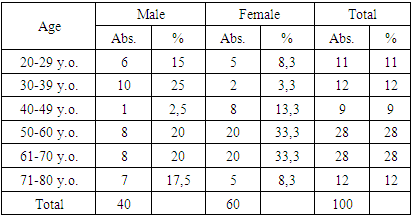
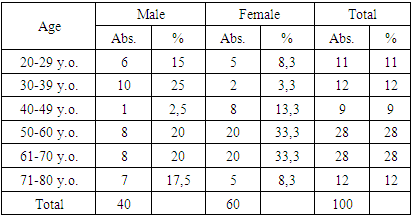
100 patients participated in our clinical study, their average age was 23-80 years. The differences in age and gender of the patients are described in Table 1.Table 1. Indicators of patients by age and gender
 |
| |
|
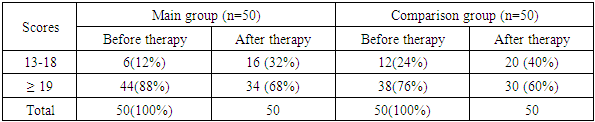
According to Table 1, 40% patients were men and 60% were women, and women consisted of 1.5 times more than men. 70% of the patients were older and elderly patients, the average age of men was 50.8±19.05 years, and the average age of women was 55.5±13.03 years.Examination of the somatic condition showed that arterial hypertension was manifested in the form of somatic pathologies in 70 (70%) patients, in 65 (65%) patients, in the form of ischemic heart disease (28%) in 28 patients (3 of them had a previous myocardial infarction). 4 (4%) cases of diabetes mellitus were noted. It should be noted that the same patient has a combination of two or more somatic diseases, which is especially characteristic of cardiovascular diseases.In the age-related analysis, it was noted that somatic pathology occurs in almost 75% of cases in the elderly and elderly.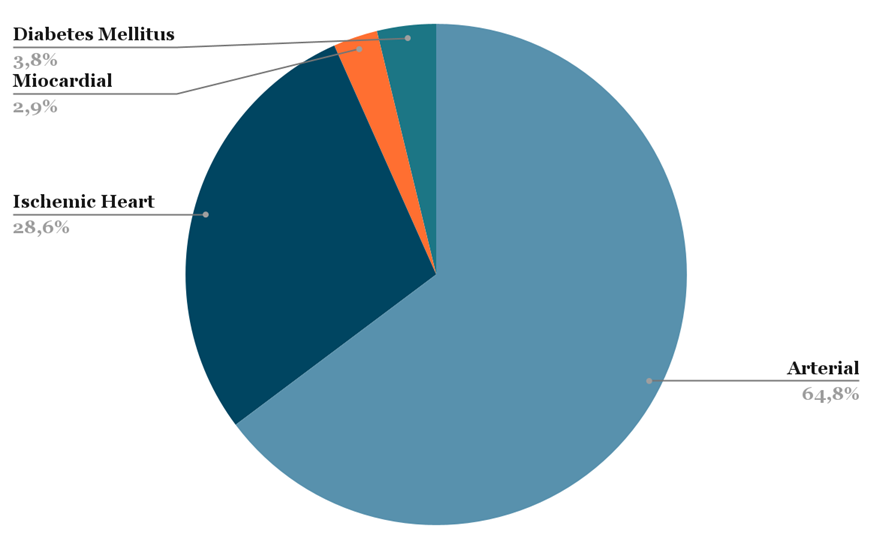 | Figure 1. Somatic status of the studied patients |
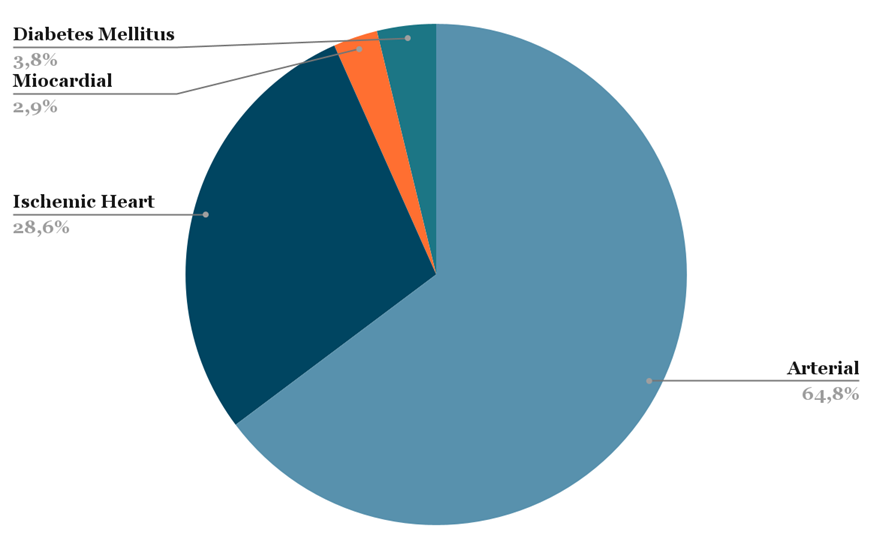
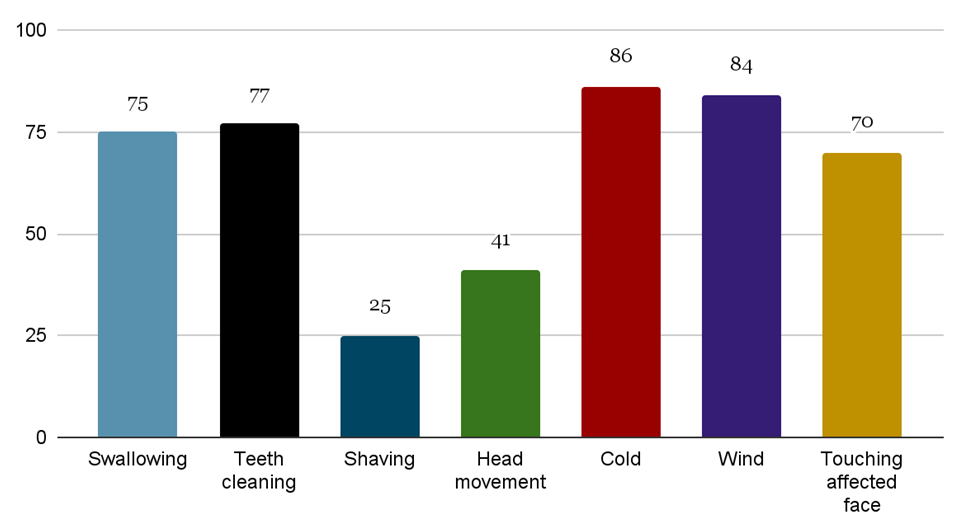
Most of the patients participating in the study had comorbid diseases: cardiovascular diseases: ischemic heart disease 14 (14%); hypertension – 31 (31%); obesity – 23 (23%); atherosclerosis - 25 (25%); diabetes - 2 (2%); if there are diseases of the gastrointestinal tract-4 (4%); thyroid disease - 1 person (1%).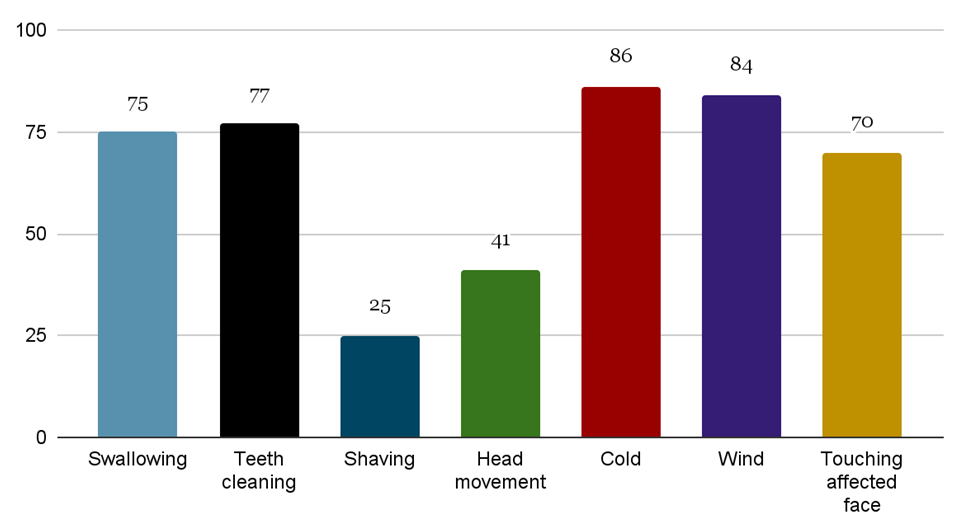 | Figure 2. Factors that trigger pain attacks |
As can be seen from Figure 2, the factors that trigger pain attacks in both groups of patients were: jaw movement (56%), swallowing (75%), brushing teeth (77%), shaving (25%), turning the head (41%), cold (86%), wind (84%), touching the affected half of the face (70%). [5]An objective examination of patients with trigeminal neuralgia revealed the presence of neurological organic microsymptoms in 100% of patients. The analysis of the neurological condition revealed asymmetry of the nasolabial folds in 60 (60%) patients. In the area of innervation of the trigeminal nerve network, signs of peripheral sensory loss were found in 91.5% of cases of sensory deficits in the orofacial region, and in 41 (41%) patients, loss of temperature and pain sensation in the upper part of the legs and arms, in 33 (33%), 36% of patients acrogiperhidrosis and acrogypothermia signs are found.Visual analogue scale (VAS), Pain Detect and McGill pain questionnaire were used to study and evaluate pain syndrome, as well as to conduct catamnetic studies. Long-term outcomes were evaluated by following up patients during the dispensary follow-up period by answering questionnaire questions during the period of disease relapse.
3. Results
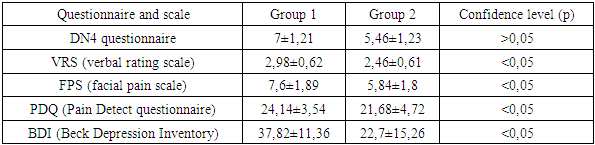
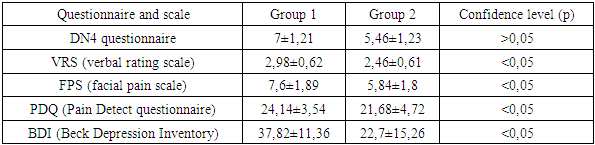
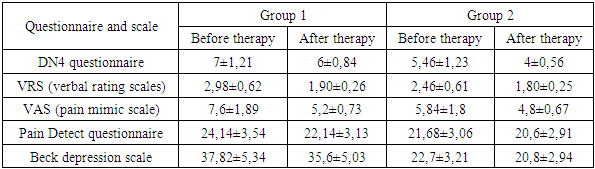
Table 2 shows the results of the research groups on the scales and questionnaires.Table 2. Indicators of research groups on scales and questionnaires
 |
| |
|
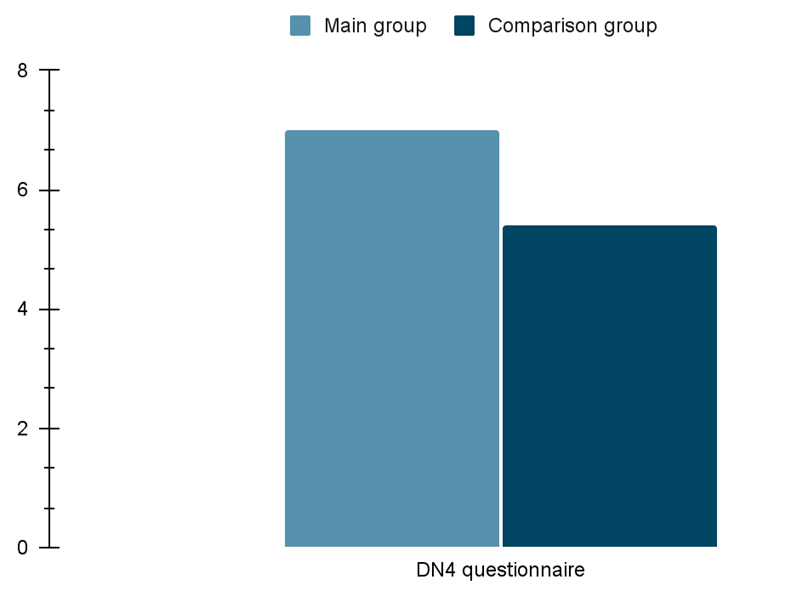
 | Figure 3. DN4 survey results |
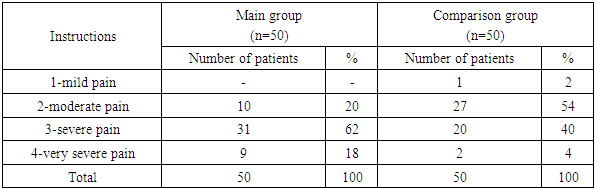
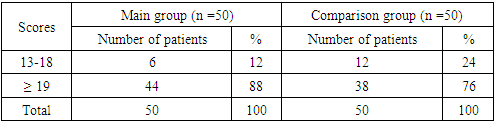
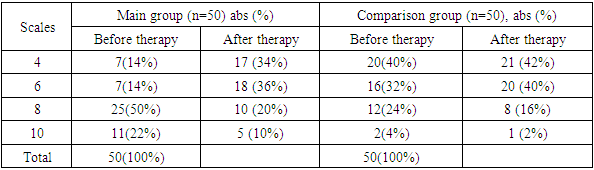
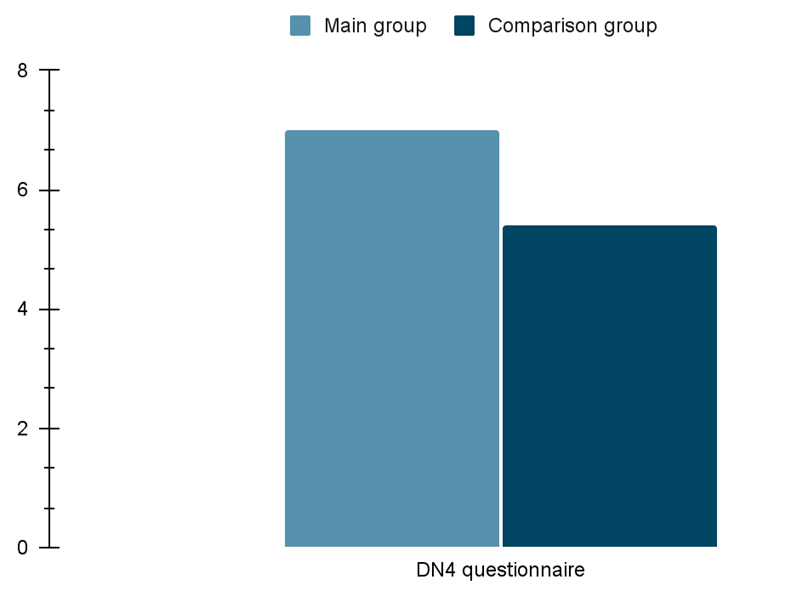
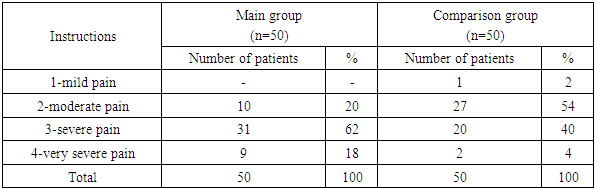
As shown in Figure 3, the DN4 questionnaire score was 7±1.21 in the pain baseline group and 5.4±1.23 in the comparison group. Accumulated points indicate that the pain paroxysm is of a neuropathic type. There were no significant differences between patients in different groups.The results of the verbal rating scale of the compared groups are presented in Table 3.Table 3. VRS (verbal rating scale)
 |
| |
|
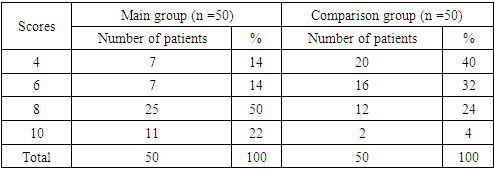
Table 4 describes the results of the pain assessment on the mimic scale.Table 4. VAS (Pain Assessment Scale)
 |
| |
|
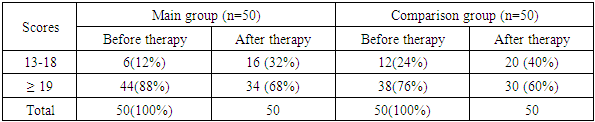
Table 5 describes the results of the Pain Detect pain questionnaire.Table 5. Pain Questionnaire by Pain Detect
 |
| |
|
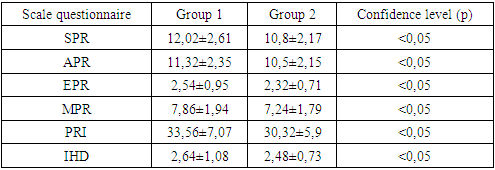
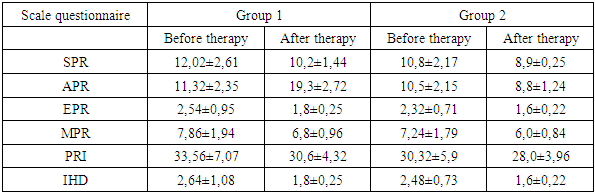
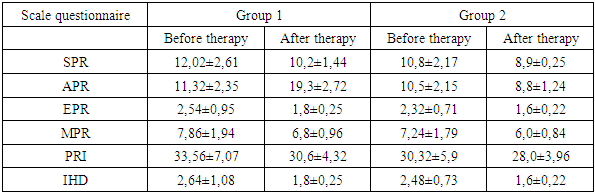
The results of SPR, APR, EPR, MPR and PRI values for both groups are presented in Tables 6. The average value of the sensory component in the first group was 12.02±2.61, and in the second group it was 10.8±2.17. The average value for the sensory component in the first group was 11.32±2.35 and in the second group it was 10.5±2.15. The average value of the mixed component in the first group was 7.86±1.94, and in the second group it was 7.24±1.79. The pain index in the first group was 33.56=7.07 points, and in the second group it was 30.32=5.9 points. [6]Table 6. McGill Pain Questionnaire
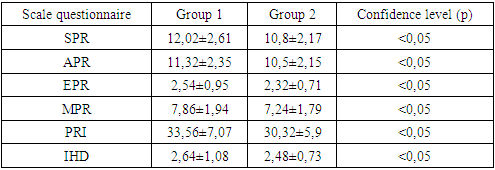 |
| |
|
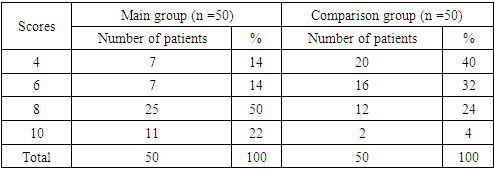
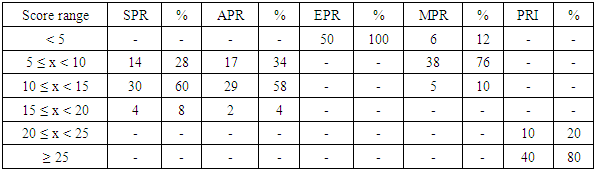
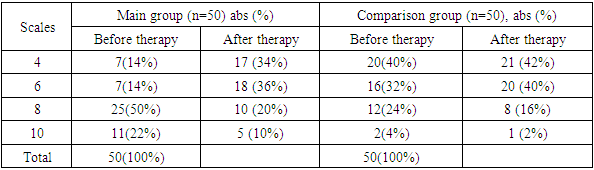
The values of the parameters of the McGill scale for the main group are shown in Table 7. In the first group, the majority of patients (80%) scored more than 25 points, 20% of respondents scored between 20 and 25 points.Table 7. McGill pain questionnaire parameters of group 1 patients
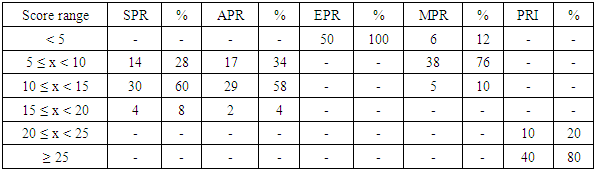 |
| |
|
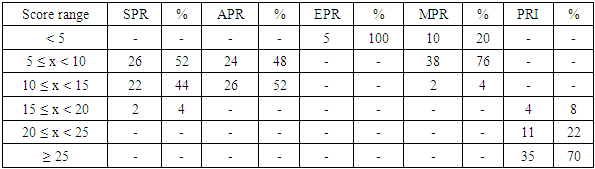
The values of the parameters of the McGill scale for the comparison group are shown in Table 8. In the second group, 15-20 points were recorded in 8% of all patients, 20-25 points were recorded in 25% of patients, and most (70%) patients had more than 35 points.Table 8. McGill pain questionnaire parameters of group 2 patients
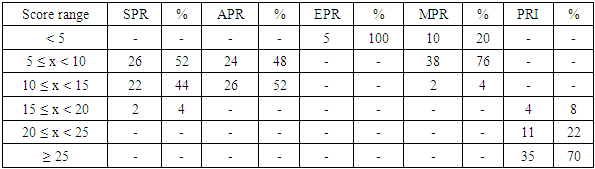 |
| |
|
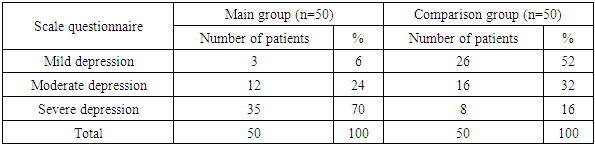
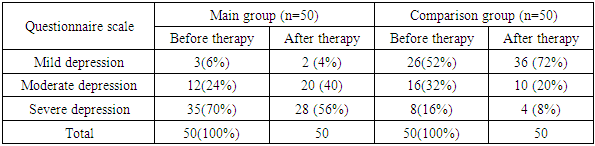
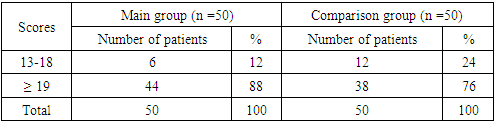
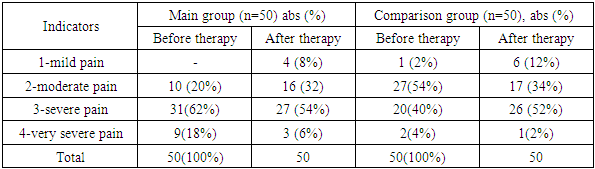
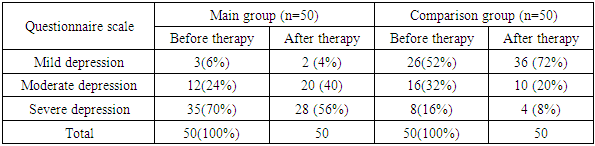
Table 9 presents the results of examining patients in research groups according to the Beck depression scale. In the main group, 3 patients with mild depression (6%) scored 10-15 points, and in comparison group, 26 patients (52%) scored. Average depression was observed in 12 patients (24%) with a score of 16-19, compared to 16 (32%) in the comparison group. [3]Table 9. Beck Depression Scale
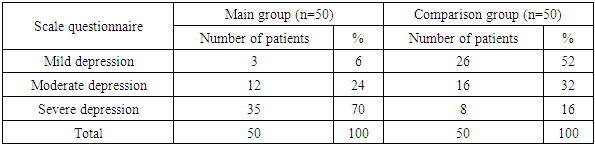 |
| |
|
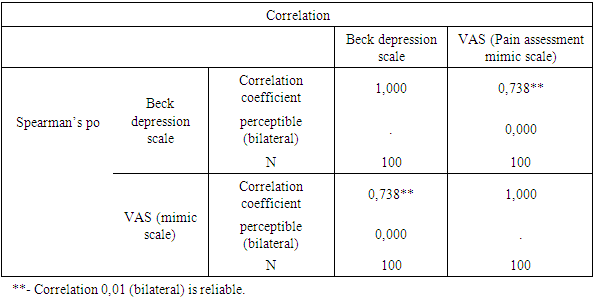
Table 10 shows the correlation between the Beck depression scale and the VAS scale in the observation groups.Table 10. Correlation between the Beck depression scale and the VAS scale
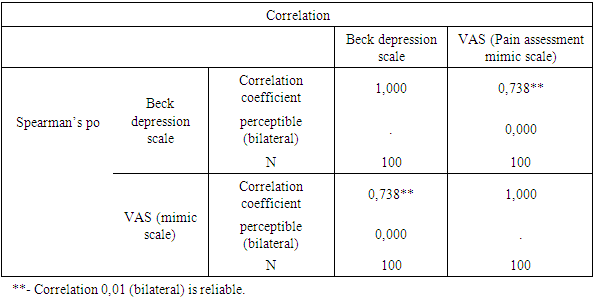 |
| |
|
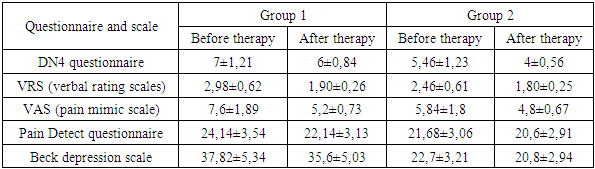
As can be seen from Table 10, in the analysis of the obtained data, a significant correlation was found between the results of the data and VAS scale in the general population (n-100) of patients examined according to the Beck depression scale. That is, we found a close relationship between the Beck depression scale and VAS scale used to assess the intensity of chronic pain syndrome (Rs=0.738 ((r<0.001)).Thus, patients of different ages react differently to pain syndrome. Based on the obtained data, we proved that the intensity of the pain syndrome can be assessed according to the Beck depression and VAS pain scales. The Beck depression scale and VAS pain scale used in our study do not reflect an objective picture of acute pain, especially in the comparison group. However, older patients with concomitant diseases and stenosis of the vertebral arteries experience more pain.We found a correlation between the data on Beck depression scale and VAS in the examined population of patients with pain syndrome, which allows us to use these two methods separately in these patients.We divided our patients who participated in our study into two groups: the main group (50 patients) and the second group (50 patients). The second group of patients received only standard treatment methods.Post-treatment results of patients participating in our study:Table 11. Post-treatment changes in scores on scales and questionnaires in the examined patient group
 |
| |
|
Table 11 shows the post-treatment results of the visual analogue scale (VAS) and the Pain Detect and McGill pain questionnaires for studying and evaluating pain syndromes, as well as for catamnetic studies.Table 12. VRS (verbal rating scale)
 |
| |
|
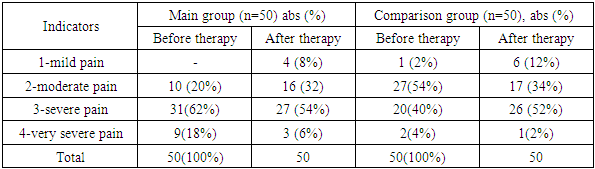
The results of VRS (Verbal Rating Scale) used to assess the intensity of pain in the patients of our research groups show a significant decrease in the intensity of pain in our groups of patients who received laser therapy. [8]Table 13. VAS (Pain Assessment Mimic Scale)
 |
| |
|
VAS (Pain Assessment Mimic Scale) results also showed improvement in both groups with group 2 predominance.Table 14. Pain Questionnaire by Pain Detect
 |
| |
|
Changes in our post-treatment questionnaires in our study groups are presented in Table 14. Based on it, changes in the DN4 questionnaire were observed in both study groups, with a decrease in neuropathic pain and a decrease in the negative sensory symptom allodynia. These indicators were evident in our 2nd group patients. [7]Table 15. McGill Pain Questionnaire
 |
| |
|
Table 16. Beck Depression Scale
 |
| |
|
4. Summary
Trigeminal neuralgia often develops in adults and elderly people against the background of somatic and neurological pathology. Trigeminal neuralgia is more common in middle-aged and elderly patients, accounting for 70% of cases. Among the patients, women predominate with 60%. Clinical signs of TN are determined by the symptom complex of lesions, and the most characteristic symptoms are the presence of trigger zones of pain development, which are noted in 97% of patients. Damage to the second (32.5%) and the second+third branches (53%) with a simultaneous right-sided localization of the process (42.5%) is often observed.Studies have shown that low-intensity laser therapy can be considered in the treatment of trigeminal neuralgia. The laser relieves pain without any side effects. This may be particularly helpful in patients with drug-tolerant neuralgia. It should be noted that differentiating neuralgia from other chronic pain such as atypical facial pain is important for effective treatment.
References
| [1] | Cheshire, W. P., Jr, & Wharen, R. E., Jr (2009). Trigeminal neuralgia in a patient with spontaneous intracranial hypotension. Headache, 49(5), 770–773. https://doi.org/10.1111/j.1526-4610.2009.01403.x. |
| [2] | Jainkittivong, A., Aneksuk, V., & Langlais, R. P. (2012). Trigeminal neuralgia: a retrospective study of 188 Thai cases. Gerodontology, 29(2), e611–e617. https://doi.org/10.1111/j.1741-2358.2011.00530.x. |
| [3] | Siddiqui MN, Siddiqui SS, Ranasinghe JS, Furgang FA. Pain relief: trigeminal neuralgia. Hospital doctor. 2003; 39:64–70. [Google Scholar] |
| [4] | Fromm G. H. (1994). Baclofen as an adjuvant analgesic. Journal of pain and symptom management, 9(8), 500–509. https://doi.org/10.1016/0885-3924(94)90111-2. |
| [5] | Baker, K. A., Taylor, J. W., & Lilly, G. E. (1985). Treatment of trigeminal neuralgia: use of baclofen in combination with carbamazepine. Clinical pharmacy, 4(1), 93–96. |
| [6] | Cheshire W. P. (2005). Trigeminal neuralgia: diagnosis and treatment. Current neurology and neuroscience reports, 5(2), 79–85. https://doi.org/10.1007/s11910-005-0003-6. |
| [7] | de Tommaso M. (2008). Laser-evoked potentials in primary headaches and cranial neuralgias. Expert review of neurotherapeutics, 8(9), 1339–1345. https://doi.org/10.1586/14737175.8.9.1339. |
| [8] | Lorenzini, L., Giuliani, A., Giardino, L., & Calzà, L. (2010). Laser acupuncture for acute inflammatory, visceral and neuropathic pain relief: An experimental study in the laboratory rat. Research in veterinary science, 88(1), 159–165. https://doi.org/10.1016/j.rvsc.2009.06.001 |
| [9] | Chung, W. Y., Liu, K. D., Shiau, C. Y., Wu, H. M., Wang, L. W., Guo, W. Y., Ho, D. M., & Pan, D. H. (2005). Gamma knife surgery for vestibular schwannoma: 10-year experience of 195 cases. Journal of neurosurgery, 102 Suppl, 87–96. |
| [10] | Park, S. H., Hwang, S. K., Kang, D. H., Park, J., Hwang, J. H., & Sung, J. K. (2010). The retrogasserian zone versus dorsal root entry zone: comparison of two targeting techniques of gamma knife radiosurgery for trigeminal neuralgia. Acta neurochirurgica, 152(7), 1165–1170. https://doi.org/10.1007/s00701-010-0610-0. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML