-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2500-2506
doi:10.5923/j.ajmms.20241410.11
Received: Sep. 5, 2024; Accepted: Oct. 3, 2024; Published: Oct. 16, 2024

Effectiveness of Treatment of Suprastenotic Esophagitis as Prevention of Complications of Esophageal-Intestinal Anastomoses
Yangiyev Akhmad Khodjaevich, Khudaykulov Bobakul Karjovovich, Alimova Zebo Farkhadovna, Kholmurodov Inoyatullo Kholmurodovich, Kurbonova Gulnoza Abdurakhimovna
Assistants of Termiz University of Economics and Service, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

As you know, reconstructive surgery on the esophagus is one of the most difficult in plastic surgery. According to the literature, the number of chemical burns of the esophagus has recently increased. 45% of patients with this pathology are subject to surgical intervention. However, reconstructive surgery-resection of the esophagus followed by thin- or thick-intestinal plasty is often complicated by scarring of esophageal anastomoses and their insufficiency. To a large extent, this is facilitated by suprastenotic esophagitis with a severe degree of inflammation not only in the mucous membrane, but also in the underlying layers of the esophagus, the presence of a large number of pathogenic strains of microorganisms, etc. Therefore, the treatment of suprastenotic esophagitis is one of the effective ways to prevent the above postoperative complications.
Keywords: Forward facially, Scarred, Anastomosis, Gastrostomy, Suprastenotic esophagitis, Laser therapy, Augmentation, Scar stricture, Reconstructive surgery, Esophagospasm
Cite this paper: Yangiyev Akhmad Khodjaevich, Khudaykulov Bobakul Karjovovich, Alimova Zebo Farkhadovna, Kholmurodov Inoyatullo Kholmurodovich, Kurbonova Gulnoza Abdurakhimovna, Effectiveness of Treatment of Suprastenotic Esophagitis as Prevention of Complications of Esophageal-Intestinal Anastomoses, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2500-2506. doi: 10.5923/j.ajmms.20241410.11.
1. Goal
- Optimization of treatment of suprastenotic esophagitis in patients with post-burn cicatricial strictures of the esophagus as prevention of postoperative complications.
2. Material and Methods
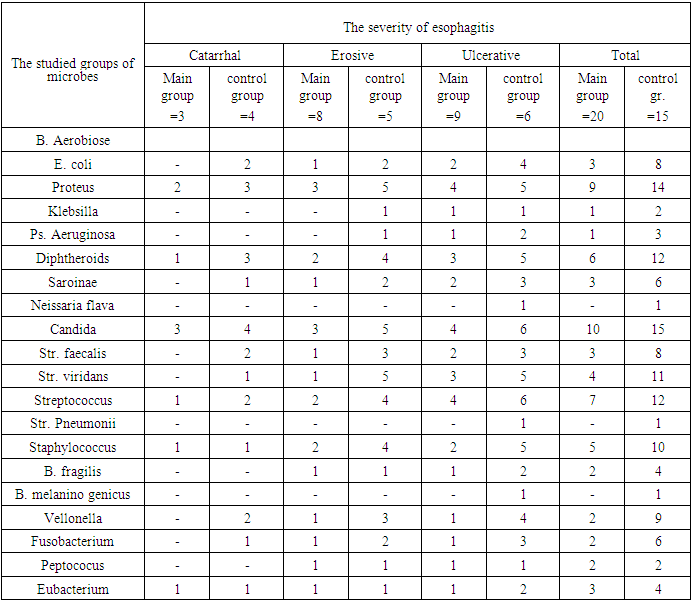
- The results of treatment of 112 patients with post-burn scarring of the esophagus were studied. Suprastenotic enlargement and esophagitis were observed in 89/79.7%/. Among the factors that caused the esophageal burn, in 31 cases they were mistakenly taken by patients, including 15 in a state of intoxication and in 58 cases for suicidal purposes. Organic and inorganic acids were the most common, less often alkalis and other caustic substances. The duration of the esophageal burn was from 3 months to 3 years [1].The causes of suture failure are diverse -these are various pathophysiological factors, the presence of inflammatory changes in tissues, infection, anatomical features, poor blood supply, metabolic disorders associated with malnutrition and starvation, as well as tactical and technical errors made during surgery. The most serious complication of esophageal anastomoses is suture insufficiency. Its frequency ranges from 5 to 17% [1,2,3].In this work, we set out to identify the role of suprastenotic esophagitis in the occurrence of suture failure after radical surgery on the esophagus, determine its frequency and indicate possible ways to prevent these complications.Since 2018- 2023, 89 patients with post-burn scarring complicated by suprastenotic esophagitis have been treated in the department. To develop treatment regimen options, microbiological studies of the material were carried out under conditions of aerobic and anaerobiosis from the anastomosing segments of the digestive tract (esophageal lumen). At the same time, it was noted that in more than half of the cases, aerobic microorganisms were seeded in associations with anaerobic ones. In this regard, antibacterial prophylaxis included drugs active against isolated microorganisms. All patients with post-burn strictures of the esophagus develop esophagitis in the suprastenotic part, the severity of which varies from plaque hyperemia to erosive ulcerative lesions of the mucous membrane.
|
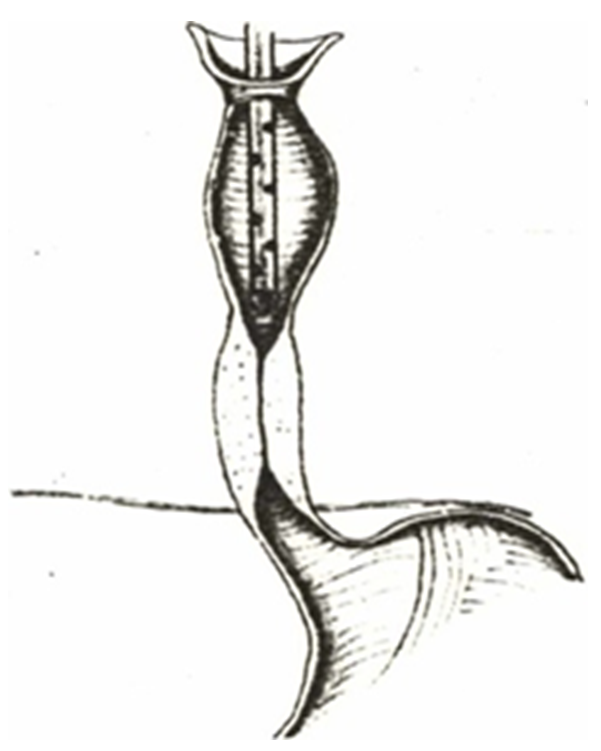 | Picture 1. The method of step-by-step rehabilitation in the proposed way |
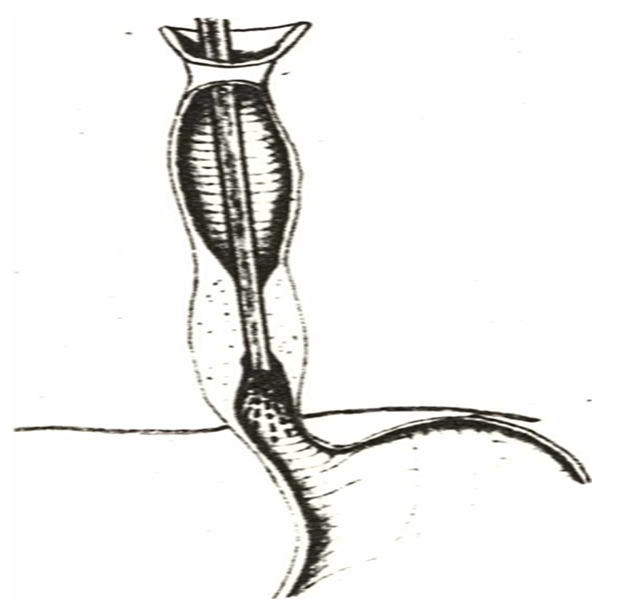 | Picture 2. Laser irradiation Suprastenotic enlarged esophagus |
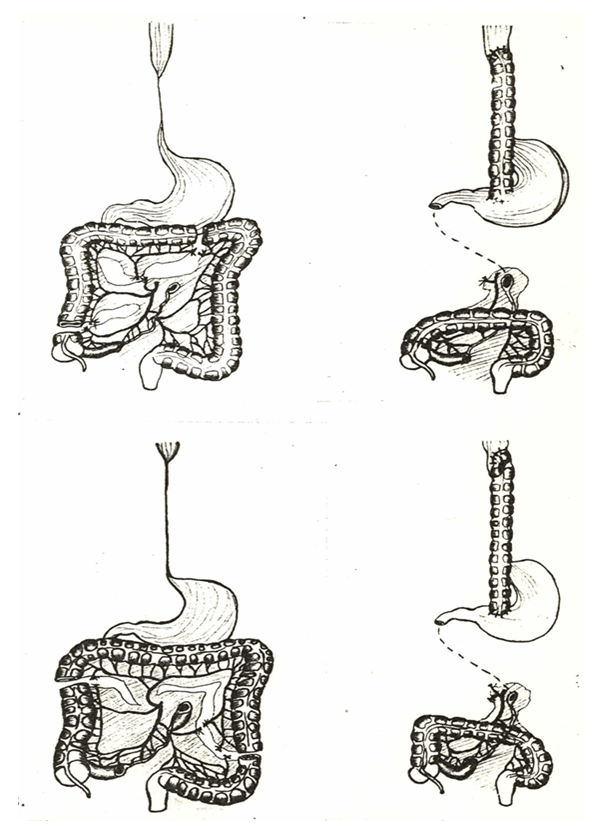 | Picture 3. Esophagoplasty of the transverse-left half of the colon |
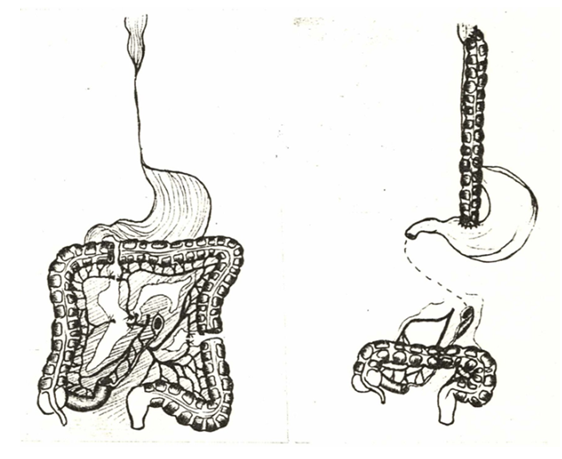 | Picture 4. Esophagoplasty of the left half of the colon |
3. Results and Discussion
- Treatment of cicatricial lesions of the esophagus is a complex and far from solved problem of modern surgery. Despite the significant success of esophageal surgery. Many issues of treatment of burn pathology remain insufficiently developed and the results of reconstructive operations do not always satisfy surgeons.Reconstructive surgery for cicatricial narrowing of the esophagus includes almost all the main difficulties of abdominal and thoracic surgery [7]. It is possible to improve the results of treatment in this group of patients by using new medical achievements, effective surgical interventions, targeted preoperative preparation, intensive management of the postoperative period and active rehabilitation measures.Among the causes contributing to complications after esophageal plastic surgery, inflammatory changes in the wall and mucous membrane of the esophagus as a result of impaired evacuation function are of great importance. The frequency of suprastenotic esophagitis ranges from 87%. The present study aimed to study the morphology and microbiology of the suprastenotic part of the esophagus, to determine the degree of changes that occur and to indicate possible ways to treat and prevent postoperative complications.The work is based on the experience of treating suprastenotic esophagitis after cicatricial narrowing of the esophagus and their complications in 89 patients who were in the department of Surgery of the Tashkent State Medical Institute from 1995 to 1998. All materials in general were analyzed and the results of treatment of patients over the past 5 years/2018-2023/ In the department of surgery of the Surkhandarin branch of the Republican Center for Emergency Medical Care were compared.The outcome of the disease after a chemical burn depended on the degree and depth, type and amount of caustic substance, timely first aid and the results of early treatment. The duration of the burn suffered in most patients ranged from 3 months to 5 years.The age of the patients ranged from 14 to 43 years, there were 32 men and 57 women.The largest number of patients with suprastenotic esophagitis were aged 19-43 years. Therefore, the functional outcome of treatment and labor rehabilitation of patients are of great social and economic importance. Currently, it has been established that the more time patients do not work before surgery after a chemical burn, the less they return to socially useful work after surgery.In this regard, the most rational is to reduce the duration of reconstructive surgery after a burn injury, however, the question of indications and timing of reconstructive surgery for burn lesions of the esophagus remains controversial and insufficiently developed.All admitted patients were examined and according to the results of clinical and instrumental research methods, it was found that the severity of the inflammatory process was distributed as follows1. Catarrhal esophagitis (47 patients).2. Erosive esophagitis (29 patients).3. Erosive ulcerative esophagitis (11 patients).4. Atrophic esophagitis (2 patients).Such a distribution of patients with suprastenotic esophagitis, depending on the nature and severity of changes in the esophageal mucosa and their complications, contributed to the development of rational diagnostic and therapeutic tactics in this cohort of patients. All patients underwent comprehensive treatment, which included a phased rehabilitation of the suprastenotic esophagus by washing with antiseptic solutions of furacilin-decasan-furacilin.Sanitation was carried out 2 times a day with a special two-lumen probe with a metal olive tree for 7-9 days. A day later, the esophagus was irradiated with helium-neon laser radiation after washing. The analgesic and anti-inflammatory effects of laser therapy made it possible to relieve esophagospasm and eliminate the phenomena of esophagitis faster, which was confirmed by endoscopic and morphological studies.Our clinical experience in more than 41 patients suggests that previously therapeutic and prophylactic augmentation and laser therapy in combination with complex therapy are effective methods of prevention and treatment of cicatricial strictures of the esophagus.The microflora was studied in 35 patients and, depending on the type of microorganism detected and its sensitivity to antibiotics, antibacterial therapy was prescribed. The procedure for the rehabilitation of the esophagus ended with the introduction of an appropriate antibiotic into the suprastenotic enlarged part of the esophagus. All patients were divided into 2 groups: 55-the main group, where complex conservative treatment was carried out, 34-the control group, where traditional treatment was carried out.Thus, out of 89 patients with suprastenotic esophagitis admitted to the clinic from 3 months to 5 years, 47 had mild suprastenotic esophagitis, 25 had moderate and 17 had severe.In the main group of patients with catarrhal esophagitis, esophageal sanitation, laser therapy and bougie were used in parallel, with erosive and erosive ulcerative esophagitis, sanitation and laser therapy are first performed, and oral nutrition was excluded and only after the removal of inflammation and some clinical improvement, bougie was used, and a number of patients had a gastrostomy.The effect of the complex treatment was evaluated upon admission and in dynamics based on the results of a comprehensive examination and indicators such as pain, esophagospasm, dysphagia and the results of microbiological, histomorphological studies, as well as the results of rehabilitation of the suprastenotic expanded site with the determination of sensitivity to antibiotics. As a rule, in the main group of patients, these symptoms weakened or disappeared earlier than in the control group. Thus, in the main group, in the presence of pain associated with inflammation or provoked basing, after 2-4 laser irradiation procedures, pain decreased and general well-being improved. The analgesic and anti-inflammatory effect was clearly manifested not only during preventive bougie, but also during the rehabilitation of the suprastenotic sac. This greatly contributed to the improvement of reparative processes in the stricture zone, since at the same time as the pain decreased, esophagospasm became less frequent or disappeared. As you know, reducing and relieving pain breaks the pathological circle of “pain-spasm-ischemia-pain-spasm". This improves blood supply to inflammatory tissues and creates conditions for epithelial regeneration.As a result of the complex treatment, the effect was achieved in 47 patients, i.e., a severe form of esophagitis (erosive and ulcerative were transferred to catarrhal in only one patient of the main group due to the severe degree of obstruction, a gastrostomy was imposed.he reduction of inflammatory changes in the suprastenotic part of the esophagus was achieved by eliminating oral nutrition and continuing complex therapy. In the control group, where the traditional method of treatment was carried out, a positive effect was achieved in one patient, but this required a longer treatment time than in the main group. It should be noted that three patients of this group with a severe degree of narrowing also had a gastrostomy. It should also be noted that the frequency of severe forms of esophagitis in the control group was 24%, and in the main group the percentage of severe forms exceeded by more than 2 times and amounted to 55%.One of the main risk factors during surgical interventions is an exacerbation of suprastenotic esophagitis. If catarrhal esophagitis is relatively easily stopped during parenteral nutrition and washing of the esophagus with antiseptic solutions, then the treatment of erosive and ulcerative esophagitis is significantly complicated, requires a long time and in some cases gastrostomy is imposed.In addition, prolonged stagnation of the contents in the suprastenotic segment of the esophagus and inflammation significantly change the nature of the microflora. When prescribing antibiotics, we took into account the whole, the age of the patients, the nature and extent of the inflammatory process, the composition and properties of the microflora of the inflammatory focus and its sensitivity to antibiotics. The vast majority of patients received certain antibiotics before admission to the clinic. Of the 52 patients who received antibiotic therapy, 13 used various combinations of drugs.Thus, the microbial landscape in 35 patients with suprastenotic esophageal enlargement and developed esophagitis depended on its severity. The more severe the degree of esophagitis, the more diverse the microflora was and pathogenic forms were more common. After comprehensive treatment, most patients managed to stop the severe degree of esophagitis. Accordingly, changes in the microbial landscape were observed, with a decrease in microbial contamination. The data obtained by us show that after the complex treatment, there was a significant decrease in germinated microbes.Low sensitivity to antibiotics and a relative increase in the number of antibiotic-resistant bacterial strains sown in patients with severe esophagitis were due to the associated action of microflora, individual representatives of which created favorable conditions for each other in the focus of inflammation. This reduces the effectiveness of antibiotic therapy and promotes the development of antibiotic-resistant strains. The pathogenic properties of microbes isolated from patients in the control group were more pronounced than in the main group.Morphological studies have shown that pronounced inflammatory changes occur in the suprastenotic part of the esophagus, affecting all layers of the esophageal wall. In most cases, this is accompanied by the development of erosions and ulcers of the mucous membrane and is sometimes accompanied by sclerotic and atrophic processes. The reason for such changes in the suprastenotic part of the esophagus is a chemical burn of the esophagus with the transition of acute esophagitis to chronic, followed by the development of esophageal stricture and a violation of its evacuation function. These changes in the mucous membrane eventually lead to the appearance of pathogenic flora, which further exacerbates the inflammation process.The complex treatment has an anti-inflammatory effect, improves microcirculation and enhances the regenerative potential of epithelial cells, which contributes to the healing of defects in the mucous membrane of the esophagus.Reconstructive surgery on the esophagus was performed in 72 patients. Only in 37 cases it was possible to restore the patency of the esophagus at the same time.With strictures of the lower, as well as the lower and middle third of the thoracic esophagus, the operation of choice is intrapleural esophagoplasty. Most often, with intrapleural esophagoplasty, the affected part of the esophagus is resected. The advantage of this operation is the removal of the affected esophagus. Unfortunately, in patients with combined burn lesions, it is not always possible to use the stomach as an esophagograft, this is possible only in cases where the lesion of the stomach is limited to a deformation of small curvature. In addition, most patients with this pathology have already operated on the stomach by the time of performing [8] reconstructive surgery on the esophagus, which makes it impossible to use it to replace the esophagus. Therefore, in this group of patients, intrapleural esophagoplasty is performed by the colon.It should be noted that intrapleural colonic plastic surgery is technically more difficult than gastric plastic surgery. And finally, by itself, the opening of the lumen of the colon in the formation of two anastomoses in the abdominal cavity significantly increases the bacterial contamination of the surgical wound and, consequently, the possibility of postoperative purulent complications.It should be noted that intrapleural esophagoplasty with the removal of the affected segment of the esophagus is extremely difficult in patients after esophageal perforation and mediasthenitis. In addition, severe complications are often observed with intrapleural esophagoplasty, such as failure of anastomosis sutures in the pleural cavity, which, as a rule, is the cause of death of the patient.An extended stricture of the esophagus, covering all its thoracic sections, is an indication for total or subtotal plastic surgery of the esophagus with an anastomosis on the neck. The most common operation for such a lesion of the esophagus is retrosternal colon plastic surgery. The esophageal anastomosis is superimposed “side to side”, "end to side". Currently, we use this particular variant of anastomosis, since we consider it necessary to disconnect the esophagus from the passage of food if it is impossible and inexpedient to remove it.In total plastic surgery of the esophagus with the colon, we most often use the thoracic pathway for grafting. It is not traumatic and is justified cosmetically.The surgery of choice in patients with burn lesions of the esophagus should be considered colonic plastic surgery of the esophagus or plastic surgery of the esophagus with stomach and anastomoses on the neck.Comprehensive assessment of the severity of the patient's condition, isolation of a group of patients in order to determine the most specific treatment tactics. The improvement of preoperative preparation of patients, the use of complex therapy in the treatment of suprastenotic esophagitis have significantly improved the results of treatment of this very severe category of patients. The number of complications in patients during treatment decreased by more than 2 times, and there was no mortality, compared to patients who were treated before the use of our proposed methods of preoperative therapy and special training.Surgical intervention in patients with cicatricial narrowing of the esophagus, complicated by suprastenotic esophagitis, is an indication and the most radical, except in cases when surgical intervention cannot be performed due to severe concomitant pathology. Thus, among our patients, combined lesions were detected in 17 patients, which required preliminary surgery to restore patency of the upper gastrointestinal tract.An important role in preventing complications in the postoperative period belongs to the preparation of the suprastenotic department of the esophagus for surgery. The method of conservative treatment of esophagitis used by us made it possible to reduce inflammatory changes in the walls of the esophagus to the level of catarrhal in almost all patients of the main group. A special technique for preparing the colon, cutting out the graft taking into account its blood supply, determining the stage of surgery, the use of high-energy laser radiation for dissecting hollow organs, precision technique for forming esophageal anastomoses on the neck using absorbable suture material contributed to reducing the frequency of immediate postoperative complications in patients of the main group to 6.1% compared with the control group-15.7%.We did not observe insufficiency of esophageal anastomosis sutures in patients of the main group.Thus, the use of an effective comprehensive diagnostic technique and rational treatment tactics, improvement of preoperative preparation of patients have significantly improved the results of treatment of burn pathology of the esophagus. The number of complications in patients decreased by more than 2 times. Improvement of the results of treatment of burn lesions of the esophagus can be achieved in specialized clinics with the use of new achievements of medical science, laser technology, as well as with an individual approach to the choice of reconstructive surgery, taking into account the degree.
4. Conclusions
- 1. Suprastenotic esophagitis occurs in 72.3% of cases and is one of the important factors influencing the course of the postoperative period. The selection of groups of patients according to the severity of esophagitis allows you to choose a rational treatment strategy.2. Morphologically, in the suprastenotic department of the esophagus, there is chronic inflammation of the mucous membrane and submucosal layer with the phenomena of impaired hemopoiesis, edema and fibrosis, and erosive and erosive ulcerative processes were detected in 41.9% of patients. The relationship between the degree of inflammatory changes and the presence of pathogenic microflora has been established: the more severe the esophagitis, the greater the contamination with pathogenic microflora.3. Complex conservative therapy with the proposed method of step-by-step sanitization, including laser therapy, contributes to a faster regression of inflammatory changes in the suprastenotic part of the esophagus, which improves the effectiveness of the surgical intervention.4. Bugging of the esophagus improves its patency, contributes to the resolution of suprastenotic esophagitis, however, it should be carried out taking into account the degree of inflammatory changes in the esophagus, bugging of the esophagus with pronounced inflammatory changes exacerbates these changes and worsens the clinical course of the disease.5. The special preoperative preparation provided by us made it possible to form an anastomosis in the distal part of the expanded esophageal zone, which is the most functionally favorable. It is better to apply an esophageal anastomosis according to the “end to side” type with the disconnection of the distal cicatricially altered esophagus.6. Optimization of medical tactics with the use of complex therapy and various methods of esophagoplasty allowed to reduce the number of postoperative complications by 2 times compared with the control group.Effectiveness of Treatment of suprastenotic esophagitis as prevention of complications of esophageal-intestinal anastomoses.The paper presents the results of treatment of 89 patients. In the main group of patients-55, compared with the control group-34, treatment included step-by-step sanitization, laser therapy with a helium-neon laser, after removal of inflammatory phenomena-esophageal augmentation. 72 patients underwent surgical intervention. A comparative analysis of the results of surgical treatment showed that complications in the main group were two times less than in the control group and amounted to 6.1%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML