-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2490-2493
doi:10.5923/j.ajmms.20241410.08
Received: Sep. 25, 2024; Accepted: Oct. 13, 2024; Published: Oct. 15, 2024

Clinical Evaluation of the Results of Endovideosurgical Operations for Inguinal Hernia
Kamalov N. A., Babazhanov A. S.
Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Analysis of the results of treatment of inguinal hernias using endovideosurgical hernioplasty: TAPP, TEP and e-TEP in 216 patients was carried out. Total extraperitoneal hernioplasty (TER) is preferable for patients who have undergone operations on the abdominal cavity and pelvic organs due to the adhesion process. TARR is recommended when it is necessary to perform simultaneous operations and in case of bilateral localization of hernias. It made it possible to reduce the number of hematomas (in the TARR groups from 8.6% to 3.7%, in the TER-e-TER groups from 7.6% to 5.7%) and seromas (in the TARR groups from 8.6% to 7.4%, in the TER-e-TER groups from 13.5% to 5.7%) with dissection in the preperitoneal space.
Keywords: Inguinal hernia, Endovideosurgical hernioplasty
Cite this paper: Kamalov N. A., Babazhanov A. S., Clinical Evaluation of the Results of Endovideosurgical Operations for Inguinal Hernia, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2490-2493. doi: 10.5923/j.ajmms.20241410.08.
1. Topicality
- A significant number of existing methods of hernia repair has become the basis for a huge number of studies comparing the effectiveness of various techniques. At the moment, however, there is no irreproachable way to perform surgery to remove an inguinal hernia. Tension methods of hernioplasty are losing ground today, and among the non-tension methods using a mesh allograft, endosurgical techniques are gaining the palm, among which TAPP (transabdominal preperitoneal hernia repair) and TEP (totally extraperitoneal hernia repair) surgical interventions stand out favorably [1,3]. Their advantage, in addition to low invasiveness, is that the implant is placed extraperitoneally and, accordingly, does not have contact with the abdominal organs. This sharply reduces the likelihood of the formation of postoperative adhesions and peritoneal adhesions. In the case of the use of TARR, which involves the use of transabdominal access, there is a risk of injury to the abdominal organs during surgery, especially in the case of previous laparotomy. TER is devoid of this drawback, since during the surgical intervention there is no entrance to the abdominal cavity, and all manipulations take place in the preperitoneal space. However, this type of surgical intervention is characterized by a small surgical space, which requires a higher qualification of the operating surgeon [2,6]. Along with this, additional problems during TER may occur in the case of previous prostate surgeries due to the scarring process in the preperitoneal tissue [4,5]. Also, TER is not considered as a surgical treatment of bilateral inguinal hernias. Improvement of the TER technique by J. Daes (2010) was implemented in e-TER (extended totally extraperitoneal hernia repair), which made it possible to perform effective surgical interventions for bilateral, strangulated and inguinal hernias of large sizes.Thus, the variety of endovideosurgical methods of hernioplasty determines the need for their further study in order to form the most favorable surgical method of surgical intervention.Objective. To analyze the results of TARR and TER endovideosurgical hernioplasty to determine the indications and conditions for their implementation and to identify shortcomings.
2. Material and Methods of Research
- The basis of this study is the analysis of the results of treatment of inguinal hernias using endovideosurgical hernioplasty: TARR, TER and e-TER in 216 patients operated in the Department of Endoscopic Surgery of Samarkand GMO No1 for 8 years (2017-2024).All of them were hospitalized for planned surgical treatment. In accordance with the tasks, the patients were divided into 2 groups. Retrospective groups included 110 patients who underwent the following patients: - TARR hernioplasty – 58 patients; - TER hernioplasty – 52 patients.Prospective groups included 106 patients who underwent the following patients: - TARR hernioplasty – 54 patients; - e-TER hernioplasty – 52 patients.Among the patients, men of middle and older age groups prevailed, which is characteristic of inguinal hernias. All hospitalized patients were diagnosed with primary uni- or bilateral inguinal hernias of I, II or III (A or B) types (according to Nyhus). In the retrospective groups, inguinal hernias were most often found in Type II (oblique with an expanded ring) and Type IIIA (straight). At the same time, among those operated using the TARR techniques, there were more patients with complex types of hernias (Type IIIA and Type IIIB). Bilateral hernias (Type IIIA) were observed in 4 (3.6%) patients, and all of them were operated using the TARR technique.This study involved patients who had previously undergone surgical treatment. In the TARR group, these were 10 (17.2%) patients, and in the TER group – 11 (21.2%). The most common is an open-access appendectomy in the right iliac region.In the prospective groups, inguinal hernias of types II and IIIA were most common in 77 (72.6%) patients.From these, more patients with direct hernias (Type IIIA) were operated using the e-TER technique: 40.4% compared to 33.3% among those, who were operated using the TARR technique. At the same time, the group of patients operated using the TARR technique included 3 (4.6%) patients with concomitant cholelithiasis, chronic calculous cholecystitis, who underwent simultaneous surgical interventions: hernioplasty + cholecystectomy. Patients with type IIIB hernias, which included sliding and inguinal-scrotal hernias, were more often operated on by the e-TER method: 17.3% versus 5.6% in the TARR group. Patients hospitalized with bilateral direct hernias (Type IIIA) were also more likely to be operated on by extended full extraperitoneal hernioplasty (5 (9.6%) patients.Patients with an operative history were much more likely operated using the e-TER technique. Thus, among all patients in whom e-TER was used (n=52), 15 (28.8%) had previously undergone abdominal surgery. In the TARR group (n=54), there were 6 such patients (10.1%), and all previous surgical interventions were performed by endovideosurgery. Ultrasound scanning has found its wide use in instrumental diagnostics of PG. The thickness of the oblique abdominal muscles in patients with PG was significantly less in comparison with healthy individuals.
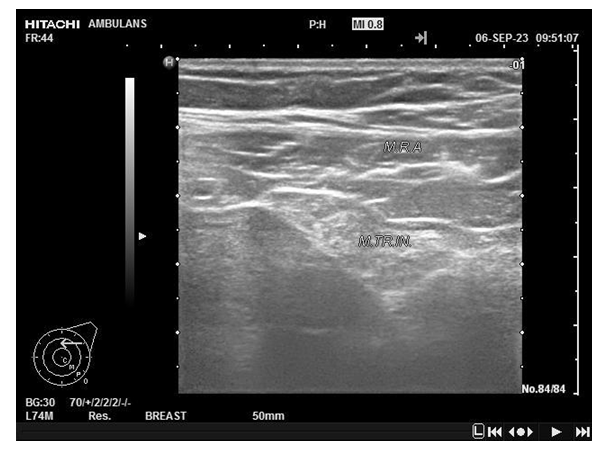 | Figure 1. Criteria for the width of the oblique abdominal muscles (rectus and internal) in patients with inguinal hernia |
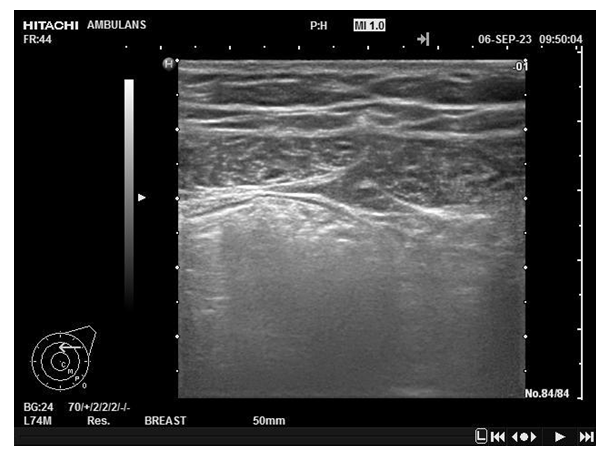 | Figure 2. Ultrasound picture of the muscles of the inguinal region in a patient with inguinal hernia |
3. Results and Discussion
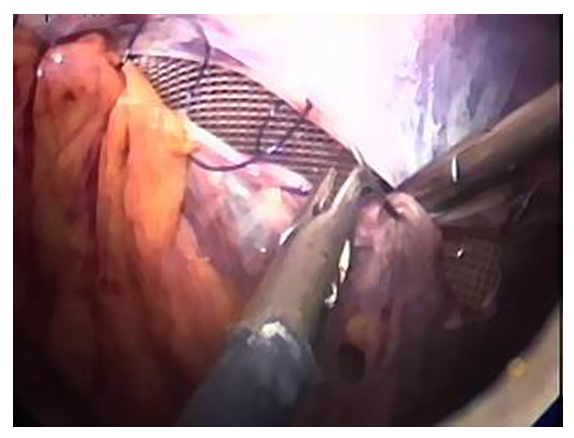
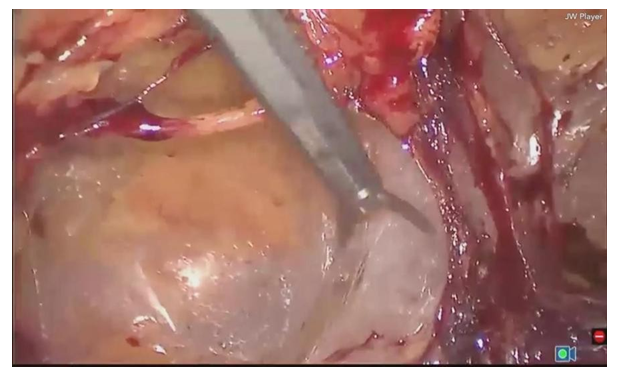
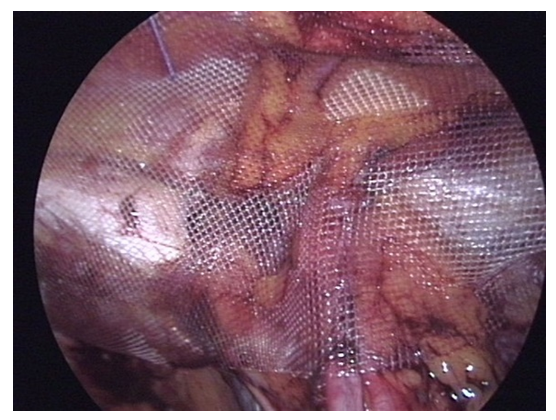
- Analysis of the treatment of patients in retrospective groups showed the following results. The average duration of surgical interventions was 82.3±15.2 minutes with the TARR method, and 79.1±13.4 minutes with the TER method (p>0.05). The total number of complications registered in both groups was 12 (10.9%) cases. Intraoperative complications were more common in the TER group (13.4% versus 8.6% in the TARR group). In the group of patients operated using the TARR technique, in 5.2% of cases, damage to internal organs occurred at the stage of the first trocar placement. All of these patients had previously undergone abdominal surgery. Such a complication was not noted in the TER group, since the technique did not imply entry into the abdominal cavity. The most common intraoperative complication of TER surgery was damage to the parietal peritoneum during dissection in the preperitoneal space. The developed pneumoperitoneum did not allow continuing the operation by the TEP method. Conversion was carried out - the transition to TARR. This option has also been classified as an intraoperative complication. Damage to the epigastric vessels was slightly more common with the TARR technique (3.4% versus 1.9% with TEP).The incidence of postoperative complications did not differ statistically significantly in the TARR and TER groups, amounting to 31.0% and 30.8%, respectively (p>0.05). At the same time, most of the complications did not have significant consequences. Seromas and hematomas in both groups were treated conservatively with a positive effect. In 3 cases, their evacuation by puncture method under ultrasound guidance was required. Mesh migration, which was observed in 2 (3.4%) cases in the TARR group and in 1 (1.9%) case in the TEP group. Long-term results of ECH hernioplasty were traced in 84 (76.4%) patients of retrospective groups. 43 (74.1%) patients after TARR hernioplasty and 41 (78.8%) patients operated on by TER answered the questionnaire. The duration of postoperative follow-up averaged 19.4±3.9 months. Recurrent inguinal hernia was detected in 1 (2.3%) patient from the TARR group and in 1 (2.4%) patient from the TER group. The prospective study is based on treatment outcomes from 106 patients. Of these, 54 patients were operated on using the TARR technique, and 52 using the e-TER technique. The TARR operation was performed under endotracheal anesthesia with mechanical ventilation. The technique of transabdominal preperitoneal hernioplasty pursues the main task of eliminating a hernial defect on the abdominal side, which is achieved by placing a mesh implant on the posterior wall of the inguinal canal, due to which it is strengthened (Fig. 3, 4).
 | Figure 3. Fixation of the mesh endoprosthesis |
 | Figure 4. Final stage. Peritonization of the endoprosthesis |
 | Figure 5. Dissection in the extraperitoneal space |
 | Figure 6. The mesh implant is placed in the preperitoneal space |
4. Findings
- 1. Endovideosurgical transabdominal preperitoneal (TARR) inguinal hernioplasty was accompanied by abdominal organ injuries in 5.2%, which was excluded with total extraperitoneal (e-TER) plasty. However, due to technical difficulties due to space constraints of 3.8%, the TER has been converted to TARR.2. Total extraperitoneal hernioplasty (TER) is preferable in patients who have undergone abdominal and pelvic surgery due to adhesions. TARR is recommended when it is necessary to perform simultaneous operations and in case of bilateral localization of hernias.3. The algorithm for choosing the method of endovideosurgical operations for inguinal hernias, based on taking into account the advantages and disadvantages of TARR and TER, made it possible to achieve a higher level of quality of treatment, made it possible to reduce the number of hematomas (in the TARR groups from 8.6% to 3.7%, in the TER-e-TER groups from 7.6% to 5.7%) and gray (in the TARR groups from 8.6% to 7.4%, in the TER-e-TER groups from 13.5% to 5.7%) in the dissection in the preperitoneal space.4. The incidence of hernia recurrence in the TARR and e-TER groups with a mean postoperative follow-up period of 17.2±3.8 months in TARR was 2.1% with recurrence leveling in e-TER. In the retrospective TARR and TER groups, the incidence of hernia recurrence also did not have significant differences (2.3% and 2.4%, respectively), but it was higher than in the prospective study, which proves the clinical efficacy of endovideosurgical hernia repair of inguinal hernias with a differentiated approach to the choice of surgical method.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML