M. H. Abdulakhatov, D. E. Khoshimov, D. T. Pulatov, G. K. Elmuradov
Republican Scientific Center for Emergency Medical Care, Tashkent, Uzbekistan
Correspondence to: M. H. Abdulakhatov, Republican Scientific Center for Emergency Medical Care, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Objective. Comparative analysis of the results of open and laparoscopic interventions in patients with different forms of acute intestinal obstruction (AIO). Patients. We evaluated the results of surgical treatment of 762 patients with UCN who were divided into 2 groups: 1) primary laparotomy group of 529 (69.4%) patients, 2) group of 233 (30.6%) patients in whom surgical intervention was started with diagnostic laparoscopy. Results. The efficacy of therapeutic laparoscopy for phytobezoars was 75.0%, adhesive intestinal obstruction - 69.3%, small intestinal adhesions - 66.7%, sigmoid intestinal adhesions - 50.0%, intussusception - 40%. In case of single adhesions in the abdominal cavity the efficiency of laparoscopic adhesiolysis was 86.9%, in case of multiple adhesions this index decreased to 32.3%. After laparoscopic adhesiolysis, compared to primary laparotomy, early postoperative complications were significantly less (13,0% vs. 43,5%, p<0,001), it was possible to reduce the period of hospital treatment from 9,31±3,31 to 5,94±1,78 bed-days (p>0,05), total mortality - from 4,9 to 2,6%. Conclusion. The use of laparoscopy in OCN helps to reduce the overall incidence of postoperative complications and decrease the severity of such sequelae.
Keywords:
Acute intestinal obstruction, Adhesion obstruction, Treatment, Videolaparoscopy
Cite this paper: M. H. Abdulakhatov, D. E. Khoshimov, D. T. Pulatov, G. K. Elmuradov, Analysis of the Possibilities of Video Laparoscopy in the Surgical Treatment of Acute Intestinal Obstruction, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2484-2489. doi: 10.5923/j.ajmms.20241410.07.
1. Introduction
The steady increase in the number of operations on abdominal cavity organs and expansion of their volume is naturally accompanied by a progressive increase in the number of patients with acute intestinal obstruction (AIO). This disease is rightly considered one of the most important problems of emergency surgery with the incidence rate of about 5 cases per 100 thousand population. In the United States alone, ICH accounts for more than 30,000 deaths and more than $3 billion in direct medical costs per year. In the United States alone, UCS accounts for more than 30,000 deaths and more than $3 billion in direct medical costs per year. Intestinal obstruction is diagnosed in 15% of patients hospitalized for acute abdomen, and these patients occupy approximately 20% in the structure of emergency surgical interventions [1,2]. According to the Institute of Health and Medical Statistics of the Ministry of Health of the Republic of Uzbekistan, more than 3-3.5 thousand patients are operated annually in the country for acute intestinal obstruction, and postoperative mortality in different years ranges from 5.7 to 7.4% [3].Adhesions, ventral hernias, and neoplasms are the cause of SCI in 90% of cases [4]. In particular, 55-75% of all cases of small intestinal obstruction are due to adhesions [5], while the remaining cases of small intestinal obstruction develop on the basis of hernias and tumors [15]. The cause of small intestinal obstruction in 60% of cases is obstruction of the intestine by a neoplasm [6], in 30% of cases - intestinal tortuosity and diverticulosis [7]; in the remaining 10-15% of cases other pathological conditions are diagnosed (carcinomatosis, endometriosis, scar stenosis of the intestinal segment, etc.).A native abdominal radiograph is usually used as the initial method of examination of patients with suspected OAB. However, this method has rather low accuracy and sensitivity in determining the etiology and level of the lesion, does not provide information about the state of the intestinal wall [8]. In this regard, ultrasound and MSCT are becoming increasingly common in the diagnosis of UCN, which are able to visualize important stigmas of the disease, allowing a more accurate differential diagnosis [9]. However, MSCT has not found widespread and widespread use as an initial and screening method of examination in OCN due to limited availability, high cost, and patient radiation exposure. Ultrasound (USG) is now increasingly used in the diagnosis of OCD, which is characterized by simplicity, accessibility, relative cheapness, non-invasiveness, efficiency and is not associated with radiation exposure, allows to assess intestinal peristalsis in real time [10]. Depending on the level of intestinal obstruction, the sensitivity of the method ranges from 69-98% and is maximum in acute mechanical obstruction of the small and right colon.With regard to the treatment of adhesions, all major international guidelines have long recommended conservative treatment [11,12], as up to 80% of cases of uncomplicated adhesions (in the absence of clinical, radiologic, and ultrasound signs of peritonitis, strangulation obstruction, and intestinal necrosis) are successfully treated with conservative means [13]. Nevertheless, new data show that surgical treatment performed on the first day of hospitalization for the first episode of adhesive UCN can significantly increase the number of quality-adjusted life years [14,15]. Historically, open abdominal adhesiolysis by wide laparotomy has long been the standard method of surgical treatment of adhesive SCI in patients with perforation or bowel necrosis, as well as when conservative treatment was unsuccessful [9,16]. In recent decades, the laparoscopic method of adhesiolysis has been introduced, which contributed to the reduction of the incidence of postoperative complications in patients with adhesive small bowel obstruction. However, the risk of iatrogenic intestinal damage remains higher in laparoscopic surgery of SCI. Therefore, the issues of specifying the indications for laparoscopic surgery and careful selection of patients for this intervention remain open [17,18].Objective. Comparative analysis of the results of open and laparoscopic interventions in patients with different forms of OCN.
2. Material and Methods
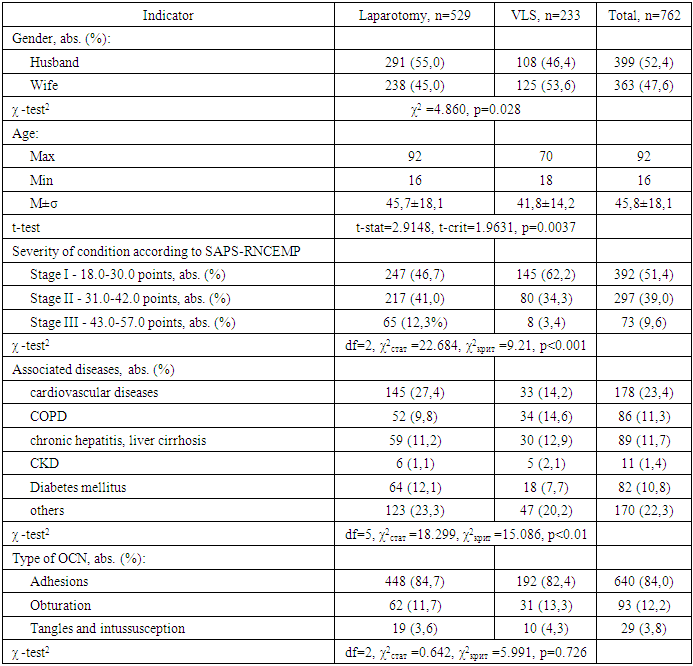
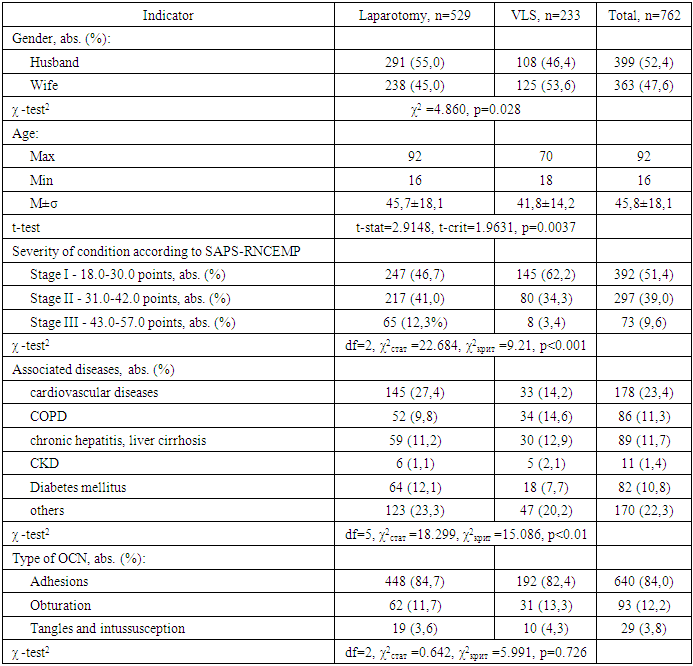
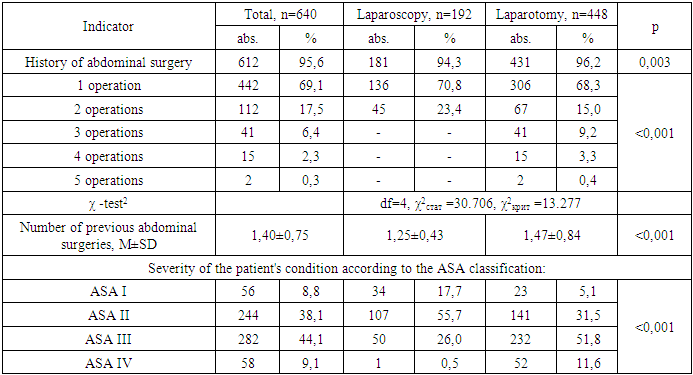
The study design was based on a comparative analysis of the results of open and laparoscopic interventions in 762 patients with various forms of OCD. Depending on the primary surgical aid used, the patients were divided into 2 groups (Table 1): 1) primary laparotomy intervention group, which included 529 (69.4%) patients;2) a group of 233 (30.6%) patients in whom surgical intervention was started with diagnostic laparoscopy. Table 1. Demographic and clinical characteristics of patients with OCN operated by open and laparoscopic methods
 |
| |
|
The male to female ratio in both groups compared was approximately 1:1 (399 (52.4%) males vs. 363 (47.6%) females) with a slight predominance of females in the VLS group and males in the open intervention group (p=0.028).We tried to limit the indications for VLS interventions in patients with severe cardiovascular and other concomitant diseases, and to use them more actively in young patients, whose requirements for cosmetic results of surgical treatment were quite high. Due to the above mentioned circumstances, the average age of patients in the group of VLS interventions was slightly younger - 41,8±14,2 vs. 45,7±18,1 years (p<0.05), and they were also characterized by a lower frequency of concomitant diseases (p<0.01) (Table 1). In addition, more strict selection of patients for laparoscopic interventions was also reflected in the index of severity of the patients' general condition evaluated using SAPS-RNCEMP classification (Table 1). The number of patients in severe condition (43.0-57.0 points) in the VLS-intervention group was only 3.4%, whereas in the group of patients undergoing primary wide laparotomy this index was 12.3% (p<0.001).We tried to use videolaparoscopic technique irrespective of the nature of OCN, and therefore the etiologic structure of the disease in patients of this group was approximately the same as in the laparotomy intervention group (p=0.726) and in the total cohort of patients included in the study (Table 1).
3. Results and Discussion
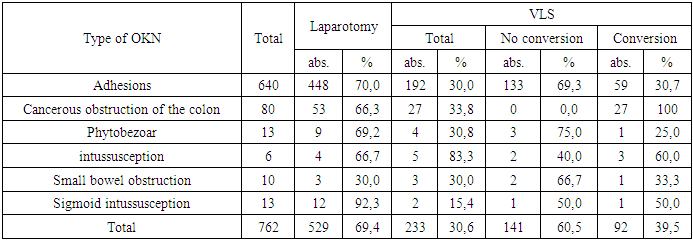
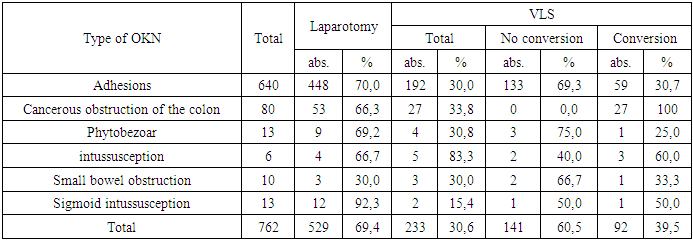
The videolaparoscopic technique at the stages of diagnostics and surgical treatment of various forms of VLS was used in 233 (30.6%) patients included in this study. The overall VLS conversion rate in this category of surgical patients is 39.5% with a range from 25.0% (in phytobezoars) to 100% (in patients with cancerous colon obturation). Video endosurgical interventions for UCN were most effective in patients with phytobezoars (75.0%), adhesive intestinal obstruction (69.3%), small intestine (66.7%) and sigmoid colon (50.0%) ingestion. In addition, in 40% of patients with intussusception, the use of VLS allowed to minimally invasively remove the intestinal obstruction without resorting to wide laparotomy (Table 2).Table 2. Conversion rates during videolaparoscopic interventions in patients with different forms of OCD
 |
| |
|
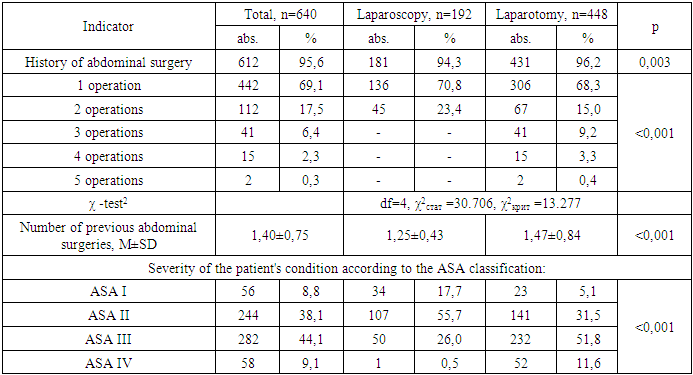
In view of the small number of clinical observations of successful application of VLS in patients with phytobezoars, intussusception and intestinal ingestion, we evaluated the effectiveness of video endosurgical technique in patients with UCN using the example of patients with adhesive intestinal obstruction. As it was mentioned above, 640 patients underwent operations for adhesive intestinal obstruction, of which 448 (70.0%) patients underwent primary laparotomy and 192 (30.0%) underwent VLS (Table 3). Table 3. Clinical characteristics of patients with adhesive intestinal obstruction
 |
| |
|
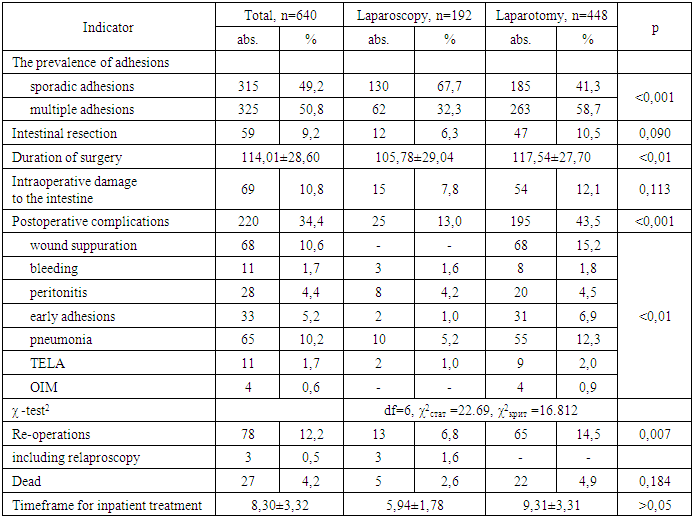
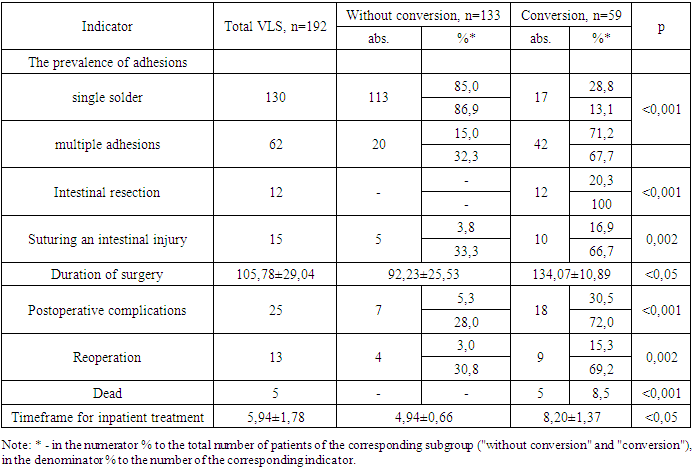
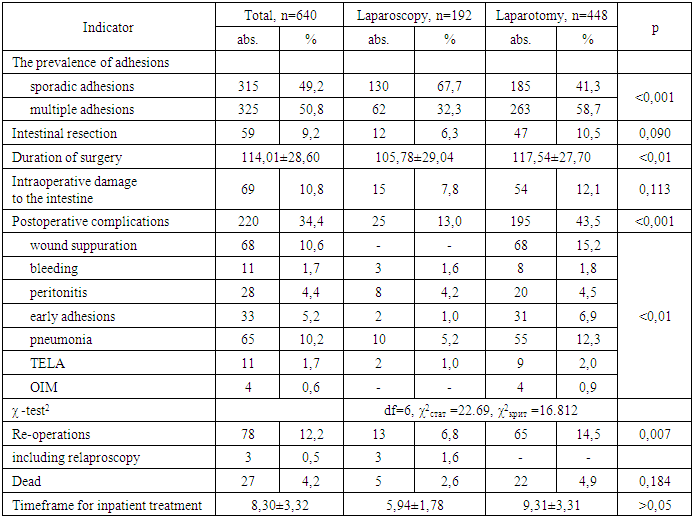
Videolaparoscopic surgeries were tried to be performed in individuals who had previously undergone no more than 2 abdominal operations, whereas in the group of patients undergoing primary wide laparotomy (n=448), the number of patients with a history of more than 2 abdominal penetrations was 58 (12.9%) (p<0.001), including 17 (3.8%) patients admitted with a clinic of adhesive intestinal obstruction after 4 or more abdominal interventions (Table. 3). The mean number of previous abdominal surgeries in the history in the VLS group was 1.25±0.43 and in the laparotomy group was 1.47±0.84 (p<0.001).In addition, VLS interventions were aged to be performed in patients without severe comorbidities; therefore, the physical status of patients was assessed as ASA I and ASA II according to the ASA (American Society of Anesthesiologists) classification in 141 (73.4%) patients of this group. At the same time, in 284 (63.4%) patients undergoing primary laparotomy, the severity of the general condition was evaluated as ASA III and ASA IV (Table 3).The selection of patients for VLS interventions taking into account the presence and number of previous penetrations into the abdominal cavity was statistically significantly reflected in the nature of the adhesion process prevalence (p<0.001) and duration of surgical intervention (p<0.01) in patients of the two compared groups. Thus, in 130 (67.7%) patients undergoing laparoscopic adhesiolysis, the surgeon dealt with single adhesions that caused UCN, whereas in the group of primary wide laparotomy in more than a half of cases - in 263 (58.7%) patients - it was necessary to isolate and dissect multiple adhesions (Table 4). In addition, in patients selected for VLS, intraoperatively, signs of intestinal necrosis requiring conversion and subsequent resection of the necrotized segment were found slightly less frequently (6.3% vs. 10.5%, p=0.090).Table 4. Intraoperative features and results of surgical intervention
 |
| |
|
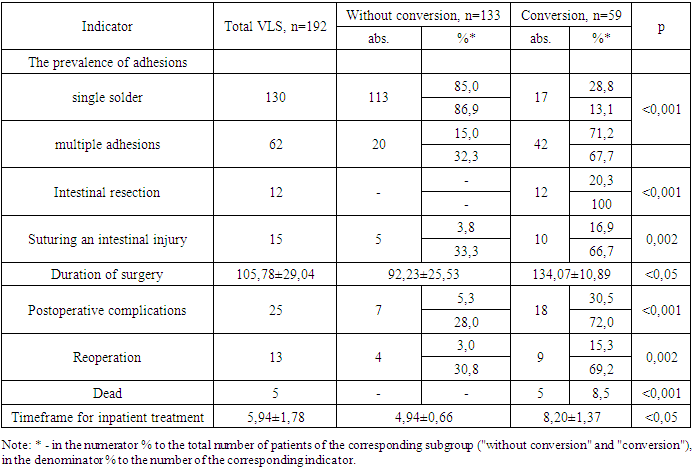
Due to the lower severity of adhesions in patients of the VLS group, the average duration of surgical intervention in them (105.78±29.04 min) was significantly shorter compared to the same indicator of the open intervention group (117.54±27.70 min). The lower prevalence of adhesions in the VLS group was also favorably reflected in the frequency of intraoperative intestinal wall damage (7.8% vs. 12.1% in the primary laparotomy group, p=0.113).After VLS adhesiolysis, statistically significantly (<0.001) fewer early postoperative complications were observed (13.0% vs. 43.5% in the primary laparotomy group). It was observed that specific postoperative complications (wound suppuration, bleeding, peritonitis, and early adhesions) were twice as frequent after open interventions (n=448) compared to nonspecific complications (pneumonia, TELA, and AMI) - 28.3% vs. 15.2%. At the same time, in the VLS intervention group (n=192), the ratio of specific to nonspecific complications was 6.8% vs. 6.3% (13/12). It should be noted that after laparoscopic operations only in 2 (1.0%) cases we observed early adhesion obstruction, whereas after wide laparotomy such complication was noted in 31 (6.9%) patients.All 13 (6.8%) patients in the VLS group who had specific postoperative complications underwent reoperations, including 3 (23.1%) cases in which intra-abdominal complications of the operation were eliminated by relaparoscopy. In the primary wide laparotomy group, the rate of reoperations/relaparotomies was 65 (14.5%) cases (Table 4).The overall mortality rate in patients with adhesive intestinal obstruction was 4.2%, and this rate was statistically insignificantly lower after VLS interventions compared to the primary laparotomy group (2.6% vs. 4.9%, p=184).The use of videolaproscopic access when performing adhesiolysis in patients with adhesive intestinal obstruction contributed to the reduction of inpatient treatment from 9.31±3.31 bed days to 5.94±1.78 days (p>0.05) (Table 4).It is well known that the effectiveness of laparoscopic assistance in the surgical treatment of adhesive intestinal obstruction directly depends on the severity of adhesions in the abdominal cavity. Our observations show that in case of single adhesions in the abdominal cavity, the efficiency of laparoscopic adhesiolysis is 86.9%, whereas in case of multiple adhesions this index decreases to 32.3%. Accordingly, in 42 (67.7%) cases of multiple adhesions (n=62) we had to resort to conversion (Table 5).Table 5. Intraoperative features and results of VLS application
 |
| |
|
If signs of necrosis of the pinched intestinal loop were detected during laparoscopic revision, which occurred in 12 patients, conversion and open intestinal resection were resorted to in all cases. In patients with adhesive intestinal obstruction in the total structure of indications for conversion (n=59) the share of necrosis of the impinged intestine is 20.3% (Table 5).While in cases of intestinal necrosis, the therapeutic possibilities of routine videolaparoscopic instrumentation used in most emergency surgery departments are significantly limited, in cases of intestinal wall damage during laparoscopic adhesiolysis (n=15), the endovideosurgical technique in 33.3% of cases allowed to restore the integrity of the intestinal wall in a minimally invasive manner.The duration of laparoscopic adhesiolysis surgeries lasted an average of 92.23±25.53 min, about 40.8 min shorter than surgeries requiring conversion. The rate of early postoperative complications was also significantly lower in patients in whom adhesiolysis could be performed laparoscopically without conversion (5.3% vs. 30.5%, p<0.001), which was favorably reflected in the reoperation rate (3.0% vs. 15.3%, p=0.002).All 5 cases of death in the group of patients who underwent primary VLS were patients in whom conversion had to be performed because of the severity of the OCD or technical difficulties encountered (Table 5).In addition, the mean hospitalization time in patients with videolaparoscopic adhesiolysis was significantly shorter than that of patients undergoing conversion (4.94±0.66 bed days vs. 8.20±1.37 days, p<0.05).
4. Conclusions
The efficacy of video-endosurgical interventions for phytobezoars is 75.0%, adhesive intestinal obstruction - 69.3%, small intestinal adhesions - 66.7%, sigmoid intestinal adhesions - 50.0%, intussusception - 40%. In case of single adhesions in the abdominal cavity the efficiency of laparoscopic adhesiolysis is 86.9%, in case of multiple adhesions this index decreases to 32.3%. After VLS adhesiolysis, compared to primary laparotomy, early postoperative complications are significantly less (13.0% vs. 43.5%, p<0.001). The incidence of specific and nonspecific postoperative complications after open interventions is 28.3% and 15.2%, and after VLS is 6.8 and 6.3%, respectively. Early adhesion obstruction after laparoscopic operations is noted only in 1.0% of cases, after wide laparotomy - in 6.9% of cases. The application of VLS adhesiolysis in patients with adhesive UCN contributes to the reduction of inpatient treatment time from 9,31±3,31 to 5,94±1,78 bed-days (p>0,05), total mortality - from 4,9 to 2,6%.
References
| [1] | Cappell M.S., Batke M. Mechanical obstruction of the small bowel and colon. Med Clin North Am. 2008; 92(3): 575-597. |
| [2] | Ten Broek R.P.G., Krielen P., Di Saverio S., Coccolini F., Biffl W.L., Ansaloni L., et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018; 13(1): 1-13. |
| [3] | Hajibaev A.M., Hodzhimukhamedova N.A., Hajibaev F.A. Diagnosis and treatment of acute intestinal obstruction. Kazan Medical Journal. 2013; 94(3): 377-381 [Khadjibaev A.M., Hodjimuhamedova N.A., Khadjibaev F.A. Diagnostika i lechenie ostroj kishechnoj neprohodimosti. Kazanskij medicinskij zhurnal. 2013; 94(3): 377-381. In Russian]. |
| [4] | Miller G., Boman J., Shrier I., Gordon P.H.. Etiology of small bowel obstruction. Am J Surg. 2000; 180(1): 33-36. |
| [5] | Ten Broek R.P., Issa Y., van Santbrink E.J., et al. Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ. 2013; 347: f5588. |
| [6] | Frago R., Ramirez E., Millan M., Kreisler E., del Valle E., Biondo S. Current management of acute malignant large bowel obstruction: a systematic review. Am J Surg. 2014; 207(1): 127-138. |
| [7] | Dederer Y.M. Pathogenesis and treatment of acute intestinal obstruction. M Medicine. 1971; 272 [Dederer YU.M. Patogenez i lechenie ostroj neprohodimosti kishechnika. M Medicina. 1971; 272. In Russian]. |
| [8] | Gore R.M., Silvers R.I., Thakrar K.H., Wenzke D.R., Mehta U.K., Newmark G.M., Berlin J.W.. Bowel obstruction. Radiologic Clinics. 2015; 53(6): 1225-1240. |
| [9] | Hollerweger A., Wüstner M., Dirks K. Bowel obstruction: sonographic evaluation. Ultraschall in der Medizin-European Journal of Ultrasound. 2015; 36(03): 216-238. |
| [10] | Boniface K.S., King J.B., LeSaux M.A., Haciski S.C., Shokoohi H. Diagnostic accuracy and time-saving effects of point-of-care ultrasonography in patients with small bowel obstruction: a prospective study. Annals of emergency medicine. 2020; 75(2): 246-256. |
| [11] | Ten Broek R.P., Krielen P., Di Saverio S., Coccolini F., Biffl W.L., Ansaloni L., Velmahos G.C., Sartelli M., Fraga G.P., Kelly M.D., Moore F.A. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World Journal of Emergency Surgery. 2018; 13(1): 1-13. |
| [12] | Maung A.A., Johnson D.C., Piper G.L., Barbosa R.R., Rowell S.E., Bokhari F., Collins J.N., Gordon J.R., Ra J.H., Kerwin A.J.. Evaluation and management of small-bowel obstruction: an Eastern Association for the Surgery of Trauma practice management guideline. Journal of Trauma and Acute Care Surgery. 2012; 73. 5: S362-S369. |
| [13] | Colonna A.L., Byrge N.R., Nelson S.D., Nelson R.E., Hunter M.C., Nirula R. Nonoperative management of adhesive small bowel obstruction: what is the breaking point? Nonoperative management of adhesive small bowel obstruction: what is the break point? The American Journal of Surgery. 2016; 212(6): 1214-1221. |
| [14] | Behman R., Karanicolas P.J., Nathens A., Gomez D.. Hospital-level Variation in the Management and Outcomes of Patients With Adhesive Small Bowel Obstruction: A Population-Based Analysis. Ann Surg. 2021; 274(6): e1063-e1070. doi: 10.1097/SLA.0000000000003739. |
| [15] | Krielen P., van den Beukel B.A., Stommel M.W.J., van Goor H., Strik C., Ten Broek R.P.G. In-hospital costs of an admission for adhesive small bowel obstruction. World J Emerg Surg. 2016; 11: 49. doi: 10.1186/s13017-016-0109-y. |
| [16] | Rami Reddy S.R., Cappell M.S. A systematic review of the clinical presentation, diagnosis, and treatment of small bowel obstruction. Curr Gastroenterol Rep. 2017; 19(6): 28. |
| [17] | Sajid M.S., Khawaja A.H., Sains P., Singh K.K., Baig M.K.. A systematic review comparing laparoscopic vs open adhesiolysis in patients with adhesional small bowel obstruction. Am J Surg. 2016; 212(1): 138-150. |
| [18] | Wiggins T., Markar S.R., Harris A. Laparoscopic adhesiolysis for acute small bowel obstruction: systematic review and pooled analysis. Surg Endosc. 2015; 29(12): 3432–3442. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML