Nurillaeva Khadicha Zhamshidovna1, Kurbaniyazov Zafar Babazhanovich1, Khamidov Obid Abdurakhmonovich2, Nurillaev Khasan Zhamshidovich3
1Doctor of Medical Sciences, Professor, Samarkand State Medical University, Samarkand, Uzbekistan
2PhD, Associate Professor, Samarkand State Medical University, Samarkand, Uzbekistan
3Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The study is based on the results of examination and treatment of 245 patients with postoperative ventral hernias. The choice of the method of hernialloplasty for postoperative ventral hernias should be based not only on the size of the hernial defect, but also on determining the ratio of the hernia volume to the volume of the abdominal cavity according to computed tomography data. The proposed algorithm for treating patients with postoperative ventral hernias based on the criteria for choosing the method of hernialloplasty made it possible to reduce the frequency of postoperative complications from 11.9% to 4.3%, and to level out the development of compartment syndrome and relapse of the disease in the main group, which were observed in the comparison group in 2.4% and 6.3%, respectively.
Keywords:
Postoperative ventral hernia, Computed tomographic hernioabdominometry, Hernioalloplasty
Cite this paper: Nurillaeva Khadicha Zhamshidovna, Kurbaniyazov Zafar Babazhanovich, Khamidov Obid Abdurakhmonovich, Nurillaev Khasan Zhamshidovich, The Role of Computer Tomographic Hernioabdominometry in the Choice of Hernioplasty Method, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2479-2483. doi: 10.5923/j.ajmms.20241410.06.
1. Relevance
According to the World Health Organization, hernias of the anterior abdominal wall are one of the most common surgical diseases, occurring in 3-7% of the population, with a predominant lesion of people of working age [2,3,4,6]. Over 5% of all laparotomies are complicated by the formation of postoperative ventral hernias (POVH), and the frequency of their occurrence depends on the nature and urgency of the surgical intervention. Existing traditional methods of hernioplasty do not always provide an effective treatment result, while the number of relapses varies from 4.3% to 46%, and with extensive defects their frequency can reach up to 60% of cases. In this regard, at present, the priority method of surgical treatment is various options of allohernioplasty, which have significantly improved long-term results [1,5]. However, ongoing developments in this area, the emergence of publications on the need for a differentiated approach to choosing the optimal surgical method, taking into account the background pathology, size and location of hernias and other factors, indicate dissatisfaction with the treatment results for this category of patients and determine the relevance and social significance of this problem [7,8].The aim of the study is to improve the results of surgical treatment of patients with postoperative ventral hernias based on the criteria for choosing the method of hernioalloplasty according to the data of computed tomographic hernioabdominometry.
2. Material and Methods of the Study
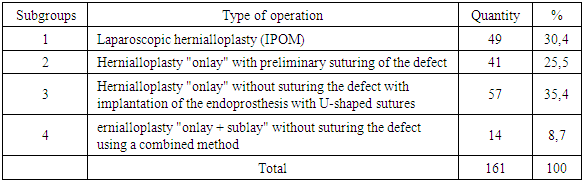
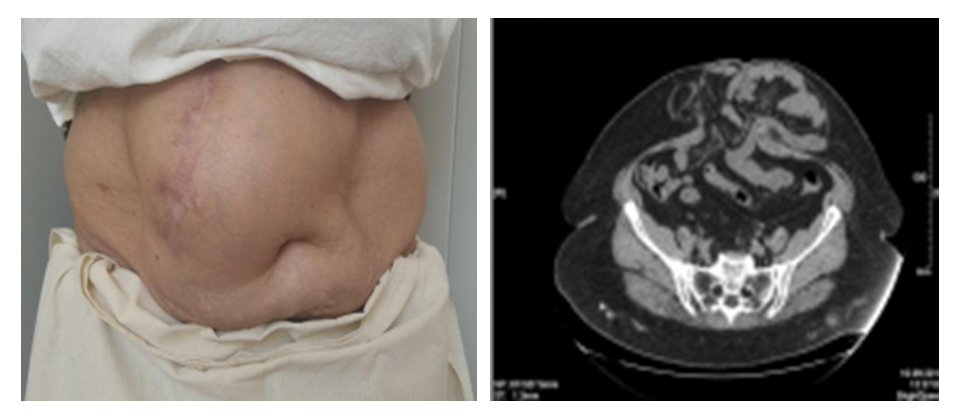
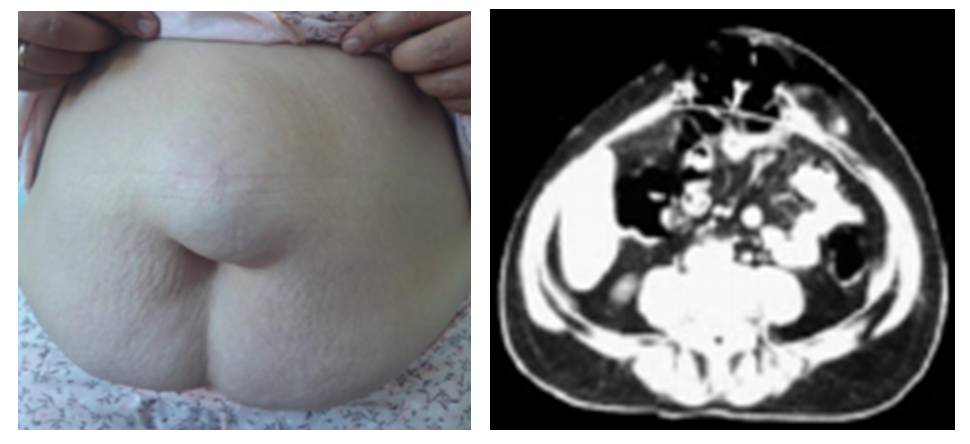
The study is based on the results of examination and treatment of 245 patients with postoperative ventral hernias, who were operated on in the surgical departments of the Samarkand City Medical Association No. 1 and the 1st Clinic of the Samarkand State Medical University in the period from 2018 to 2022. All patients were operated on on a planned basis, and depending on the choice of treatment tactics, the patients were divided into 2 groups. The comparison group consisted of 84 patients operated on in the period 2018-2019, in the treatment of which standard generally accepted approaches were used. The main group consisted of 161 patients who underwent operations in 2020-2022 according to the developed criteria for choosing a hernioalloplasty method.Of the 245 patients, 73 (29.8%) were men, 172 (70.2%) were women.Distribution by age: up to 45 years – 44 (16.8%), 45-59 years – 138 (52.9%), 60-74 years – 56 (21.5%), 75-80 years – 7 (2.7%). In the study groups, 139 (53.3%) patients had uncomplicated forms of hernias and 106 (46.7%) had such a complication as irreducibility. Our study did not include patients with strangulated hernia.According to the classification by Chervel J.P. and Rath A.M. (1999), the vast majority of patients (187 – 76.3%) had midline abdominal hernias – supraumbilical (M1), paraumbilical (M2) and infraumbilical (M3) hernias. The smallest number of patients had lateral (L) 48 (19.6%) and combined (M+L) 10 (4.1%) postoperative ventral hernias. 116 patients (47.3%) had large (W3) and giant (W4) hernias. In 162 (66.2%) they were postoperative (R0), in 83 (41.3%) recurrent postoperative ventral hernias (Rn).When performing CT, attention was paid to the thickness and uniformity of distribution of the subcutaneous fat of the anterior abdominal wall, while assessing the possibility of performing DLE (Fig. 1, 2, 3).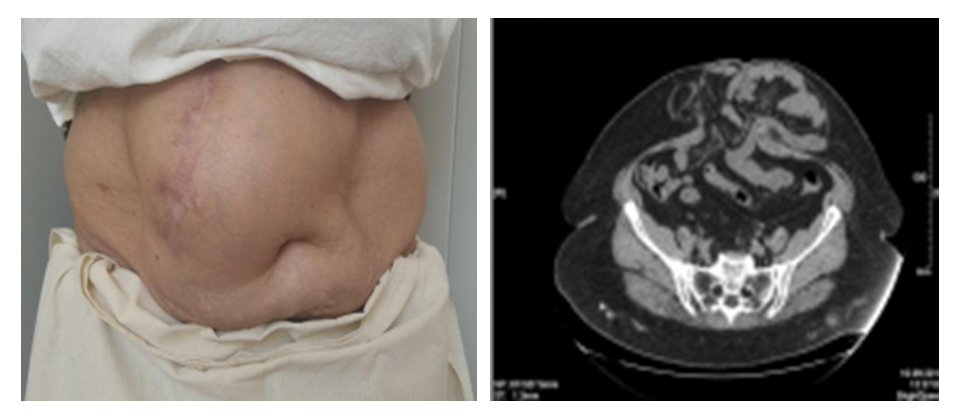 | Figure 1. Patient P., 56 years old, with postoperative ventral hernia (M2W3R0) and computed tomography of the anterior abdominal wall and abdominal cavity |
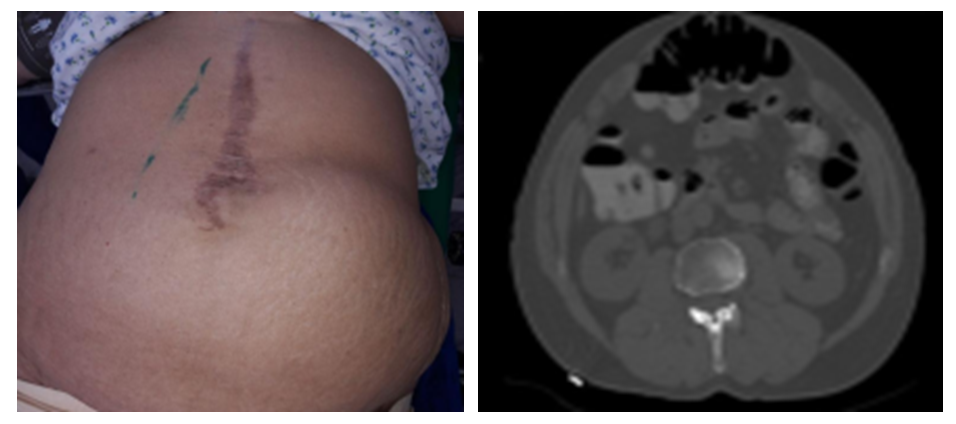
 | Figure 2. View of the anterior abdominal wall and computer hernioabdominometry of patient K., 52 years old, with postoperative ventral hernia (M2W2R0) |
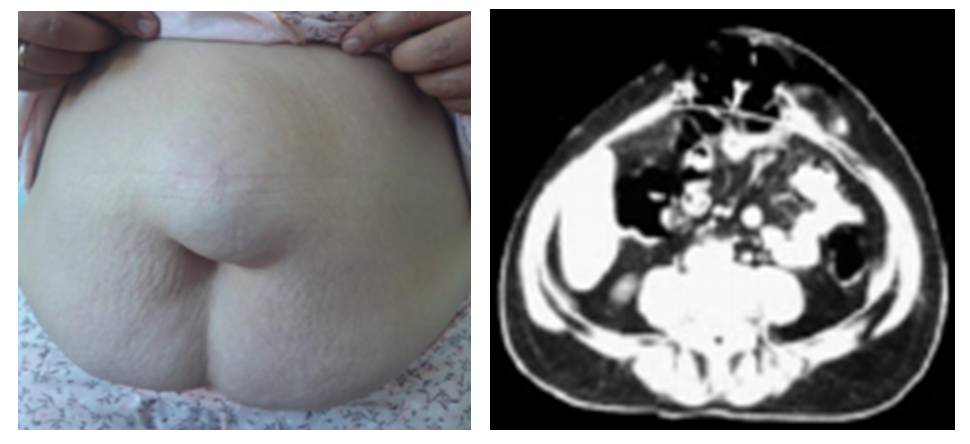
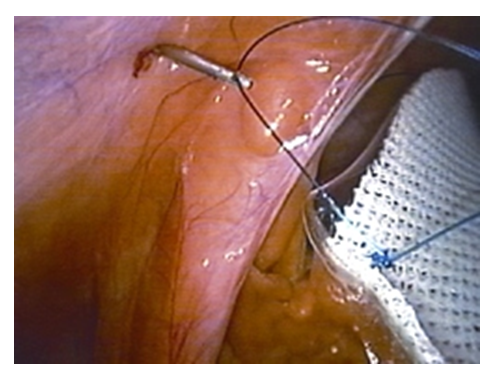
 | Figure 3. View of the anterior abdominal wall and computer hernioabdominometry of patient S., 62 years old, with postoperative ventral hernia (M2W3R0) |
In all patients, a defect in the projection of the hernial protrusion was reliably visualized. In terms of their length, these formations were from 50 to 250 mm, with a width of 50 to 180 mm.In the projection of the hernial orifice, elements of the omentum, loops of the small intestine, as well as the most mobile parts of the large intestine were identified.Adhesions were found between the contents of the hernial sac and its walls. The frame of the anterior abdominal wall in the area of the hernial orifice was thinned, its thickness sometimes reaching 3-4 millimeters (p<0.05). Its main mass was represented by the skin and the parietal peritoneum.Unchanged tissue of m. rectus abdominis of the rectus muscles in 31 (44.9%) patients with postoperative ventral hernia was visualized as homogeneous, the density of its structure was up to 40-50 HU units, more than one centimeter thick, and with clear, even, unchanged contours (p> 0.05). In 38 (55.1%) examined patients, sharp thinning and areas of tissue fraying were observed in m. rectus abdominis (Fig. 2) (p<0.05).A diffuse change in the density of muscle structures was determined, with a decrease in density to 20-30 HU units.Against the background of a diffuse decrease in density, areas of replacement of muscle elements with connective tissue were reliably determined (p<0.05), and the appearance of fatty tissue between groups of muscle fibers of the rectus abdominis muscles was also observed (p<0.05).The size of the hernial orifice was estimated using the formula A/2 × B/2 × 3.14 = cm2, taking the hernial orifice as an ellipse, where A is the largest and B is the smallest diameter of the ellipse. The volume of the hernia and the abdominal cavity with the pelvis was measured using the direct CT method by tracing each section and adding up their results. Since a number of authors (Rodriques A.J., 2003) assume that a hernia is a sphere, its volume was measured using the formula a × b × c × 0.52 = cm3, where a, b, c are the transverse, anteroposterior dimensions and length of the hernia. If the relative volume of the hernial protrusion was less than 5% of the volume of the abdominal cavity, the hernias were considered small.If the relative volume of the hernial protrusion was from 5.1% to 14.0% of the volume of the abdominal cavity, they were considered medium hernias.If the relative volume of hernial protrusion was within 14.1%-18%, the hernia was considered large.If the relative volume of the hernial protrusion from the volume of the abdominal cavity was 18% or more, the hernia was considered giant.Thus, CTGA is the most informative in diagnosing the condition of the tissues of the anterior abdominal wall in patients with postoperative ventral hernia. The use of this technique allows us to obtain a more detailed and clear description of the picture that influenced the change in the topography and structure of the elements of the muscular-aponeurotic framework. The obtained forms of topography violation allowed us to develop rational preparation of the patient before surgery, depending on the size of the hernia, and also to choose the optimal method of hernioplasty individually for each patient.Computer tomography was performed in 69 (42.9%) patients of the main group and was carried out to determine the size of the hernial orifice, the volume of the contents of the hernial sac, identify additional defects of the aponeurosis, identify concomitant pathology of the abdominal organs and topographic changes due to the adhesion process, the thickness and uniformity of the subcutaneous fat of the anterior abdominal wall, as well as for the preliminary determination of the method of hernioalloplasty.
3. Results and Their Discussion
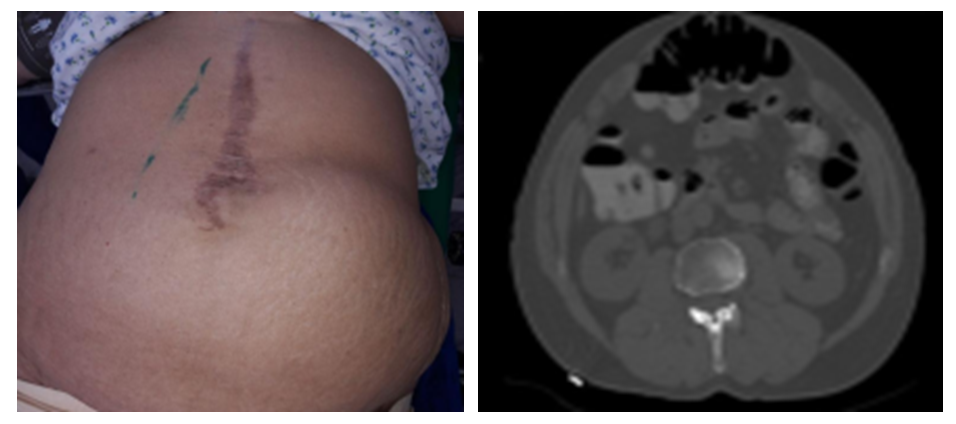
In the comparison group (n=84), hernioalloplasty was performed in 37 patients (44.1%) using tension methods and in 47 patients (55.9%) using non-tension methods.In the main group, the choice of hernioalloplasty was differentiated in accordance with the developed criteria for choosing the method of hernioalloplasty in patients with postoperative ventral hernias (Table 1). Table 1. Types of hernioalloplasty in the main group
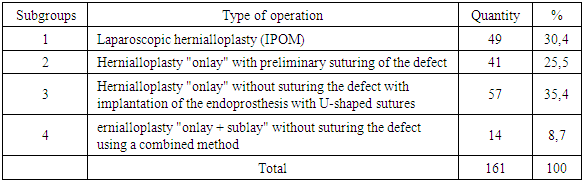 |
| |
|
In patients with a hernial protrusion volume of up to 5% of the abdominal cavity volume according to CT data, laparoscopic hernialloplasty was performed as a priority. With a hernia volume of 5.1% - 14% of the abdominal cavity volume, as well as in case of technical difficulties of laparoscopic surgery, "onlay" hernialloplasty was performed with preliminary suturing of the defect.Laparoscopic prosthetic hernioalloplasty using the IPOM method for postoperative ventral hernias was used by us in 49 patients with small and medium hernias (W1, W2), with corresponding sizes of the aponeurosis defect up to 5 cm and from 5 to 10 cm.Depending on the type of mesh implant, the following surgical interventions were performed in patients of the main group. 37 patients (75.5% of 49 patients who underwent laparoscopic prosthetic hernioplasty) who used standard mesh polypropylene implants. 12 patients (24.5%) used composite mesh implants "Physiomesh" or "Prosid" (Ethicon).Before the implant was inserted into the abdominal cavity, the peritoneum was opened, the hernial sac was isolated and a "pocket" was created in the preperitoneal space, the distance along the perimeter from the hernial orifice was 5-6 cm. Then, a mesh implant rolled into a tube was inserted into the abdominal cavity through a trocar, unfolded and placed in the created preperitoneal "pocket". It was pressed to the anterior abdominal wall using ligatures tied along the edges of the implant. The implant was sutured to the anterior abdominal wall with a thread extracorporeally using an Endo Close needle modified by us (Fig. 4).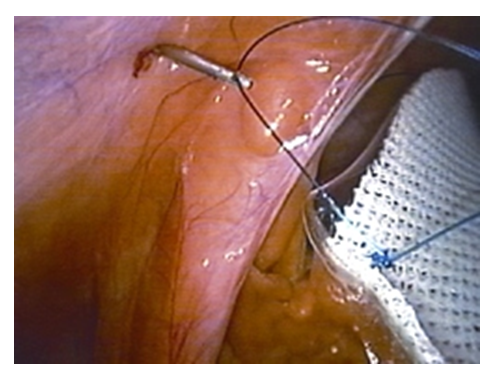 | Figure 4. Removal of suture thread using a modified Endo Close needle (view from the abdominal cavity) |
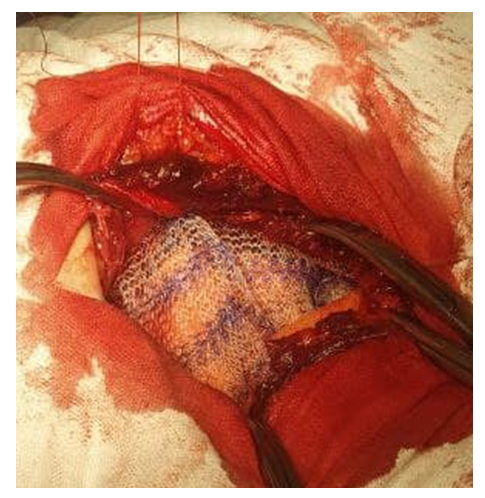
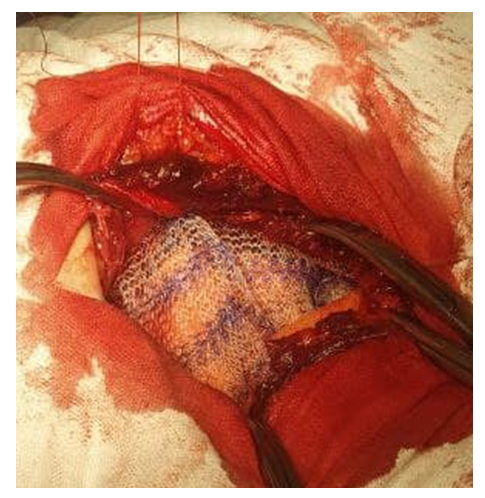 | Figure 5. Fixation of the “sublay” endoprosthesis to the anterior abdominal wall with previously applied U-shaped sutures |
The use of composite mesh implants "Physiomesh" or "Prosid" (Ethicon) in 12 (26.7%) patients made it possible to avoid the need to create a preperitoneal "pocket" before fixing the prosthesis to the anterior abdominal wall.At the same time, 41 patients with a hernial protrusion volume of up to 14% of the abdominal cavity volume according to CT data underwent implantation of an "onlay" endoprosthesis with suturing of the defect. In 6 patients, this type of surgery was continued as a conversion during laparoscopic hernialloplasty.In patients, taking into account CT data with a hernial protrusion volume of more than 14.1% of the abdominal cavity volume, we performed "onlay" hernialloplasty without suturing the defect with implantation of an endoprosthesis with U-shaped sutures in 57 patients. In order to increase the volume of the abdominal cavity, to prevent the development of SAH, after delimiting the abdominal cavity with a hernial sac flap, plastic surgery of the anterior abdominal wall was performed by applying a mesh to the aponeurosis without suturing it. Fixation of the endoprosthesis was performed with U-shaped sutures applied in advance with the capture of all layers of the muscular-aponeurotic wall to the peritoneum. In 14 (17.9%) patients of the main group with a hernial defect size of more than 10 cm and a hernial protrusion volume of more than 18% of the abdominal cavity volume according to CT data, a combined tension-free hernioplasty "onlay + sublay" was performed, i.e. one implant was placed behind the muscular-aponeurotic layer after delimiting the abdominal cavity with a hernial sac flap, the second implant was placed above the aponeurosis. Then the endoprosthesis was placed as a "sublay", previously applied U-shaped sutures were passed through all layers above the aponeurosis and the second endoprosthesis was fixed to these sutures as an "onlay".Also, nodal sutures were applied between the endoprostheses, creating an artificial "white line" of the abdomen. The special significance of this method is the anatomical and physiological reconstruction of the anterior abdominal wall, as well as the white line of the abdomen. The use of this method in the clinic gave a good functional result.To assess the effectiveness of the treatment results for patients with postoperative ventral hernias in the compared groups, the following parameters were used as the main criteria: abdominal complications of the early postoperative period, extra-abdominal complications, wound complications. In 241 patients (98.3%), normal gastrointestinal function was maintained after surgery, only 4 patients (1.6%) (2 patients in each study group) had intestinal paresis, and 2 patients (2.4%) in the comparison group and 2 in the main group (1.2%) had urinary retention. Bronchopulmonary complications were noted in 3 (3.6%) and 4 (2.2%) in the comparison and main groups, respectively. The development of SAH (compartment syndrome) occurred in 2 (2.4%) patients in the comparison group, the patients required long-term mechanical ventilation with breathing training, which was successfully stopped conservatively. Cardiovascular complications were observed in 2 (2.4%) patients in the comparison group. Both respiratory and cardiovascular complications were associated with abdominal compression due to tension hernioplasty.Among the wound complications, postoperative hematomas were noted in 2 (2.4%) and 1 (0.6%) cases, respectively, seromas in 2 (2.4%) and 3 (1.8%) patients, lymphorrhea in 3 (1.2%) patients, in 2 and 1 case in the comparison group and in the main groups, respectively, wound suppuration in 1 (1.2%) patient in the comparison group and necrosis of the edge of the skin flap in 2 (2.4%) and 1 (0.6%) cases. It should be noted that, on average, one patient in the comparison group had 2-3 complications in the form of a combination of bronchopulmonary or cardiovascular with wound complications. In total, the comparison group had 10 (11.9%) patients with various complications, of which 9 (10.7%) had wound complications and 10 (11.9%) had general extra-abdominal complications. In the main group there were 7 patients (4.3%) with various complications, 6 (3.7%) with wound complications and 8 (4.9%) with general complications. According to the comparative indicator for the number of complications, a reliable improvement was obtained in the main group (Criterion χ2 = 4.043; Df = 1; p = 0.045).At the stages of treatment, the level of intra-abdominal pressure was measured dynamically. Based on the data obtained, regular changes in intra-abdominal pressure indicators were identified towards their increase at the stages of the operation associated with the immersion of the hernial contents and hernioplasty using the tension method. Performing tension-free hernioalloplasty with implantation of an endoprosthesis with U-shaped sutures and a combined method of "onlay + sublay" without suturing the defect, used in 71 patients of the main group, made it possible to avoid an increase in intra-abdominal pressure.Thus, the application of the algorithm taking into account the criteria for choosing the method of plastic surgery in the surgical treatment of patients with postoperative ventral hernias made it possible to reduce the overall frequency of postoperative complications from 11.9% to 4.3% (p = 0.045), including wound complications from 10.7% to 3.7% and extra-abdominal complications from 19.1% to 4.9%, and also significantly reduce the duration of surgical treatment, rehabilitation periods and total periods of inpatient treatment after various types of hernioplasty.Remote results were analyzed in 187 (75.9%) of 245 operated patients for periods from 1 year to 5 years. Recurrence of ventral hernia was noted in 5 (6.3%) patients only in the comparison group. Thus, the conducted studies allowed us to draw the following conclusion: the proposed treatment algorithm based on the criteria for choosing the method of hernioalloplasty in patients with postoperative ventral hernias allowed us to reduce the frequency of postoperative complications from 11.9% to 4.3% (p=0.045). Improvement of the technical aspects of performing tension-free methods of hernioalloplasty with implantation of an onlay endoprosthesis using U-shaped sutures and a combined method of onlay+sublay allowed us to level out the recurrence of the disease and improve the quality of life with an increase in the proportion of excellent and good long-term results from 77.7% to 92.1% and a decrease in unsatisfactory outcomes from 8.3% to 1.9% (p=0.030).
4. Conclusions
1. The choice of the method of hernialloplasty for postoperative ventral hernias should be based not only on the size of the hernial defect, but also on determining the ratio of the hernia volume to the volume of the abdominal cavity according to computed tomography data.2. The proposed algorithm for treating patients with postoperative ventral hernias based on the criteria for choosing the method of hernialloplasty made it possible to reduce the frequency of postoperative complications from 11.9% to 4.3%, and to level out the development of compartment syndrome and relapse of the disease in the main group, which were observed in the comparison group in 2.4% and 6.3%, respectively.
References
| [1] | Abduraxmanov D. S. H. et al. Criteria for choosing surgical treatment of patients with ventral hernias and obesity // International Journal of Pharmaceutical Research (09752366). – 2020. – Т. 12. – №. 3. |
| [2] | Abduraxmanov D. et al. Criteria for choosing plastic surgery in patients with postoperative ventral hernias and abdominoptosis //Science and Innovation. – 2022. – Т. 1. – №. 5. – С. 56-61. |
| [3] | Abduraxmanov D. et al. Features of hernioplasty and abdominoplasty in patients with postoperative ventral hernia and abdominoptosis // Science and innovation. – 2022. – Т. 1. – №. 5. – С. 33-40. |
| [4] | Mukhtarov Z. M., Malkov I. S., Alishev O. T. Prevention of wound postoperative complications in patients with postoperative ventral hernias // Practical Medicine. - 2014. - No. 5 (81). |
| [5] | Teshaev O. R., Khaitov I. B. Experimental modeling of anterior abdominal wall hernia with abdominovisceral obesity // Journal of Theoretical and Clinical Medicine. - 2016. - No. 4. - P. 23-25. |
| [6] | Baylón K. et al. Past, present and future of surgical meshes: a review // Membranes. - 2017. - Vol. 7. - No. 3. - P. 47. |
| [7] | Berrevoet F. et al. A multicenter prospective study of patients undergoing open ventral hernia repair with intraperitoneal positioning using the monofilament polyester composite ventral patch: interim results of the PANACEA study // Medical devices (Auckland, NZ). – 2017. – T. 10. – P. 81. |
| [8] | Elstner K. E. et al. Preoperative progressive pneumoperitoneum complementing chemical component relaxation in complex ventral hernia repair // Surgical endoscopy. – 2017. – T. 31. – No. 4. – S. 1914-1922. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML