-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(10): 2453-2457
doi:10.5923/j.ajmms.20241410.01
Received: Aug. 3, 2024; Accepted: Sep. 1, 2024; Published: Oct. 11, 2024

Inguinal Hernia: Prevalence, Risks, Treatment Prospects
Khalikov S. P., Khusinov D. O., Yakubov O. E., Elmuratov I. U.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article notes various methods of surgical treatment of inguinal hernia, including open and laparoscopic access. Each method has its advantages and disadvantages, and the selection choice depends on the individual characteristics of the patient and the experience of the surgeon.
Keywords: Transabdominal preperitoneal (TAPP), Totally extraperitoneal (TER), Natural orifice transluminal endoscopic surgery (NOTES)
Cite this paper: Khalikov S. P., Khusinov D. O., Yakubov O. E., Elmuratov I. U., Inguinal Hernia: Prevalence, Risks, Treatment Prospects, American Journal of Medicine and Medical Sciences, Vol. 14 No. 10, 2024, pp. 2453-2457. doi: 10.5923/j.ajmms.20241410.01.
Article Outline
1. Introduction
- Inguinal hernia accounts for 75% of all hernias of the anterior abdominal wall, and the risk of development throughout life is observed in 32% of men and 3% of women. Oblique (external) inguinal hernias outnumber direct (internal) inguinal hernias in approximately a 2:1 ratio. The incidence of the most common surgical pathology has two risk periods of development, at the age of 16-24 years (110 patients per 100,000 population) and 65 years and older (2,000 per 100,000 population). The incidence of inguinal hernia increases with age and the average age at diagnosis is 40-59 years [1,3,6].Even though women suffer much less from inguinal hernia, they have risk factors for the development of this pathology, which is especially evident during pregnancy and childbirth, but this does not account for a large percentage of occurrence (0.1%). In the pediatric population, the incidence of inguinal hernia in children is 1-5% and is even higher in premature infants, reaching 10-30% [7,10].Among all surgical interventions, hernia repair is one of the most common both in the world and in the Republic of Uzbekistan. About 250,000 surgical interventions for various hernias are performed annually in the country. The number of operations for this pathology in Russia reaches 400,000 per year. According to US statistics, more than 1 million operations are performed annually to repair hernias of the anterior abdominal wall, of which about 750,000 operations are for inguinal hernia [1,22].The history of inguinal hernia dates back to 1550 BC when the earliest evidence of inguinal hernia appeared in ancient Egypt. The surgical history of hernias, having centuries of experience, was limited to ligation of the neck of the hernial sac, followed by amputation of the testicle, or cauterization of the hernia, which later also ended in the removal of the egg [2,5].With the advent of anatomical history, radical treatment of hernias using surgical interventions began to develop rapidly. Not every anatomical structure or human organ can boast of having names named after a specialist. F. Poupart (1661-1709) – Poupart's ligament (inguinal), P. Camper (1722-1789) – Camper's fascia, A. Scarpa (1752-1832) – Scarpa's fascia, C. Amyand (1660-1749) – Amyand's hernia, A.P Cooper (1768-1841) – Cooper’s ligaments, F.K Hesselbach (1759-1816) – Hesselbach’s triangle [4,7].The first report of successful transabdominal plastic surgery was described in 1716 by Demetrius Cantemir (1673-1723). Henry O. Marcy (1837-1924) stated that failure to close the internal inguinal ring or low ligation of the hernial sac could lead to recurrence, thereby describing the technique of reconstruction that was the first to use high ligation of the hernial sac and closure of the inguinal ring. Bassini described the anatomy of the anterior inguinal canal and introduced safe and effective surgery into the modern era by introducing the Bassini procedure in 1887. Subsequently, William S. Halstead (1852-1922) and Edmund Andrews (1824-1904) modified Bassini's repair. Modified Bassini repair (North American Bassini plasty) has been used throughout the world, although it has a high recurrence rate. Chester McVay (1911-1987) pioneered the use of the Cooper ligament repair of the inguinal canal in 1939. In 1919, Georges La Roque (1876-1934) used abdominal and skin incisions and then ligated a hernial sac that had been pulled in from the abdominal cavity. In 1936, Arnold Henry (1886-1962) developed a similar approach using a midline incision in the lower abdomen. In 1920, George Lenthal (1865-1951) pioneered the use of the total extraperitoneal approach as a radical surgical procedure for both inguinal and femoral hernias, using an inferomedial preperitoneal approach. By the concept of the preperitoneal approach, in 1959, Lloyd M. Nyhus (1923-2008) proposed reconstruction of the iliopubic tract. Subsequently, based on this concept of preperitoneal access, prosthetic reinforcement for unilateral hernias was first described in 1965 by Jean Reeves (1873-1985) and in 1969 by René Stoppa (1921-2006) for bilateral inguinal hernias [2,4,5,7].In 1986, Irving Lichtenstein (1920-2000) first introduced a Mesh Plug made by twisting a piece of flat polypropylene into a cigarette shape to fill a femur defect. The mesh was fixed with interrupted sutures; this “cigarette” plug was used to repair inguinal, femoral, and recurrent hernias. Thus, Lichtenstein created a tension-free technique that ushered in a new era of surgery. Classic hernia repair used sutures under tension, which led to a high recurrence rate. This technique significantly reduced the frequency of relapses and infections, and as a result, it became preferred and spread throughout the world [23].Since the second half of the 20th century, prosthetic mesh has been routinely used in practical surgery by the concept of tension-free plastic surgery.Laparoscopic transabdominal preperitoneal (TAPP) repair is based on the same principle (transperitoneal approach for inguinal hernia) as the technique published by Lawson Tait (1845-1899) in 1891. In 1979, P. Fletcher first used a laparoscope to repair an inguinal hernia. Subsequently, Ralph Gehr in 1982, S. Bogoyavalensky in 1989, Leonard Schultz in 1990, and Maurice E. Arregui in 1992 published their experience with hernioplasty using the TAPP technique [21,23].The first to use the term "totally extraperitoneal" was Edward Phillips in 1993. TEP – totally extraperitoneal - without entering the free abdominal cavity, using endoscopic technology, the preperitoneal space is cut out, with the installation of a synthetic prosthesis to strengthen the groin area. Almost at the same time, similar reports on hernioplasty using the TEP technique were published by G. Ferzli (1992), J. Himpens (1992), J. Barry McKernan and H. Laws (1993) [18,19].Transluminal endoscopic surgery through natural orifices - (Natural orifice transluminal endoscopic surgery (NOTES)) - continues to be studied as a future option for general surgery. Panait et al reported on 107 patients who underwent transvaginal appendectomy, cholecystectomy, and ventral hernia repair. Proponents of this approach claim potential cosmetic benefits, reduced postoperative pain, early return to daily activities, reduced port site complications, and specific benefits in obese individuals. However, most agree that NOTES hernia repair procedures increase the risk of severe complications, and these techniques should be strictly considered experimental at this time and performed according to institutional research protocols [15,24].Robotic technology in general surgery has become increasingly popular since G. Himpens and G. Cadiere presented the first robotic cholecystectomy on a 72-year-old obese patient using the da Vinci surgical system. The da Vinci Surgical System, a product of Intuitive Surgical, Inc. (Sunnyvale, California, USA), was approved by the US Food and Drug Administration (FDA) in 2000 and its use has expanded since then. The first inguinal hernia repair using robotic access dates back to 2007. Since then, there has been growing interest in using a robotic platform to repair abdominal wall defects [15,20,24].Modern surgery of inguinal hernias has been supplemented with high-tech minimally invasive interventions. The practicing surgeon can now choose from several types of approaches (open or laparoscopic, anterior or preperitoneal), choose the layer of placement of the mesh implant (on the transverse fascia or preperitoneal space), types of methods for fixing the prosthesis to the surface of the small pelvis (suture, without suture, Velcro, adhesive), with a varied selection of flaps of synthetic material to strengthen the groin area (soft or hard, sheet or three-dimensional).
2. Methods for Diagnosing Inguinal Hernias
- In 95% of patients with suspected inguinal hernia, a general practitioner or surgeon can diagnose the disease based on the clinical picture and physical examination. If doubts are identified when setting a tactic, a specialist may prescribe imaging studies, such as abdominal ultrasound, and X-ray methods (MSCT or MRI) [3,12].Laboratory tests are not specific to the evaluation of patients with inguinal hernias but may be useful for general medical assessment.A CT scan of the abdomen and pelvis can help detect many hidden hernias, demonstrating separate locations of the bowel, bladder, or female internal reproductive organs. MSCT is indicated for the diagnosis of obturator or doubtful hernia, as well as in cases where it is necessary to differentiate the hernia from formations of the abdominal wall (tumors, hematomas, abscesses, aneurysms, undescended testicle). When the patient’s appearance makes it difficult for the doctor to perform a high-quality physical examination, it is also necessary to use this diagnostic method [6,10].Several scientific studies have been conducted to compare the roles of ultrasound, MRI, and CT in the diagnosis of inguinal hernias, to determine which diagnostic method is most accurate in identifying the disease. Experts concluded that ultrasound has the highest sensitivity and specificity compared to CT and MRI. Ultrasound: sensitivity – 87%, specificity – 100%; CT: sensitivity – 73%, specificity – 63%; MRI: sensitivity - 93%, specificity - 95% [8,10].The estimated positive predictive value of ultrasound was 90.9%, which indicates a high frequency of predicting surgically significant inguinal hernia. For this purpose, it is necessary to adhere to the following points of the standard template: the position of the patient during the examination, the use of the Valsalva maneuver (+ or -), the size of the gate and the hernia itself, the nature of the contents of the sac [3,11].Radiation diagnostic methods are used as additional tools and allow one to obtain a complete picture of an inguinal hernia. Based on this, it is recommended to adhere to the protocol for performing radiation methods of the anterior abdominal wall for instrumental differentiated diagnosis of inguinal hernias.
3. Classifications of Inguinal Hernias
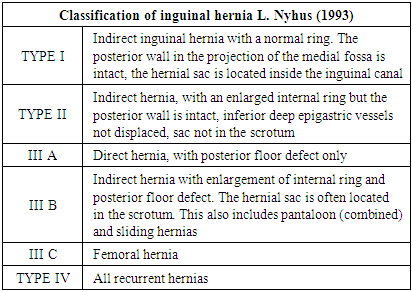
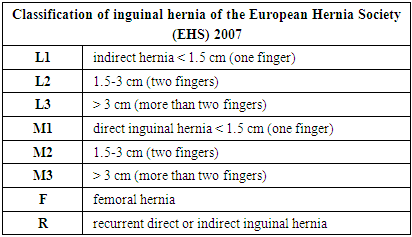
- The classification of inguinal hernia is a necessary tool for the surgeon when making the right choice of surgical intervention in each case. Many generations have contributed to changes in the classification of hernias, so it should not be considered a solid construct, since it reflects the development of hernia surgery. Each proposed classification is an individual opinion or vision of a specialist when approaching a given pathology.The inguinal hernia was classified according to three functional structures (transversalis fascia, aponeurosis of the external oblique muscle, and iliopectineal ligament (Cooper)) in 1967 by Kasten.Halverson and McVay in 1970 proposed four classes of hernia: small indirect inguinal hernia, medium indirect inguinal hernia, large indirect and direct inguinal hernia, and femoral hernia [9,17].In 1989, Gilbert published his vision based on anatomical and functional defects identified intraoperatively: the presence or absence of a peritoneal sac, the size of the internal ring, and the integrity of the posterior wall. Rutkov and Robbins (1993) modified this classification and added combined direct and indirect hernia and femoral hernia [14,16].Niehus (1991) used internal ring size and posterior wall integrity to define anatomical criteria. Continuing this idea, to measure the diameter of the hernial orifice, it was proposed to determine the size using the fingers, 1 finger - 1st degree, 2 fingers - the second, if 3 fingers or more fit in the hernial orifice, the hernia is considered large (Aachen classification, 1995). In 2003, Zollinger presented a modified version of the traditional classification of inguinal hernias, which included all classes or degrees proposed by Niehus and Stoppa, Gilbert, and Schumpelik [9,13].A special classification dedicated to recurrent inguinal hernias was proposed by Zhebrovsky (2005), which was based on the localization of the exit of the hernial sac, and subsequently modified according to the degree of complexity (2007). The works of Campanelli (2006) and Ostrovsky (2010) were devoted to the same direction.The classification of inguinal hernias helps the specialist in the correct choice of surgical treatment method. When examining a patient with an inguinal hernia, a specialist first of all determines the size of the hernia, large or small, since surgical tactics for large hernias change dramatically, it is necessary to perform an open intervention instead of a minimally invasive one, and given the presence of laparoscopic technology in the surgeon’s arsenal, minimally invasive interventions should prevail.Today, the Niehus classification (1993) is widely used, which has 3 types and is used throughout the world. However, it is not without its drawbacks; in particular, it does not take into account factors such as reducible or irreducible hernia, and congenital and bilateral hernias. Also, this classification is based on indications for an open (anterior) approach (Table 1).
|
|
4. Conclusions
- The article addresses the problem of inguinal hernia, which is the most common surgical pathology. Inguinal hernia accounts for 75% of all hernias of the anterior abdominal wall, with indirect (external) hernias outnumbering direct (internal) ones in a ratio of 2:1.The risk of developing an inguinal hernia is related to gender and age. In men, the risk is 32%, and in women it is 3%. The incidence of inguinal hernia has two risk periods of development: from 16 to 24 years and after 65 years. The average age at diagnosis is 40-59 years.The article also notes that women, although they suffer from inguinal hernia less often, have risk factors for developing the pathology, especially during pregnancy and childbirth. In children, the incidence of inguinal hernia is 1-5%, and among premature babies, it can reach 10-30%.Hernia repair is one of the most common surgical procedures both in the world and in various countries. In Russia, about 400,000 operations for inguinal hernia are performed annually.The history of hernia repair began long before our era, and with the advent of wide polymer plastic meshes at the end of the 20th century, significant progress in the surgical treatment of inguinal hernia occurred. These meshes have made it possible to reduce relapses after surgery and improve the prognosis of patients.The article notes the various methods of surgical treatment of inguinal hernia, including open and laparoscopic approaches. Each method has its advantages and disadvantages, and the choice is made depending on the individual patient and the experience of the surgeon.To summarize, the need for early diagnosis and treatment of inguinal hernia should be emphasized to prevent complications and improve the quality of life of patients. Surgical treatment using polymer plastic meshes is considered the most effective and safe treatment method, which allows for achieving good results and minimal risk of relapse.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML