-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2441-2444
doi:10.5923/j.ajmms.20241409.68
Received: Aug. 21, 2024; Accepted: Sep. 19, 2024; Published: Sep. 30, 2024

Clinical Evaluation of the Effectiveness of Various Maloinvasive Methods in the Diagnosis and Treatment of Central Serous Chorioretinopathy
Jamalova Sh. A.1, Ibodullaeva D. Ch.1, Aktamov A. Sh.2
1Republic Specialized Eye Microsurgery Scientific-Practical Medical Center, Uzbekistan
2Sihat Ko‘z LLC Clinic, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The use of various noninvasive examination methods in the diagnosis of central serous chorioretinopathy (CSCR) and evaluation of the effectiveness of treatment of various forms of the disease using subthreshold microimpulse laser therapy. Materials and methods. 64 patients with CSCR (68 eyes) were examined at the Republican Specialized Scientific and Practical Medical Center for Eye Microsurgery. 22 of the total number of patients (25 eyes) were 34.37 percent with chronic form, 30 (46.8%) with acute form, and the control group was 12 (18.75%) with acute form. Results. Positive changes began to be observed in patients 1 month after treatment. At the initial examination, 65.6% of patients showed an increase in visual acuity from 0,46±0,052 to 0,81±0,075 and 46.8% (30 eyes) of patients showed complete resorption of subretinal fluid. Conclusion. The results of the examination and observations showed the effectiveness of subthreshold micro-pulse laser exposure with a yellow wavelength (577 nm) in the treatment of various forms of CSCR disease. Key words: central serous chorioretinopathy, subthreshold microimpulse laser therapy, fluorescent angiography, autofluorescence, neuroepithelial detachment.
Keywords: Chorioretinopathy, Microimpulse, Subretinal fluid, Autofluorescence, Neuroepithelial detachment
Cite this paper: Jamalova Sh. A., Ibodullaeva D. Ch., Aktamov A. Sh., Clinical Evaluation of the Effectiveness of Various Maloinvasive Methods in the Diagnosis and Treatment of Central Serous Chorioretinopathy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2441-2444. doi: 10.5923/j.ajmms.20241409.68.
1. Introduction
- Central serous chorioretinopathy (CSCR) occurs mainly in people of working age (39–51 years old) with increased choriocapillary permeability, pigment epithelium (PE) dysfunction, retinal neuron (NE) or pigment epithelium serous detachment, fluid secretion into the subretinal space, etc. It is a disease with changes [5].The disease is characterized by decreased visual acuity, macropsia, and changes in color sensitivity, including acute forms that resolve spontaneously in 80% of cases and chronic forms with the appearance of prolonged neuroepithelial detachment and foci of diffuse atrophy of PE in combination with the above complaints [1,9]. Currently, early diagnosis of clinical changes occurring in CSCR is the main factor in achieving complete regression of the disease against the background of conservative treatment and preventing its transition to a chronic form. It is possible to use several scanning programs of OCT in the differential diagnosis of different forms of CSCR and in determining the filtration point (FP) identified in fluorescence angiography (FAF) in the acute form of CSCR, which corresponds to the defect point in the retinal pigment epithelium [3,6]. In addition, it is possible to determine the damaged area of PE, which is considered the source of FP, using autofluorescence (AF) [2]. Autofluorescence is manifested in the form of foci in the form of increased (hyperautofluorescence) or decreased (gpoautofluorescence) autofluorescence intensity of the area where the retinal neuroepithelium has migrated and the filtration point [7]. In the treatment of acute and chronic types of the disease, the use of laser devices of different wavelengths has been effective to date. Among them, subthreshold micropulse laser therapy is now widely used in the treatment of various forms of CSCR [4,8]. The main effect of subthreshold micropulse laser therapy involves the transmission of energy in the form of successive very short picosecond pulses. This, in turn, causes a certain amount of temperature increase in the cells, and the state of coagulation does not occur. It prevents tissue-destructive temperature increases and reduces the harmful effects of lasers. The use of this type of laser avoids complications that may occur as a result of focal laser coagulation (FLC). Alternatively, the fact that the FP is located in the parafoveolar or foveolar area is also a solution to another problem. It is also worth noting that the ability to use it several times in cases of recurrence and chronic forms of the disease further increases the effectiveness of this method of treatment.Purpose of the investigation. The use of various non-invasive examination methods in the diagnosis of central serous chorioretinopathy and the evaluation of the effectiveness of subthreshold micropulse laser therapy for various forms of the disease.
2. Materials and Methods
- We examined 64 patients (67 eyes) with CSCR who were referred to the Republican Specialized Scientific and Practical Medical Center for Eye Microsurgery. The average age of 24 women is 35.6 ± 3.4 years, and the average age of 40 men is 40.2 ± 5.1 years. Of the total patients, 22 (25 eyes) with 34.37% chronic form, 30 (30 eyes) with 46.8% acute form, and 12 (12 eyes) with 18.75% acute form were included in the control group received. Patients who received anti-VEGF injections, photodynamic therapy (PDT), and patients with choroidal neovascularization were not included in the scope of the investigation. All patients underwent standard and additional examinations. In the FA examination, 10% 5ml fluorescein sodium is sent into the vein and the picture is taken. The examination is carried out several times over a certain period of time, starting from the time when the dye deposit in the fundus of the eye comes out of the vein. All patients were examined by optical coherence tomography (OCT) and optical coherence tomography + angiography (OCT-A) using DRI OCT Triton Plus (Topcon, with Swept Source technology) Line and 3D-reference scanning protocols. The height of the detached area of the retinal neuroepithelium was measured from the internal limiting membrane to the pigment epithelium, and in cases where PE detachment was present, from the Bruch's membrane to the inner border of the pigment epithelial cells. The thickness of the vascular layer included the distance from the center of the fovea, from Bruch's membrane to the area of the choriscleral junction. Filtration points detected by FAG were studied using different OCT scanning protocols. When a 3D-reference scan was performed and the pigment epithelium was analyzed in En Face mode, PE detached zones were expressed as hyporeflective (black) dots. A line scan showed morphological changes in pigment epithelial cells (fragmentation of cells) and photoreceptors (partial destruction of outer segments) in the projection of filtration points. The therapeutic effect of the laser was carried out in the subthreshold micropulse mode of the "Easy Ret Quantal Medical" (France) laser device at the wavelength of yellow (577 nm). For the purpose of testing, laser applications were conducted in the micropulse mode in the area of the retina near the arcade away from the affected area, and the indications of the laser were: the diameter of the laser spot is 160 microns, the pulse duration is 0.2 s, the packet duration is 100 ms, the duty cycle is 5%, and the power is selected individually for each patient and increased every 100 mW until an almost visible tissue reaction is formed. After the laser power is selected, it is reduced by 50%. Using the indicators selected as a result of the test, a laser is applied to the area of serous migration of PE or NE and the hyperfluorescence area detected on FA. Thus, the hyperfluorescent surface is made in the form of a "layer" densely placed next to each other, and the serous detached area is made in the form of a "grid".
3. Results and Discussion
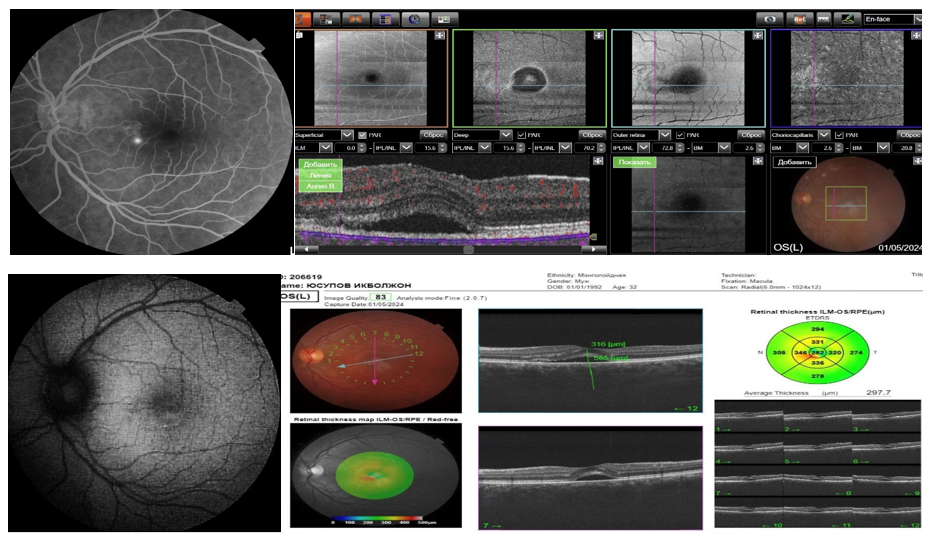
- All patients underwent FA, and retrospective analysis of the results showed that 1 FP was detected in 28 eyes. In addition, 2 pieces of FP were detected in 9 eyes, and 3 pieces of FP were detected in 5 eyes. FP detected on examination has various appearances, such as "pipe smoke," "ink stain," and "flashlight." Diffuse dye leakage was detected in 25 eyes. When the macular area is conditionally divided into 4 segments using perpendicular lines passing through the center of the fovea, the percentage of FN meeting is 32.7% in the upper outer square, 12.68% in the upper inner square, 11.8% in the lower inner square, 22.13% in the lower outer square, and 20.69% in the subfoveolar. The average height of the detached retinal neuroepithelium in patients with acute form was 279.2±139.6 mkm, and in chronic form it was 230.4±110.2 mkm. In 18 patients with acute form, 28.12% local PE detachment was observed, and in 13 (20.3%) patients, the area of detached PE and the hyper- and hypoAF foci of AF were determined to correspond to the FP area determined by FAG examination (Fig. 1). In 13 patients with PE detachment, the outer phalanges of photoreceptors in the projection of the detached pigment epithelial point were thinned, and their average thickness was 35.7±13.6 mkm. The average thickness of photoreceptors in the other projection is 67.38±5.22 mkm, and a statistical difference was found when comparing these parameters. (r<0.05).
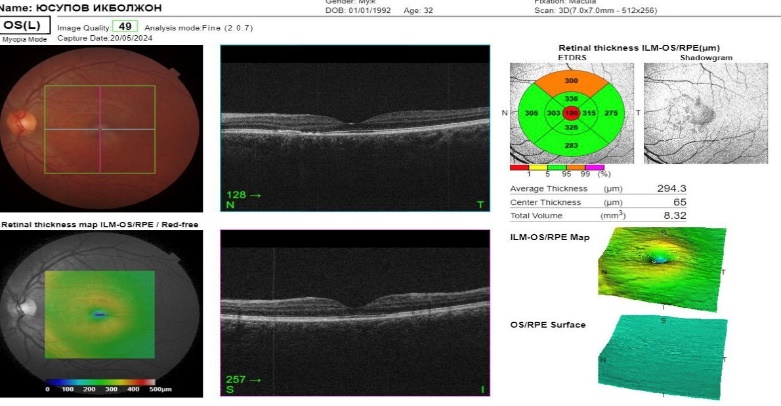 | Figure 2. On OCT 1 month after subthreshold micropulse laser therapy, we can see that the subretinal fluid is completely absorbed and the NE is in place |
4. Conclusions
- The results of the examination and observations show that the results of the examination and observation of the patients who underwent subthreshold micropulse laser therapy on the yellow (577 nm) wavelength "Easy Ret Quantal Medical" (France) laser device showed the effectiveness and safety of this treatment method in the treatment of various forms of the CSCR disease.This type of laser allows for laser intervention when the FP is located in the subfoveal area and with a chronic form of the disease with a large area of diffuse hyperfluorescence; in cases where the FP is not detected in the PE area, and in cases of recurrence of the disease, it allows to perform repeated laser intervention several times without complications.In 13 patients, or 20% of the patients, it was found that the projection correspondence of the filtration point corresponds to the area of pigment epithelial detachment, and these changes correspond to the area of hyper- and hypofluorescence foci of AF, mainly, there was a full correspondence of cases where one filtration point was detected in FA examination and one retinal pigment epithelial detachment in OCT examination.Evaluating the efficiency of microinvasive methods in determining the filtration point in the acute form of central serous chorioretinopathy and creating new treatment algorithms based on the obtained analyses will make it possible to treat the disease in cases where FA examination is not possible.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML