-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2432-2438
doi:10.5923/j.ajmms.20241409.66
Received: Aug. 19, 2024; Accepted: Sep. 15, 2024; Published: Sep. 30, 2024

The Role of ENT Organs in the Development of Hypoxia in Children with Secondary Temporomandibular Joint Deforming Osteoarthritis
Shaykhova H. E.1, Yakubov R. R.2, Yakubov R. K.3
1D.Sc, Professor, Tashkent Medical Academy, Uzbekistan
2Researcher, Tashkent Medical Academy, Uzbekistan
3D.Sc, Professor, Tashkent State Dental Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Secondary deforming osteoarthritis of the temporomandibular joint (TMJ) in children is a multifactorial and polyetiologic disease, which is complicated by respiratory apnea with its consequences in the form of hypoxia and acidosis. The main causes and factors of endogenous hypoxia in children with TMJD in correlation with general pathology and diseases of ENT organs are insufficiently studied.
Keywords: Nasal septal deviations, Rhinitis, Pharyngeal tonsil, Hypoxia, Osteoarthritis, Osteoarthritis, Temporomandibular joint
Cite this paper: Shaykhova H. E., Yakubov R. R., Yakubov R. K., The Role of ENT Organs in the Development of Hypoxia in Children with Secondary Temporomandibular Joint Deforming Osteoarthritis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2432-2438. doi: 10.5923/j.ajmms.20241409.66.
Article Outline
1. Introduction
- The problem of complex rehabilitation of children with secondary deforming osteoarthrosis of the temporomandibular joint (SDO TMJ), prediction and prevention of complications is one of the most important tasks of modern pediatrics and pediatric maxillofacial surgery. The multifactorial nature and polymorphism of this pathology are noted. Among the main causes, the authors identify trauma, inflammatory diseases of the ear, hematogenous and odontogenic osteomyelitis, as well as undifferentiated connective tissue dysplasia [8,15,27].Yakubov R.K., Azimov M.I. (2001) note the importance of diseases of internal organs and systems. [25]. According to Khitrov N.A. (2011). Osteoarthrosis is a chronic progressive disease of the joints - not a single disease, but a whole group of diseases with similar pathomorphological processes and pathogenetic features of development. [10]. All patients with SDO TMJ require surgical and orthodontic stages of treatment: distraction osteogenesis (DO) and/or mandibular condylectomy with bone grafting, mandibular endoprosthetics in order to restore the impaired forms and functions of the TMJ. However, complications such as osteolysis, infection with rejection of the transplanted bone tissue, contracture, recurrence of deformity and respiratory problems often occur [15,22].An important concept has recently appeared in the world literature – the «United Airways». [21] That is, the cavities of the nose, mouth, paranasal sinuses, auditory tubes, middle ear, pharynx, larynx, trachea, bronchi and lungs are actually extensions of each other and interconnected with each other.A significant role is played by hypoxia, which stimulates the formation and action of osteoclasts, increasing bone resorption, and worsening the remodeling of bone and soft tissues [1,19,20,23].Experimental and clinical studies have established the role of hypoxia in disrupting the processes of bone tissue remodeling, associated with the activation of inflammatory factors, angiogenesis and osteoclast formation, with the induction of osteoclastic resorption of bone tissue [3,14,16].Manifestations of intermittent hypoxia and obstructive sleep apnea syndrome (OSA), are mainly associated with difficulty in nasal breathing, partial or complete restriction of movements of the lower jaw, one- or two-sided retro-microgenia with dislocation of the tongue, aggravated during sleep in the supine position, accompanied by severe snoring. Sleep apnea is a cessation of breathing during sleep with a decrease of up to 90% or absence of pulmonary ventilation for more than 10 seconds. It is accompanied by short-term pauses in breathing (there can be from 5 to several hundred of them during the night), snoring, anxiety, and a feeling of constant fatigue due to lack of proper sleep.Gas exchange between the body and the environment, including the absorption of oxygen and the release of carbon dioxide, as well as the transport of these gases within the body through the system of respiratory tubes is called external respiration.Decreased minute ventilation can occur at all levels of the respiratory system, including insufficient respiratory activity (brain stem), impaired transmission of respiratory impulses (spinal cord, peripheral nerves), as well as morphological or functional abnormalities of the musculoskeletal system, chest, scoliosis [2,7].Clinicians recommend screening for nocturnal hypoventilation (NH) in individuals with neuromuscular diseases with a predicted <70% forced expiratory vital capacity of the lungs (FVC). <65% is predicted, especially in the presence of scoliosis. Children with nocturnal hypovetilation appear to have greater gas retention and decreased muscle strength compared to those who do not. They perceive a deterioration in their general health [9].Researchers health-related quality of life and well-being were found to be significantly worse in pediatric patients suffering from four important otolaryngological diseases: chronic sinusitis, deviated septum, hypertrophy of the nasopharyngeal tonsil and hearing diseases [5,11].Analysis of literature data shows that patients with SDO TMJ experience clinical symptoms. Manifestations of intermittent hypoxia and obstructive sleep apnea syndrome, the main cause of which is local pathological processes - jaw deformation, retromicrogenia, changes in the ENT organs: deformation of the nasal septum, etc. But they are the cause of structural disorders of the upper respiratory tract with narrowing of the airways and a decrease in air flow velocity. The causes of hypoxia associated with changes in other parts of the bronchopulmonary are not taken into account. Restrictive ventilation disorders are caused by processes that limit the filling of the lungs with air. The cause of such disorders can be not only changes in the lungs themselves, associated with an increase in the elasticity of the lung tissue (edema, pulmonary fibrosis, etc.), but also external causes that limit the mobility of the chest (kyphoscoliosis, trauma and deformation of the chest, etc. d.). Inspiratory disturbances in extrapulmonary diseases are caused either by weakness of the inspiratory muscles or by chest rigidity. In both cases, the effort of the inspiratory muscles is not enough to significantly expand the chest.Detection of airway obstruction and assessment of its severity is the most common indication for spirometry. Spirometry is a non-invasive method for measuring air flows and volumes during quiescent and forced breathing maneuvers.Narrowing of the airways leads to a drop in airflow velocity due to increased bronchial resistance, which is functionally manifested by a decrease in the speed parameters of forced exhalation. The degree of decrease in maximal expiratory flow (MEF) as you exhale from 25 to 75% forced expiratory vital capacity of the lungs (FVC) reflects the dynamics of the resistance provided by the ventilation device to breathing. Its part, corresponding to 0–25% of exhaled FVC, reflects the air patency of the large bronchi, trachea and upper respiratory tract, the section from 50 to 85% of FVC reflects the patency of the distal bronchi and bronchioles. A deflection in the descending portion of the curve in the expiratory region of 75–85% FVC indicates a decrease in the patency of small bronchi and bronchioles. These indicators are of greatest value in diagnosing initial disorders of bronchial obstruction [6,17].Since bronchial resistance is important in the development of bronchial asthma, an increase in resistance (for example, against the background of edema of the mucous membranes of the upper respiratory tract) may be the main mechanism in the occurrence of expiratory dyspnea. Disorders of nasal breathing against the background of narrowing of the lumen of the upper respiratory tract may also be etiological factors leading to increased resistance.The causes and factors of endogenous hypoxia in children with SDO TMJ in connection with general pathology and diseases of the ENT organs remain unstudied. Many researchers point out the need for an in-depth study of the relationship between local hypoxia factors and the development and chronicity of inflammatory diseases of the nasal cavity and paranasal sinuses.The purpose of our research is to diagnose the pathology of the ENT organs, as a respiratory factor of endogenous hypoxia, which contributes to impaired external respiration in children with SDO TMJ, as one of the factors of the causes and/or consequences of hypoxia and contributing to the chronicity of inflammatory processes.
2. Material and Research Methods
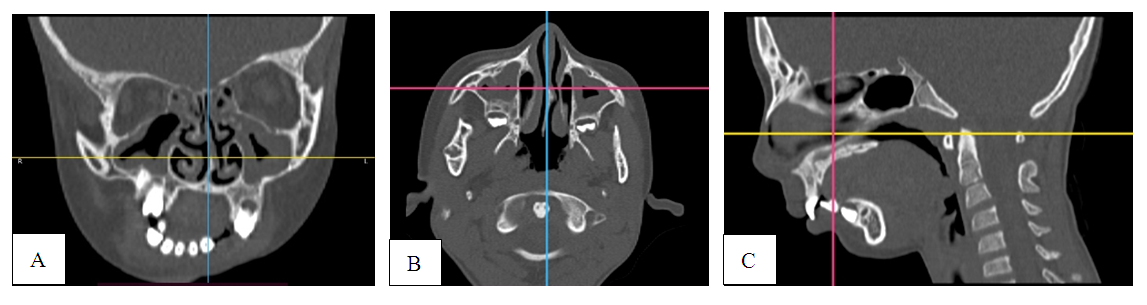
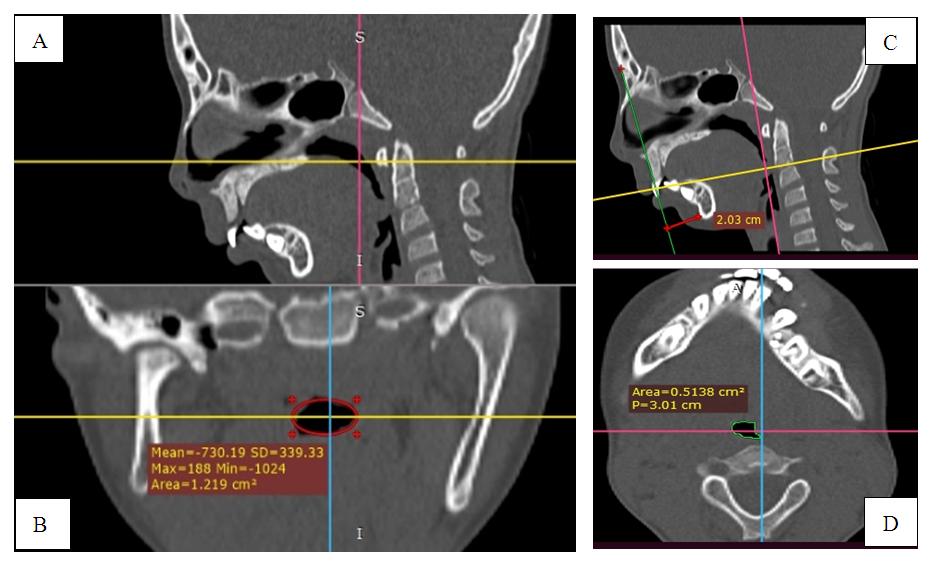
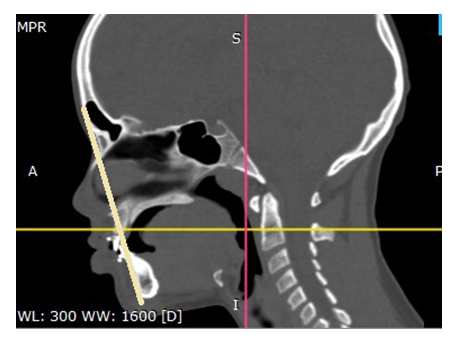
- During the period from 2018 to 2023, in order to diagnose and treat diseases of the ENT organs during their preparation for surgery under general anesthesia with endonasal intubation using a bronchoscope, 65 sick children with SDO TMJ were examined in the department of pediatric maxillofacial surgery of the Tashkent state dental institute and in the department of otorhinolaryngology at the multidisciplinary clinic of the Tashkent Medical Academy [26]. Depending on the period of development of the body, the children were divided into 3 age groups. At the age of 3-6 years, 18 patients were examined, 7-11 years-23, 12-18 years - 24 patients. The frequency of treatment in all groups was approximately the same.The examination methods included standard methods: study of anamnesis, complaints, general examination of ENT organs, clinical and laboratory, X-ray examination (MSCT of the maxillofacial region and ENT organs). Among the factors affecting external respiration, in addition to the above-mentioned areas, the physical development of children was studied, which included: measurement of body size and weight (anthropometry by centiles), changes in the shape of the chest, physiometric indicators (such as vital capacity of the lungs) by spirometry [17].
3. Research Results
- We divided all complaints presented by patients and their parents into external - and facial symmetry with violation of aesthetic proportions, limited mouth opening, difficulty chewing - in 92.3%. From the ENT organs - 76.9%. 78.4% of patients complained of the presence of neurological disorders, 53.8% of patients complained of dysfunction of the digestive organs.%. (Figure 1)
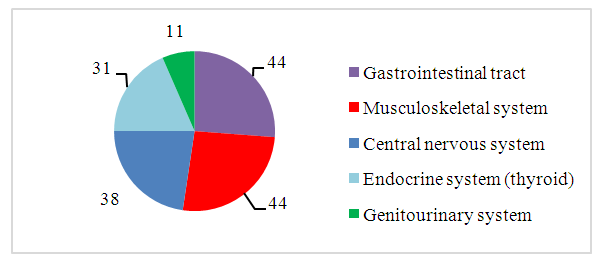 | Figure 1. General incidence of children with SDO TMJ |
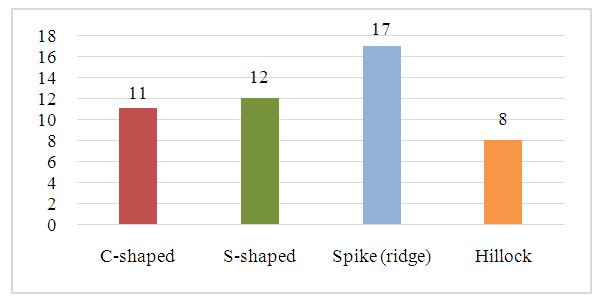 | Figure 2. Frequency of occurrence and forms of deviated nasal septum |
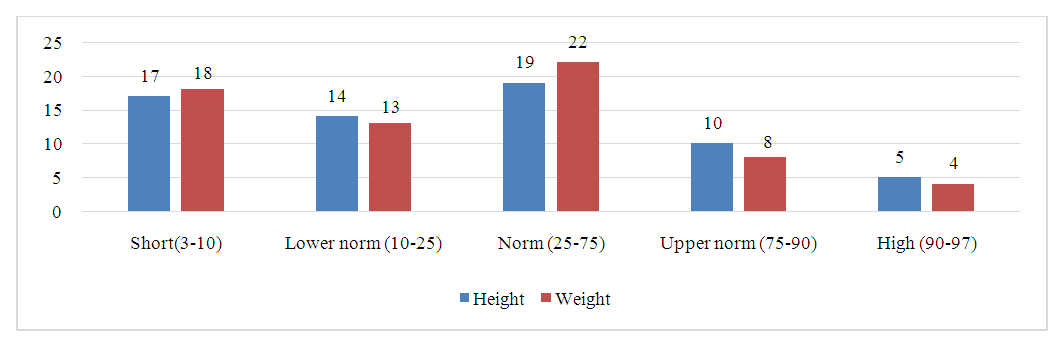 | Figure 3. Results of height and weight assessment by centiles |
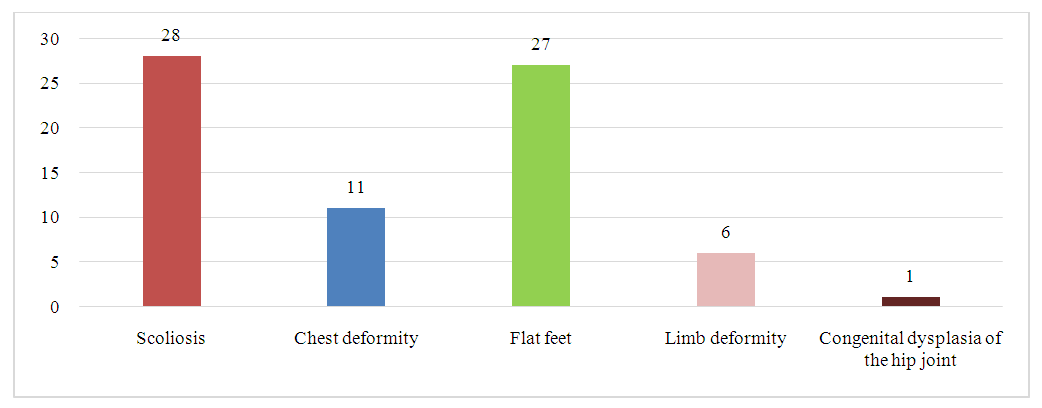 | Figure 4. Combined pathology of the skeletal system in children with SDO TMJ (n=37) |
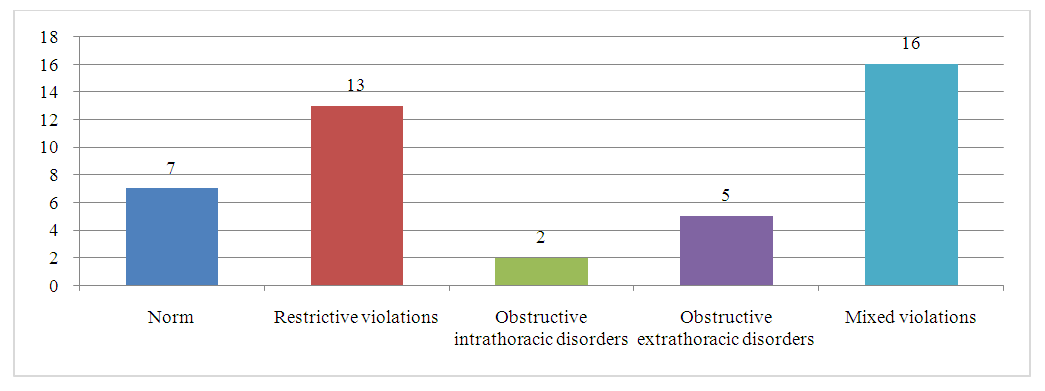 | Figure 5. Detected external respiration disorders according to spirometry findings (n=43) |
4. Clinical Example
- Patient L., 11 years old, turned to our clinic with a diagnosis: SDO TMJ on the right, microgenia.
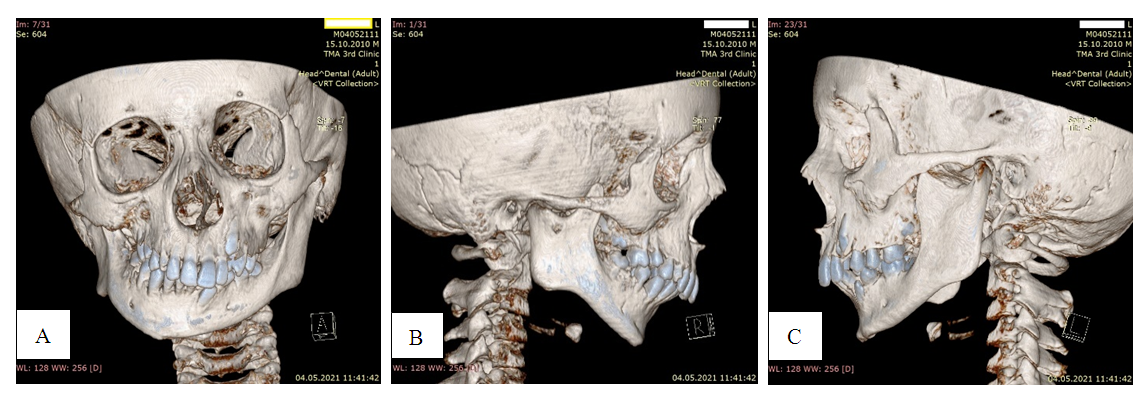 | Photo 1. MSCT photographs of a patient with: A - significant deformation of the facial bones and jaws with laterognathia. B, C-microretrogeny |
 | Photo 4. MSCT of a patient with a bilateral fracture of the articular head in the stage of osteoarthritis without retromicrogenism and respiratory apnea: normal pharyngeal lumen is noted |
5. Conclusions
- In children with retarded physical development, diseases of both the gastrointestinal tract, nervous, endocrine, and musculoskeletal systems were observed, manifested by poor posture, deformities of the chest, changes in muscle tone involved in ventilation of the lungs, masticatory muscles and other parts of the body.Diseases of the ENT organs that occur with respiratory disorders negatively affect the child’s health and lead to the development or progression of somatic pathology.Somatic pathology in children with SDO TMJ leads to delayed physical development and bronchopulmonary syndrome with impairment of external respiration in the form of obstructive, restrictive and mixed forms respiratory disorders, which in many cases are the trigger for the development of hypoxic conditions.Disturbances in the area of the upper and lower respiratory tract negatively affect the child’s body, in the development of age-related dynamics during periods of morphogenesis, neurohumoral restructuring, sexual and somatic development. Of course, this is important in the preparation and conduct of surgical treatment and rehabilitation of patients with SDO TMJ.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML