-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2416-2418
doi:10.5923/j.ajmms.20241409.62
Received: Aug. 29, 2024; Accepted: Sep. 20, 2024; Published: Sep. 30, 2024

Determination of the Degree of Inflammation in the Organs of COVID-19 Patients
Razzakova Sh. O., Akhmedova Х. Yu.
Republican Specialized Scientific and Practical Medical Center of Epidemiology, Microbiology, Infectious and Parasitic Diseases, Tashkent, Uzbekistan
Correspondence to: Razzakova Sh. O., Republican Specialized Scientific and Practical Medical Center of Epidemiology, Microbiology, Infectious and Parasitic Diseases, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The level of antigen-binding lymphocytes specifically sensitizing to tissue antigens of some internal organs (lungs, liver, kidneys, brain) was evaluated in patients with COVID-19 who were hospitalized for inpatient treatment in the clinic of the Republican Specialized Scientific and Practical Medical Center of Epidemiology, Microbiology and Infectious and Parasitic Diseases (RSSPMCEMIPD) in the dynamics of the disease. We enrolled 161 patients diagnosed with coronavirus infection COVID-19 (ICD code U07.1 to U07.2) aged 17 to 93 years. The mean age of patients was 47.63±1.31 years, and patients aged 41 to 61 (52.2%) prevailed. There were 43 (26.7%) males and 117 (72.7%) females. The SARS-CoV-2 virus was identified in all (100%) patients. A comparative analysis of the rate of decrease in the antigen-binding lymphocyte (ABL) to tissue antigen (TAG) values of the corresponding organs relative to the values before treatment showed certain effectiveness of the treatment, but taking into account the persistently high level of ABL to TAG organs relative to the values in the control group, we might say that a pathological process of varying intensity persists in the organism.
Keywords: Antigen-binding lymphocytes, COVID-19, Multiple organ lesions, SARS-CoV-2, Tissue antigens
Cite this paper: Razzakova Sh. O., Akhmedova Х. Yu., Determination of the Degree of Inflammation in the Organs of COVID-19 Patients, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2416-2418. doi: 10.5923/j.ajmms.20241409.62.
Article Outline
1. Introduction
- Coronavirus infection is now an integral part of our daily lives, forcing us to rethink our usual routines and introduce elements of safety and precaution. The uniqueness of this virus is due to the presence of ACE-2 and CD147 receptors, which are found on a wide variety of cells (including stem cells) and tissues, leading to the development of multiple organ lesions [1,2].To date, extensive scientific research has confirmed that the key factors underlying the development of multi-organ disorders are three interrelated mechanisms: The first is the direct cytopathic effect of the virus on target cells, the second is the cytokine storm that leads to tissue and vascular damage, stimulates the inflammatory response and coagulopathy, involving lymphocytes and macrophages, and the third is direct damage to the endothelium of blood vessels and organ cells, resulting in thrombosis and hemorrhage [3,4,5].Coronavirus infection is associated with various cardiovascular diseases such as myocardial inflammation, endocardial and pericardial inflammation, acute myocardial infarction, small-focal cardiosclerosis, and cardiomyopathy [6,7].COVID-19 studies found that 14 to 53% of patients suffered mild to moderate liver damage. Clinical signs included elevated aminotransferase levels, decreased blood protein levels, and prolongation of clotting time. The more severe the course of the disease, the more liver damage was detected.Clinical manifestations of the gastrointestinal tract in COVID-19 vary greatly and include anorexia (39.9-50.2%), diarrhea (2-49.5%), vomiting (3.6-66.7%), nausea (1-29.4%), abdominal pain (2.2–6.0%) and gastrointestinal intestinal bleeding (4-13.7%). It was observed before and after diagnosis as an intestinal symptom in children and adults with an average duration of 4.1±2.5 days and was observed before and after diagnosis of COVID-19.Additionally, numerous studies have shown a lesion of the pancreas, which is caused by the expression of CE2 in the pancreas, and the level of messenger ribonucleic acid (mRNA) in the pancreas is higher than that in the lungs. In other studies, SARS-mediated damage to pancreatic β-cells has been suggested as a likely mechanism for the development of "acute diabetes" in patients with acute respiratory viral infections [8].Having studied the peculiarities of disease development affecting multiple organs and systems, we analyzed the level of antigen-binding lymphocytes (ABL) reacting to tissue antigens (TAG) of lung, liver, kidney, and brain. We compared the dynamics of antigen-binding lymphocyte indices in relation to different tissue antigens to determine the degree of inflammation in organs and to assess the effectiveness of therapy in patients undergoing evaluation [9,10,11].Because of the importance of this disease to medicine and society, many prominent publications are rapidly disseminating information about COVID-19. However, to date, recommendations for the identification and management of comorbid conditions in patients with COVID-19 have not been based on a systematic review [12].
2. Purpose of the Study
- Determination of the depth of the inflammatory process in the organs and evaluation of the effectiveness of the therapy by studying the dynamics of indicators of antigen-binding lymphocytes to certain tissue antigens.
3. Material and Methods
- To achieve this goal, we conducted a comparative analysis of the indicators of patients who were under observation at the RSScPMCEMIPD clinic in period from July to August 2021. The study included 161 patients diagnosed with COVID-19 coronavirus infection (ICD code U07,1 - U07,2) aged 17 to 93 years. The average age of patients was 47,63±1,31 years, and patients aged 41 to 61 (52,2%) years prevailed. There were 43 (26,7%) males and 117 (72,7%) females. The SARS-CoV-2 virus was identified in all (100%) patients. The examination of patients was carried out according to the temporary guidelines «Prevention, diagnosis, and treatment of new coronavirus infection (COVID-19) » (Version 8).The level of ABL to TAG reflects the intensity of the processes of destruction and necrosis of structures in the organ: an increase in ABL in dynamics indicates an increase, and a decrease in ABL indicates an extinction of the intensity of these processes, which allows us to assess the degree of organ damage, as well as the effectiveness of therapy. The value of the method for determining ABL to TAG is its high sensitivity and specificity: the content of ABL reaches a diagnostic level in the early stages and long before the manifestation of clinical signs of organ damage, which makes it possible to predict the risk of organ failure early. The formulation of the ABL reaction with the TAG of several organs makes it possible to identify multiple organ damage to the body during the development of the disease.For quantitative registration of ABL specifically sensitized relative to TAG of various organs, an indirect rosette formation reaction (IRFR) was used according to the method of Garib F.Yu. [13].Lymphocytes were isolated from whole heparinized blood by centrifugation in a density gradient of Ficoll-verografin 1,077 g/ml.
4. Research Results
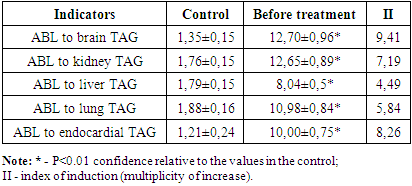
- The analysis of the conducted studies in patients with acute respiratory viral infections-2 showed that in almost all the internal organs studied by us (brain, liver, lungs, kidneys, hearts, etc.) of patients, pronounced inflammatory changes were observed to varying degrees. The results obtained are shown in table 1.
|
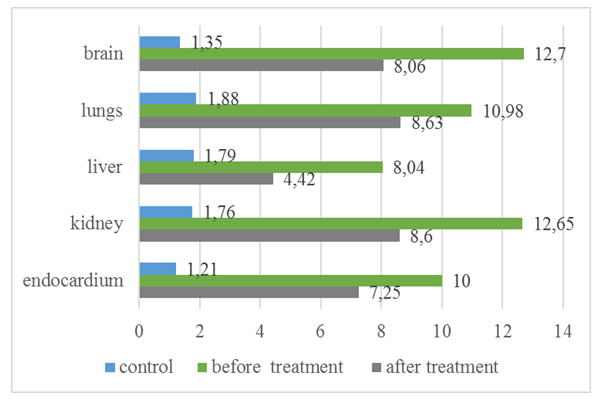 | Diagram 1. Dynamics of ABL to TAG of the brain, liver, kidneys, lungs, and endocardium |
5. Conclusions
- Analyzing the decrease in the level of ABL to TAG in the organs of the patients as a result of the treatment, a certain effectiveness of the therapy was revealed. However, considering the high level of TAG-ABL in the organs compared to the control group, it can be concluded that the pathological process is still present in the body to varying degrees. This, in turn, implies the need to continue the treatment or to make adjustments to the applied traditional therapy regimens.Contribution of authors. The concept and design of the study – Razzakova Sh.O., Akhmedova X.Yu.; collection and processing of material - Razzakova Sh.O.; statistical processing – Razzakova Sh.O.; writing the text - Razzakova Sh.O., Akhmedova X.Yu.; editing - Akhmedova X. Yu.Conflict of interest. The authors declare no conflict of interest.Funding – the study and preparation on the article did not receive financial support.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML