-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2397-2401
doi:10.5923/j.ajmms.20241409.58
Received: Aug. 22, 2024; Accepted: Sep. 15, 2024; Published: Sep. 30, 2024

Optimized Surgical Tactics for Ulcerative Gastroduodenal Bleeding in the Elderly
Abdullajanov Baxrom Rustamovich1, Botirov Akramjon Kodiraliyevich2, Akhmadbekov Bekzodbek Olimbek O`g`li3, Otakuziev Axmadillo Zokirovich4
1Professor of the Department of Surgical Diseases, Doctor of Medical Sciences, Andijan State Medical Institute, Uzbekistan
2Free Applicant for the Department of Surgical Diseases, Andijan State Medical Institute, Uzbekistan
3Head of the Department of Surgical Diseases, Doctor of Medical Sciences, Professor, Andijan State Medical Institute, Uzbekistan
4Associate Professor, Department of Surgical Diseases, Andijan State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The authors report that in the present study, optimization of surgical tactics reduced overall mortality in gastroduodenal ulcerative bleeding in a prospective group of patients to 2.4% versus 5.9% in a retrospective group. The authors conclude that improved treatment results were achieved by reducing surgical activity from 44 to 21%, reducing emergency surgical interventions, and also by reducing postoperative mortality after delayed operations from 5.9 to 2.4% through adequate preoperative preparation and reducing the rate of recurrent bleeding from 19.6 to 4.8%.
Keywords: Ulcerative gastroduodenal bleeding, Old age, Diagnostic and treatment algorithm
Cite this paper: Abdullajanov Baxrom Rustamovich, Botirov Akramjon Kodiraliyevich, Akhmadbekov Bekzodbek Olimbek O`g`li, Otakuziev Axmadillo Zokirovich, Optimized Surgical Tactics for Ulcerative Gastroduodenal Bleeding in the Elderly, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2397-2401. doi: 10.5923/j.ajmms.20241409.58.
Article Outline
1. Relevance of the Problem
- Over the past decades, surgical tactics for ulcerative gastroduodenal bleeding have undergone changes associated with the introduction of modern equipment and new means for endoscopic hemostasis and a revision of approaches to performing surgical procedures. However, in most cases, surgeons with ongoing bleeding, in the event of ineffective endoscopic hemostasis or technical difficulties in treating recurrent ulcerative gastroduodenal bleeding, resort to emergency surgical interventions. At the same time, in elderly people, some typological features (including chronic ulcer or acute drug ulcer) ulcerative gastroduodenal bleeding are often not taken into account, which is often the cause of tactical and technical omissions, and, accordingly, a high incidence of general and postoperative mortality and complications [1-3]. The aim of this research was to improve the results of surgical treatment of Ulcerative gastroduodenal bleeding in the elderly by determining the characteristics of the clinical course and optimizing surgical tactics.
2. Material and Methods
- The work is based on an analysis of the results of treatment of 326 patients subject to inpatient treatment at the Department of Surgical Diseases in the clinic of the Andijan State Medical Institute named after Otabekov Yu.O and in the Andijan branch of the Republican Scientific Center for Emergency Medical Care for the period from 2019 to 2023. At the same time, patients with Ulcerative gastroduodenal bleeding are conditionally divided into two groups:- control group (234 patients), under the age of 60 years (average age was 35.3±0.5; p <0.001);- the study group (92 patients), in old age (average age was 67.2±0.5 (p <0.001).To solve the assigned problems, general clinical, laboratory, instrumental and statistical research methods were used in accordance with protocols approved by the Ministry of Health of the Republic of Uzbekistan.
3. Results and Their Discussion
- In all patients, bleeding was diagnosed based on clinical signs such as the presence of melena (88.4%); and vomiting “coffee grounds” (71.5%). Other signs were not expressed sufficiently. In most cases, the diagnosis of bleeding was late. Often the presence of tarry stools was associated with taking iron supplements, and patients were examined by a surgeon 2-3 days after the onset of bleeding. This situation was identified in 12 patients. This circumstance worsens the results of treatment of bleeding in this group of patients; in addition, ongoing bleeding contributes to an increase in ischemia of internal organs, including the myocardium and brain. A vicious circle develops.To objectively assess the severity of the condition and predict the outcome of the disease, we used the integrated original simplified SAPS scale (Original Simplified Acute Physiology Score). Data were obtained for the first 24 hours of patients' stay in the intensive care unit. As the SAPS value increases, the probability of an unfavorable (fatal) outcome of the disease increases. A retrospective analysis of the results of surgical treatment in the comparison group (2016-2019) showed that the severity of the physiological condition of patients with ongoing bleeding, the degree of blood loss, and the risk of relapse in case of unstable hemostasis and existing bleeding were underestimated with due objectivity. As a result, we performed a large number of urgent operations at the height of bleeding, and time was lost for thorough preoperative preparation.Underestimation of the severity of the condition in 14 (10.9%) patients led to insufficient replenishment of blood volume, in 8 (6.3%) - a late decision to operate, as a result of which it was not possible to compensate for the changes that occurred as a result of blood loss. Identified omissions in previously used treatment tactics for elderly patients with Ulcerative gastroduodenal bleeding contributed to the development of an improved treatment and diagnostic algorithm, taking into account some typological features, which made it possible to optimize surgical tactics by predicting recurrent bleeding and achieving improved results of surgical treatment.Based on the results of treatment of patients in the control group, seven of the most informative diagnostic signs were selected according to risk factors: 1) age of the patient; 2) a history of coffee-ground vomiting and/or melena more than 2 times a day; 3) the number of red blood cells is below 2.5-1012/l, hemoglobin is below 100 g/l; 4) hypotension of blood pressure below 80/40 mm Hg and pulse above 100 beats. /min); 5) localization of the ulcer; 6) size of the ulcerative defect; 7) endoscopic picture according to Forrest.Emergency fibroesophagogastroduodenoscopy was performed in 80 (86.9%) patients, including 41 patients of the main group with Ulcerative gastroduodenal bleeding. There were 38 (41.3%) patients with acute ulcers, 54 (58.7%) with chronic ulcers. According to our data, patients with chronic ulcers predominated. During fibroesophagogastroduodenoscopy, ongoing bleeding was detected in 38 (41.2%) (Forrest I), ongoing bleeding in 45 (49.0%) (Forrest II), and anamnestic gastrointestinal bleeding in 9 (9.8) (Forrest III) patients in groups of patients. Mild blood loss was diagnosed in 9 (9.8%) patients, moderate in 45 (49.0%), severe in 23 (25.0%), and extremely severe in 15 (16.2%). According to our data, average and severe blood loss was 73.9%.More often, an ulcerative defect was found in the stomach - 35 (38.0%) patients, duodenal ulcers in 57 (62.05%). Acute ulcers were multiple and small in size. Chronic ulcerative defects were more often single and large in size. According to our data, almost 30 (32.6%) ulcerative defects had sizes from 0.2 to 1 cm, 36 (39.1%) from 1 cm to 2 and 26 (28.3%) from 2.5-3 cm and more. From the anamnesis it was established that due to the presence of various (49) concomitant pathologies, 27 patients periodically took NSAIDs, and 22 patients took anticoagulants.Indications for endoscopic hemostasis were: ongoing bleeding (F-Ia, F-Ib). In case of unstable hemostasis (F-IIa, F-IIb and F-IIc), endoscopic hemostasis was also performed. In cases of stopped bleeding, control endoscopy was performed on the 7th and 14th days. To assess the source of bleeding, the most convenient classification is J. Forrest (1987). The use of endoscopic hemostasis and complex antiulcer therapy, including proton pump inhibitors, cytoprotectors, and Helicobacter agents, made it possible to achieve reliable hemostasis and accelerate reparative processes.In the diagnosis of acute ulcerative gastroduodenal bleeding, the following tasks are solved: 1) establish the fact of bleeding; 2) identify the nature and location of the source of bleeding; 3) find out whether the bleeding continues or has stopped; 4) in case of stopped bleeding, assess the degree of stability of hemostasis; 5) determine the amount of blood loss; 6) assess the severity of concomitant diseases.Clinical signs of unstable hemostasis are: a recorded collaptoid state during bleeding, the presence of laboratory signs of severe blood loss, repeated hemorrhagic attacks recorded on the basis of obvious signs of bleeding. In this regard, for Ulcerative gastroduodenal bleeding in elderly people, we have proposed an improved treatment and diagnostic algorithm, which is presented in picture 1.
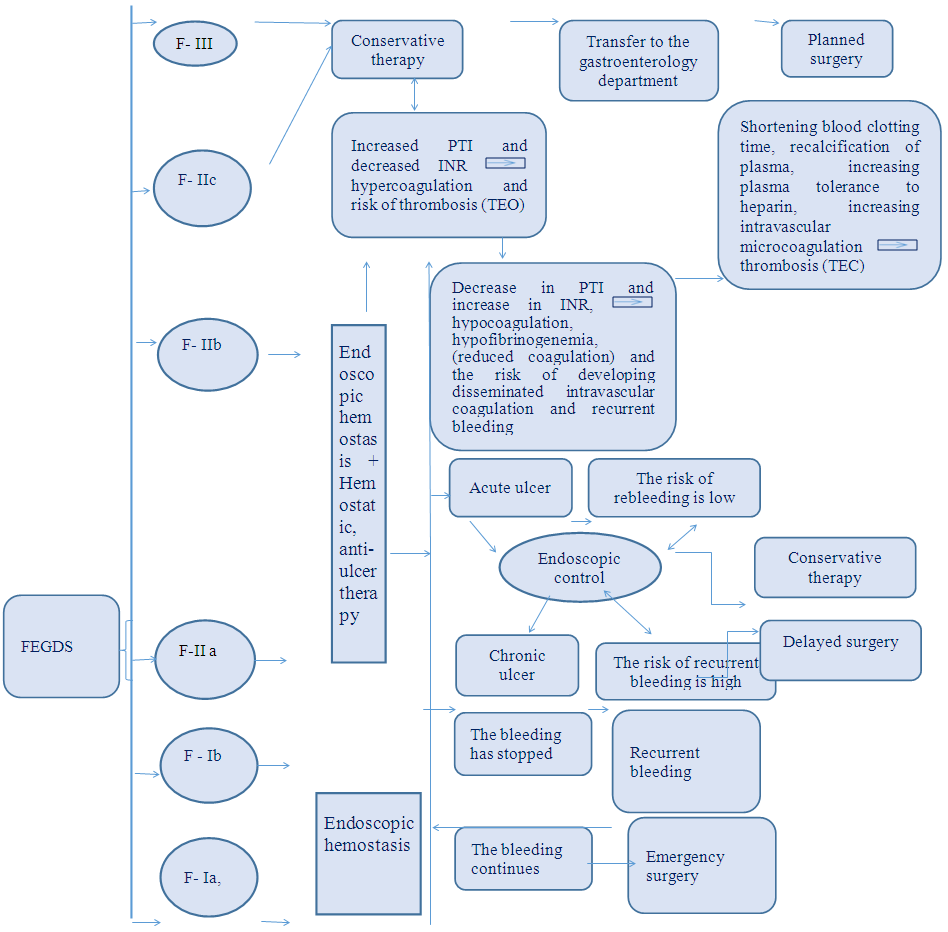 | Picture 1. Improved treatment and diagnostic algorithm |
4. Summary
- Thus, in the present study, optimized surgical tactics made it possible to reduce the overall mortality rate for Ulcerative gastroduodenal bleeding in a prospective group of patients to 2.4% versus 5.9% in a retrospective group. Improved treatment results were achieved by reducing surgical activity from 44 to 21%, reducing emergency surgical interventions, as well as by reducing postoperative mortality after delayed operations from 5.9 to 2.4% through adequate preoperative preparation and reducing the frequency of recurrent bleeding from 19.6 to 4.8%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML