-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2351-2354
doi:10.5923/j.ajmms.20241409.48
Received: Aug. 23, 2024; Accepted: Sep. 19, 2024; Published: Sep. 28, 2024

Rehabilitation of the Patient's Paralyzed Limbs and Effectiveness of Mobile Application “Stroke Help"
Dilbar Rasulova, Gulnara Rakhimbaeva, Munisa Rasulova
Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbeksitan
Correspondence to: Dilbar Rasulova, Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbeksitan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Stroke rehabilitation - the main goal of recovery is to restore the patient's lost or damaged functions due to a stroke, to help him to social and psychological readaptation, and to prevent another stroke. The recovery process takes years: the patient has to relearn almost everything. For the first time, we have created the mobile application STROKE HELP in Uzbek language in order to provide methodical support to patients' relatives in these procedures. In patients who used the mobile application, we observed a better recovery of muscle strength and degree of paralysis in dynamics, and a decrease in the level of spasticity. STROKE HELP mobile application is a methodical guide for patient's relatives and helps to prevent arthrosis and contractures, one of the bad complications of stroke.
Keywords: Stroke, Stroke help, Mobile application, Post-stroke rehabilitation
Cite this paper: Dilbar Rasulova, Gulnara Rakhimbaeva, Munisa Rasulova, Rehabilitation of the Patient's Paralyzed Limbs and Effectiveness of Mobile Application “Stroke Help", American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2351-2354. doi: 10.5923/j.ajmms.20241409.48.
1. Introduction
- Strokes are the most common diseases of the nervous system, acute disorders of cerebral blood circulation, lasting more than 24 hours or ending with death, focal neurological and general syndromes [1] The brain tragedy starts suddenly, the patient has weakness of arms and legs (hemiparesis) [3], loss of speech (aphasia) [2], facial distortion. The increase in mortality and disability after ischemic strokes [4] requires the relevance of this direction, its comprehensive development and optimization of various approaches to restorative treatment.Stroke rehabilitation - the main goal of recovery is to restore the patient's lost or damaged functions due to a stroke [5], to help him to social and psychological readaptation [6], and to prevent another stroke. The recovery process takes years: the patient has to relearn almost everything. Because we pity and love our patient [7], when he becomes sick, we want to help our dear person in all his difficulties: even if he drinks water on his own, we help him to drink, even if he reaches down to take something, we give it to him. we try to help even if he is self-sufficient, we are even ready to perform gymnastics and exercises for him. But don't we make our patient prematurely disabled by this? The patient gradually becomes submissive, relaxed, the unused functions begin to fade, he stops doing his favorite work. Everyone loses from this: the patient, who feels weak, and the person helping, who is tired of waiting for the result. Untimely medical measures lead to irreversible anatomical and functional changes in the patient's body.According to the recommendations of the EUSI (European Stroke Initiative, 2004), post-stroke rehabilitation measures should be started as early as possible. The goal of early hospitalization of stroke patients is not only rapid diagnosis and drug treatment [8], but also determines the need to start movement recovery early, because the peak of movement recovery is 3 months after the stroke and continues for another 3 months.What neurologic problems occur in the average stroke patient? [9]1. Paralysis - paralysis of an arm or leg - movement disorders [10];2. Balance disorders;3. Pain and sensory disturbances;4. Difficulty swallowing - dysphagia;5. Disorders of the urinary organs - urinary incontinence or constipation;6. Bed sores;7. Speech disorders – aphasia [11];8. Cognitive disorders - difficulty understanding, dementia;9. Seizures;10. Sleep disorders;11. Psychological disorders - anxiety and severe depression;12. Social problems - need for self-support, family conflicts, impairment of working capacity.If the lesion of the brain due to a stroke is large, sepsis-internal poisoning, cardiovascular dysfunction - arrhythmias and myocardial infarction can also be observed in patients with additional, related diseases [12].Therefore, the sooner the diagnosis of stroke is made and the earlier treatment is started, the duration of stroke complications will be shortened and the severity of the neurological symptoms after the disabling stroke will decrease in the patient.
2. Materials and Methods
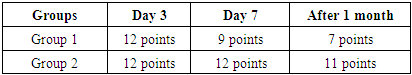
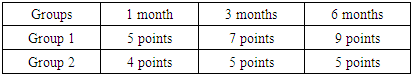
- The purpose of scientific research. Evaluating the effectiveness of the mobile application "STROKE HELP" in the rehabilitation of movement disorders during acute and convalescent brain strokes.Research materials and methods of investigationDuring 2022-2023, in the Department of Neurology and Intensive Neurology of the Tashkent Medical Academy, we examined patients with movement disorders who had acute circulatory disorders in the area of the left middle artery of the brain. The presence of comorbid diseases in all patients: heart disease, diabetes, ischemic heart disease was taken into account. Patients underwent clinical neurological, laboratory tests, neurovisualization methods (cranial CT scan, MRT). We divided 60 stroke patients in the department into 2 groups. Group 1 included 30 patients treated in the intensive neurology department during the acute period of stroke. The prototype of the "Stroke Help" mobile application was downloaded to the Android phones of the relatives of 1 group of patients, and the operation of the application was explained. Group 2 patients were 30 patients who were treated without such guidelines during the acute period of stroke. We used the NIHSS (National Institute of Health Stroke Scale) scale to dynamically assess the severity of neurological symptoms during the acute period of stroke, and the Rivermid scale, which sheds light on the dynamics of the patient's movements during the stroke recovery period. The neurological condition of the patients was examined 3 times: 1) 3 days during the acute period of the stroke; 2) between 7-21 days in the acute period; 3) early recovery period after the patient is discharged home.
3. Results and Discussions
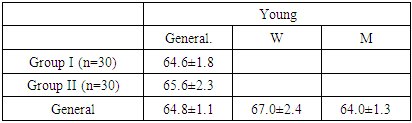
- In the rehabilitation of stroke complications, the greatest emphasis is placed on the patient's family and relatives, because it is the patient's relatives who are considered the main motivators and advocates of the patient's recovery. Relatives of group 1 patients were given a prototype of the "Stroke Help" mobile application, which explains how to care for a stroke patient in the acute phase of the disease, the causes of neurological disorders (hemiparesis, aphasia) observed in the patient, complications that can be observed in bed patients, and how to prevent complications caused by stroke. the principles of prevention were explained.The main goal of acute stroke rehabilitation:1. Early patient activation;2. Prevention of pathological conditions caused by stroke (spastic contractures and arthropathies, thrombophlebitis and bedsores and pneumonias);3. Restoring voluntary movements of the patient.Factors to initiate patient activation included:1. Cessation of destructive disorders of the brain (brain tumor, dislocation of the brain stem and structures);2. Improvement of the patient's hemodynamic indicators;3. Improvement of the patient's well-being.In the obtained results, men made up 45-75%, women made up 15-25%. By age, 64.8 + 1.1 was considered the average age.
|
|
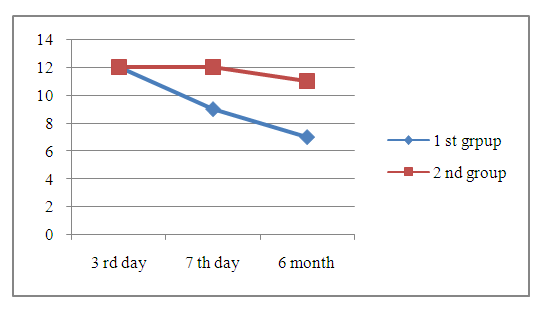 | Diagram 1. Dynamics of NIHSS scale indicators of patients included in the study |
|
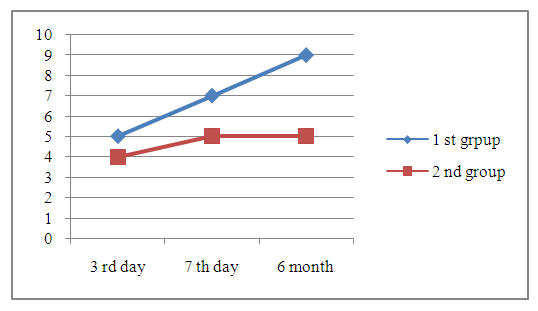 | Diagram 2. The Rivermead scale |
4. Conclusions
- As a conclusion of the scientific work, we created a prototype of the first national mobile application in the Uzbek language, "Stroke Help", which helps to work with stroke patients for the first time in our republic, and recommended it for neurological practice. The use of the mobile application "Stroke Help" has been shown to be effective in improving the degree of paralysis (dynamic recovery, spasticity reduction, muscle strength in dynamics, and speech improvement in patients). This application is an effective methodological guide for relatives of stroke patients. It accelerated the functions of the areas of the brain responsible for movement and speech, which were saved, but temporarily paralyzed, and helped the intensive passage of neurodynamic processes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML