-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2333-2336
doi:10.5923/j.ajmms.20241409.44
Received: Sep. 2, 2024; Accepted: Sep. 20, 2024; Published: Sep. 21, 2024

Indicators of Biochemical and Immunological Profile in Premature Discharge of Amniotic Fluid
Kayumova Guzal Mukhtorovna
Bukhara State Medical Institute named after Abu Ali ibn Sina, Bukhara, Uzbekistan
Correspondence to: Kayumova Guzal Mukhtorovna, Bukhara State Medical Institute named after Abu Ali ibn Sina, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Complication of birth due to premature rupture of the umbilical cord is one of the most important problems of modern obstetrics. According to the duration of the pregnancy, ectopic pregnancy causes the onset of labor in 8-92% of cases. Premature discharge of amniotic fluid is closely related to infection, which in turn increases the risk of purulent-septic complications in a pregnant woman 10 times. Chorioamnionitis is a major risk for a pregnant woman that worsens the delivery process and results.
Keywords: Premature birth, Premature discharge of amniotic fluid, Chorionic amnionitis, Femoflor, Progesterone
Cite this paper: Kayumova Guzal Mukhtorovna, Indicators of Biochemical and Immunological Profile in Premature Discharge of Amniotic Fluid, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2333-2336. doi: 10.5923/j.ajmms.20241409.44.
Article Outline
1. Introduction
- One of the most serious complications of preterm birth is premature amniocentesis. In full-term pregnancy, PDOAF is the most important risk factor for pregnancy complications that threaten the health of the fetus and mother, determines the high level of perinatal and infant morbidity and mortality [1,3,8]. Premature amniocentesis in preterm labor is the most important risk factor for the fetus and mother, as it determines the high risk of morbidity and mortality of perinatal babies. Therefore, complications of premature birth due to rupture of the membranes are one of the most important problems of modern obstetrics [12,18].PDOAF is a complication of pregnancy and is characterized by a violation of the integrity of the fetal membrane and the release of amniotic fluid (before the onset of labor). The frequency of this pathology, according to different authors, varies widely and ranges from 1.0% to 19.8%. According to the World Health Organization, every year in the world 15 million children are born prematurely [16]. The problem of premature birth remains one of the most urgent problems in obstetrics and perinatology, because of the polyetiological nature of this pathology and the lack of a single tactic in the delivery process. Despite the emergence of many drugs used for the risk of preterm birth on the pharmaceutical market, the frequency of PB in different countries has remained stable from 5% to 12% over the past 30 years. In the period from 22 to 28 weeks of pregnancy, the frequency of PB is 5-7% of all cases of this pathology, from 29 to 34 weeks - 33-42%, from 34 to 37 weeks - 50-60% [4,17].
2. Materials and Methods
- Premature and perinatal amniocentesis occupies one of the first places among modern obstetric problems, because it determines the high level of perinatal and infant morbidity and mortality. Premature discharge of amniotic fluid during premature and full-term pregnancy is the most important risk factor for the fetus and the mother [5,7,15].Premature amniocentesis is an urgent problem of modern obstetrics, causing complications for the mother and the fetus possible. Therefore, delivery complicated by premature amniocentesis should be carried out in a maternity hospital based on scientific examination [6,11]. Premature amniocentesis is a common obstetric pathology, occurring in 10-19% of cases in term and in 25-54% of premature births. Childbirth with SCI is often accompanied by various anomalies of uterine contraction activity, in particular, weakness of labor activity (4.9-23%) or discoordination of labor activity (8.3-41.8%) [9,10].Premature rupture of the placenta occurs in 3-10% of all pregnancies. It is determined by the violation of the integrity of the fetal membranes and the release of amniotic fluid before the onset of labor, regardless of the period of pregnancy [13,19].Premature discharge of amniotic fluid in premature pregnancy is one of the urgent problems. This problem should be considered not only medically, but also socially and economically. Premature discharge of amniotic fluid accompanies every third case of premature birth [2,14].PB complicates up to 8% of all pregnancies and is the main reason for the development of spontaneous PB in 30-51%. When preterm labor begins before the 26th week of pregnancy, the percentage of SCC reaches 90-92%.Complication of birth due to premature rupture of the umbilical cord is one of the most important problems of modern obstetrics. According to the duration of the pregnancy, PDOAF causes the onset of labor in 8-92% of cases [13,20].
3. Goal of Study
- A differential approach to pregnancy and childbirth based on changes in the immunological status of the mother-placental-fetus system during premature amniocentesis.In 2022, 177 pregnant women with vaginal discharge who were under control at the perinatal center of Bukhara region were prospectively analyzed. The examined women were divided into 2 groups: 1 group included 107 women who had premature rupture of membranes and gave birth; 30 pregnant women with amniocentesis were divided into 2 groups; 40 relatively healthy pregnant women were selected for the control group.
4. Result and Discussion
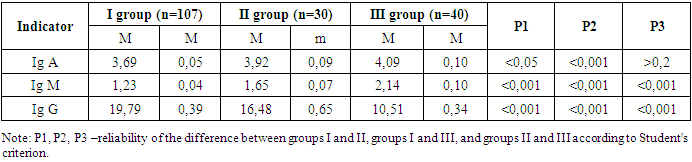
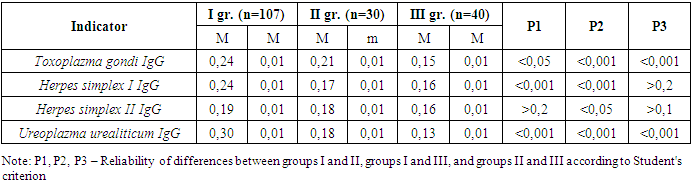
- As part of the study, a comparative analysis of the level of immunoglobulin was conducted in three groups of women. Analysis showed statistically significant changes in immunoglobulin levels between groups. The average value of IgA increased by 3.69 mg/L in the third group compared to the first group, and reached 4.09 mg/L, with the most significant increase between the first and second groups (p<0.001). This indicates an activation of the immune system in response to premature ejaculation, as IgA plays an important role in local immunity and mucosal protection. The amount of IgM was also studied in detail, from 1.23 mg/l in the first group to 2.14 mg/l in the third group. it was found that it increased up to, a high statistical index of changes was noted between all groups (p<0.001). The primary response of the IgM immune system to infection may be due to inflammation associated with potential agents or premature ejaculation. The greatest change was observed in the amount of IgG, which decreased from 19.79 mg/l in the first group to 10.51 mg/l in the third group, the difference between all groups being statistically significant (p<0.001). A decrease in IgG, the main component of humoral immunity, may reflect a long-term load on the immune system or a violation of its regulatory mechanisms under conditions of stress due to premature dehydration (Table 1).
|
|
5. Conclusions
- In order to determine the risk factors for the development of the pathology of premature discharge, it is necessary to analyze the patients' catamnestic and anamnestic data during outpatient or inpatient follow-up. According to the results of the dissertation research, the most common risk factors of pregnancy that cause PDOAF are: hypoxic conditions, pre-pregnancy or related somatic diseases, inflammatory diseases of the genital system. shows support for stress and protection. How it responds to this unaltered state in immunoglobulin levels has an important bearing on the diagnosis and treatment of PDOAF.
ACKNOWLEDGMENTS
- The authors are grateful for the support and helpful comments provided by the department of Obstetrics and gynecology in Bukhara State Medical Institute, as well as other experts consulted as part of the process. We would also like to thank Bukhara city maternity complex for her assistance in creating the figure for our literature search.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML