-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2275-2279
doi:10.5923/j.ajmms.20241409.33
Received: Aug. 12, 2024; Accepted: Sep. 10, 2024; Published: Sep. 18, 2024

Characteristics of Clinical and Functional Features and Microbiota of the Respiratory Tract in Children with Chronic Bronchitis
Aripova Shakhnoza Khabibullaevna1, Shamsiev Furkat Mukhitdinovich2, Musazhanova Rano Anvarbekovna3
1Basic Doctoral Student of the Pulmonology Department of the Republican Specialized Scientific and Practical Medical Center of Pediatrics, Tashkent, Uzbekistan
2Head of the Pulmonology Department of the Republican Specialized Scientific and Practical Medical Center of Pediatrics, Tashkent, Uzbekistan
3Scientific Secretary of the Republican Specialized Scientific and Practical Medical Center of Pediatrics, Tashkent, Uzbekistan
Correspondence to: Aripova Shakhnoza Khabibullaevna, Basic Doctoral Student of the Pulmonology Department of the Republican Specialized Scientific and Practical Medical Center of Pediatrics, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to study the clinical and functional features and microbiota of the respiratory tract in children with chronic bronchitis. Microbiological research methods were used in the process of a comprehensive clinical and functional examination of children. The results of the conducted studies showed that in chronic bronchitis with bronchial obstruction, an excessive growth of Staphylococcus aureus was more often detected, while in non-obstructive course, the most common pathogen was Streptococcus pneumoniae. In addition, in children with chronic bronchitis with bronchial obstruction, an obstructive type of respiratory dysfunction was more often detected, in contrast to children with non-obstructive course, in whom the restrictive type prevailed.
Keywords: Children, Acute and chronic bronchitis, Spirography, Peak flowmetry, Microbiome
Cite this paper: Aripova Shakhnoza Khabibullaevna, Shamsiev Furkat Mukhitdinovich, Musazhanova Rano Anvarbekovna, Characteristics of Clinical and Functional Features and Microbiota of the Respiratory Tract in Children with Chronic Bronchitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2275-2279. doi: 10.5923/j.ajmms.20241409.33.
Article Outline
1. Introduction
- According to official statistics, respiratory diseases account for about 40% of all cases of appeal, which exceeds the levels of other classes of diseases. Almost all nosologies are socially significant, since in addition to high morbidity and mortality, they also bring significant economic damage [4]. Today, clinical observations show that over the past 10 years, chronic bronchopulmonary diseases in children have undergone a significant transformation. This is due to a better understanding of etiopathogenetic mechanisms and the improvement of diagnostic methods [2].According to Yu. L. Mizernitsky, chronic obstructive pulmonary disease (COPD) has become a reality in children. The possibility of emphysema formation in childhood has been proven. Chronic pneumonia has completely "disappeared", having essentially disintegrated into chronic bronchitis (CB) and bronchiectasis [6].The prognosis for chronic bronchitis is always serious, since the inflammation is bilateral and diffuse, progresses over time and leads to irreversible changes in the lungs and the development of respiratory failure. It is this group of patients that requires great attention associated with timely diagnosis, adequate treatment and dispensary observation [5]. CB can often be accompanied by bronchial obstruction. Despite the fact that in recent years there has been an increase in the number of respiratory diseases in children, including bronchitis, occurring with bronchial obstruction syndrome, there are still no clear data on the prevalence of obstructive syndrome in various bronchopulmonary pathologies in children. Diagnosis of chronic bronchitis is based on a combination of clinical and anamnestic data, physical examination results, allergological status, chest X-ray, and respiratory function (FER) testing data: peak flowmetry and spirometry, the technique and technology of which are constantly being improved.Bacteria play a significant role in exacerbations of chronic bronchitis. Currently, there is no doubt that exacerbations play a decisive role in the progression and hospitalization of patients with chronic bronchitis [1]. Chronic colonization of the lower respiratory tract by bacterial pathogens in patients with chronic bronchitis enhances the chronic inflammatory response and leads to progressive airway obstruction (vicious circle hypothesis) [9]. The composition of the microbiome of the respiratory tract and lungs largely depends on the migration of microbial communities from the oral cavity [7]. The most colonized by bacteria are non-sterile parts of the respiratory tract: the oral cavity, nose, oropharynx and larynx. Non-sterile parts of the respiratory tract serve as a reservoir of microorganisms that cause pneumonia, bronchitis, exacerbation of chronic or recurrent bronchitis, otitis media, sinusitis. However, out of more than 300 species of bacteria living in the oral cavities and nasopharynx, only a few can cause diseases. These primarily include pneumococcus, Staphylococcus aureus, Haemophilus influenzae, and Moraxella catarrhalis [8].In this regard, a comprehensive description of the clinical and functional characteristics and microbiota of the respiratory tract in children with chronic bronchitis is a relevant area of scientific research. In addition, the accumulation of scientific data on the microbial composition of the respiratory tract in children with chronic bronchitis will allow a better understanding of the pathogenetic mechanisms of the disease and the justified use of modern methods of microbiological diagnostics.Objective of the study. To study the clinical and functional characteristics and microbiota of the respiratory tract in children with chronic bronchitis.
2. Material and Methods of the Study
- During the research work, 105 patients with chronic lower respiratory tract diseases were examined, who were treated in the pulmonology department of the Republican Scientific and Practical Medical Center of the Ministry of Health of the Republic of Uzbekistan. The group was represented by such nosological forms as chronic bronchitis (CB) (n=41) and CB bronchial obstruction syndrome (BOS) (n=64). The comparison group consisted of 35 children with recurrent obstructive bronchitis (ORB). The diagnosis was made taking into account the ICD-10 classification and based on the systematization of the main clinical forms of bronchopulmonary diseases, which was adopted at a special meeting of the XVIII National Congress on Respiratory Diseases [3].During the comprehensive examination of children, clinical, functional and microbiological studies were used:- study of the function of external respiration (FER) using a SHILLER SPIROVIT SP-1 spirometer (Moscow) and the SEMA 2000 program, was carried out in the pulmonology department of the RSNPMCP of the Ministry of Health of the Republic of Uzbekistan;- monitoring of the peak expiratory flow rate (PEF) using a device - a peak flow meter (Philips Respironics), a portable device with a division scale for children from 35 to 350 l / min., was carried out in the pulmonology department of the RSNPMCP of the Ministry of Health of the Republic of Uzbekistan;- bacteriological examination included: taking swabs from the throat and nose, quantitative and qualitative sowing on nutrient media, identification of isolated cultures, determination of the microbial contamination index (MCI) and assessment of biofilm formation. The studies were carried out in the laboratory of the RSNPMCP of the Ministry of Health of the Republic of Uzbekistan.The obtained results were statistically processed using the software in the Statistica 10 package. We applied the methods of variation statistics to calculate the arithmetic mean (M), confidence interval (m) and test the hypothesis of equality of means using the Student's t-test. Differences were considered statistically significant at p <0.05; p <0.01; p <0.001.
3. Research Results and Their Discussion
- Having analyzed detailed anamnestic data of the examined children, we determined the risk factors for the development of chronic bronchitis in children: higher relative risk and odds ratios for the development of CB with BO in children were revealed in comparison with chronic bronchitis (perinatal factors, passive smoking, artificial feeding, aggravated allergological history on the part of the mother (OR=2.32-9.56; RR=1.34-2.79; p from <0.01 to <0.001), aggravated premorbid background, concomitant and past diseases (OR=2.58-13.3; RR=1.32-3.06; p from <0.01 to <0.001).The results of the analysis of the frequency of clinical symptoms in the selected groups showed that more than half of the children with CB and CB with BO complained of weakness (82.9% and 95.3%), while with OBRС it reached 51.4%. When analyzing the frequency of occurrence among the entire spectrum of complaints - lethargy, which with OBRС occurred in 45.7%, with CB and CB with BO - in 87.8% and 81.3% of cases. In almost all cases, children with CB and CB with BO noted a decrease in appetite (87.5% and 90.2%), with OBRС this percentage was lower and amounted to 65.7%. Paleness of the skin was recorded among children with CB and CB with BO (85.4% and 92.2%), in the group of children with OBRС this percentage was lower and amounted to 80.0%. The presence of cyanosis of the nasolabial triangle, the frequency of which was recorded in most cases in patients with CB with BO (90.6%), with CB and OBRС this symptom was recorded 1.4 and 2.9 times less often (65.9% and 31.4%). Dyspnea was recorded in all patients with CB with BO compared to children with CB (21.9%). The presence of oral wheezing was noted only in 100% of children with OBRС and in 95.3% of patients with CB with BO. Dry cough was noted in most cases in children with OBRС- 82.8%, almost 2 times less often with CB with BO (42.2%) and 3.8 times less often with CB (22.0%), which may indicate another distinctive feature in the clinical symptoms for children with OBRT. The presence of wet cough was typical for children with CB (78.0%), this symptom was 1.3 times less common in CB with BO (57.8%) and 4.5 times less common in children with OBRT (17.2%). During lung percussion, shortening was noted in 92.7% of cases with CB, in 9.4% of cases with CB with BO and during OBRT, shortening of the percussion sound was not determined. During auscultation, harsh breathing was determined in 100% of cases with OBRС, in 71.9% - with CB with BO and in 46.3% of children with CB. Weakened breathing was recorded only in CB (53.7%) and in patients with CB with BO (28.1%). Dry wheezing was heard mainly in 85.7% of children with OBRT, and in chronic bronchitis and chronic bronchitis with BO, wet wheezing was recor During the X-ray examination, the picture of the lungs in patients with CB depended on the severity of pathological changes - in 97.1% of patients with CB, an increase in the pulmonary pattern was detected, and in 60.3% of children, deformation of the bronchopulmonary pattern was detected.The results of the conducted studies of the microflora of the nasal mucosa showed that in most patients with CB with BO, compared with CB, Staphylococcus aureus was more common, isolated in 40.6%, in 21.9% − Streptococcus pneumonia, were sown less often: Moraxella catarrhalis - in 9.4%, yeast-like fungi of the genus Candida were sown in 4.9% (Fig. 1). The results of the conducted studies of the microflora of the mucous membranes from sputum showed that in most patients with CB with BO, compared with CB, microorganisms were more often isolated: Staphylococcus aureus, isolated in 37.5%, in 23.4% − Streptococcus pneumonia, were sown less often: Moraxella catarrhalis - in 12.5%, Candida albicans in combination with other bacterial pathogens. – 10.9%.
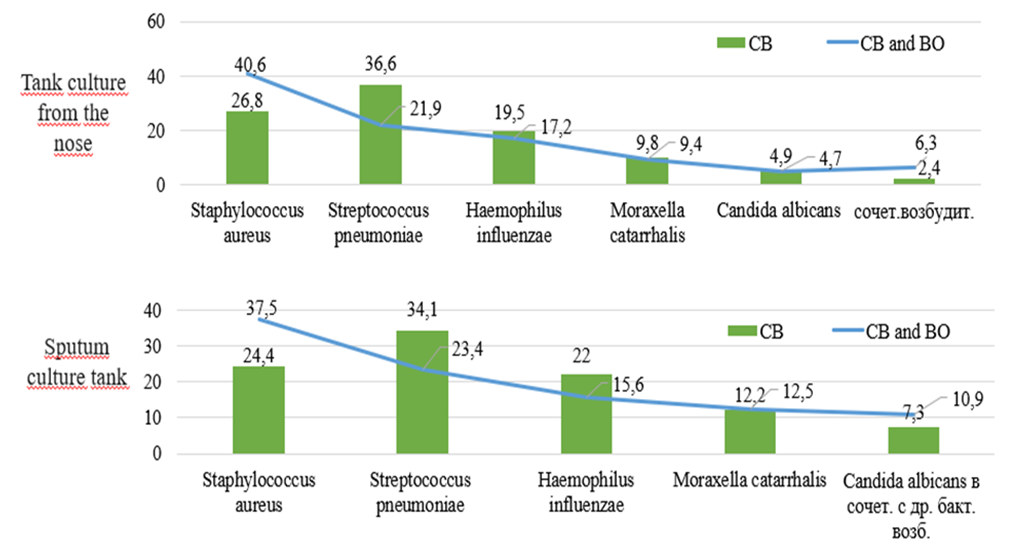 | Figure 1. Microbiota of the pharynx and bacterial culture of sputum in the examined children, (%) |
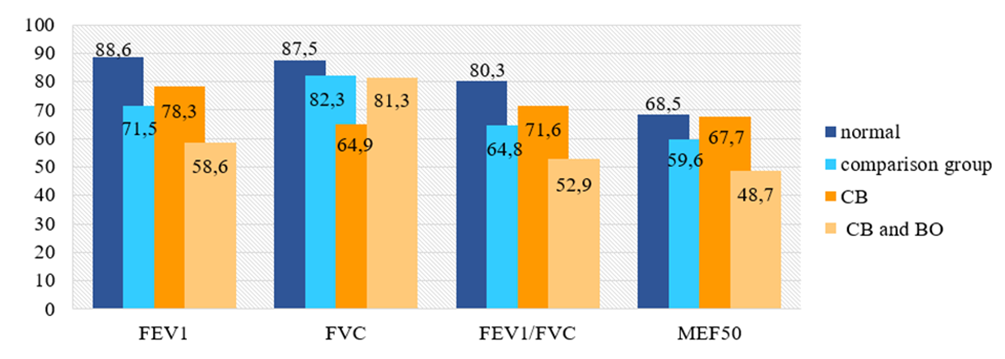 | Figure 2. Results of the FVD analysis in the examined children, (M±m) |
4. Conclusions
- 1. Microbiological study showed that in chronic bronchitis with bronchial obstruction, Staphylococcus aureus overgrowth was more often detected (in 40.6% of cases from the nose and in 37.5% of cases from sputum), while in chronic bronchitis, the most common pathogen was Streptococcus pneumoniae (in 36.6% of cases from the nose and in 34.1% of cases from sputum).2. When assessing the function of external respiration in children with chronic bronchitis, a restrictive type of disorder was noted in 58.5% of cases, which was 5.1 times higher than the indicators of the comparison group. These children also showed a reliable decrease in the level of vital capacity by 1.3 times (p < 0.001). In children with chronic bronchitis with bronchial obstruction, the obstructive type of disorder was detected in 70.3% of cases, which was 1.3 times higher than the indicators of the comparison group. In addition, this group of children showed a reliable decrease in FEV1 by 1.2 times, as well as a reliable decrease in the FEV1/VC ratio by 1.2 times in relation to the comparison group (p from <0.05 to <0.01).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML