-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2273-2274
doi:10.5923/j.ajmms.20241409.32
Received: Aug. 8, 2024; Accepted: Sep. 5, 2024; Published: Sep. 18, 2024

The State of Carbohydrate Metabolism in Patients with Prediabetes
Komiljonova Kamilla Valizhonovna, Kamalov Telman Tolyaganovich
Republican Scientific and Practical Medical Center of Endocrinology, Tashkent, Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Prediabetes is a condition in which people have blood glucose levels that are higher than normal, but not high enough to be classified as diabetes. People with prediabetes have an increased risk of developing type 2 diabetes. An estimated 34% of adults have prediabetes. Prediabetes is now recognized as a reversible condition that increases a person's risk of developing diabetes. Lifestyle-related risk factors for prediabetes include being overweight and being physically inactive.
Keywords: Prediabetes, Cholesterol, Carbohydrate metabolism
Cite this paper: Komiljonova Kamilla Valizhonovna, Kamalov Telman Tolyaganovich, The State of Carbohydrate Metabolism in Patients with Prediabetes, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2273-2274. doi: 10.5923/j.ajmms.20241409.32.
1. Introduction
- Currently, there are more than 537 million patients with type 2 diabetes mellitus (T2DM) and about 850 million with initial carbohydrate metabolism disorders in the world. Given the constant increase in the number of new cases of carbohydrate metabolism disorders, their timely diagnosis is extremely important, especially in the early stages [1].Management of patients with prediabetes primarily involves lifestyle modification aimed at weight loss. If lifestyle modification is insufficiently effective, drug therapy may be advisable. At the same time, given the high risk of cardiovascular disease in patients with prediabetes, correction of such classic risk factors for atherosclerosis as arterial hypertension and dyslipidemia is necessary [1]. It should be noted that normalization of glycemia in patients with prediabetes reduces the risk of not only cardiovascular events in the future, but also, possibly, microangiopathies.Currently, the global epidemic of type 2 diabetes is acquiring the character of a growing pandemic. Type 2 diabetes is one of the highest priority problems facing the health care of almost all countries in the world. This is due to the high risk of complications and mortality, as well as high disability of patients [2,3]. According to the World Health Organization, there are currently approximately 425 million patients with type 2 diabetes in the world, by 2035 this number will increase to 592 million. Every year, 5 million people die worldwide from causes related to type 2 diabetes. Given the constant increase in the number of new cases of carbohydrate metabolism disorders, their timely diagnosis is extremely important, especially in the early stages [4]. Prediabetes is a metabolic condition that predisposes to the development of type 2 diabetes. People with prediabetes, in addition to the high risk of developing type 2 diabetes, have an increased risk of developing retinopathy, nephropathy, neuropathy and cardiovascular diseases (CH)D by 1.9 times, ischemic stroke by 2.2 times), the risk of developing non-alcoholic fatty liver disease (NAFLD) increases significantly. IFG – impaired fasting glycemia IGT – impaired glucose tolerance DM – carbohydrate metabolism disorders.
2. Material and Methods
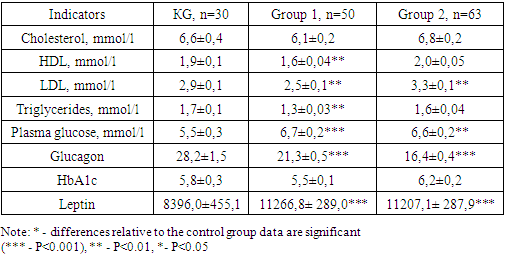
- The examined patients with prediabetes were divided into 2 groups: Group 1 consisted of 50 patients with impaired fasting glycemia (IFG), Group 2 – of 63 patients with impaired glucose tolerance (IGT). For adequate assessment of the degree of impairment of the parameters, a control group of practically healthy people without impaired carbohydrate metabolism (ICM) was formed. Biochemical blood analysis included determination of glucose level; determination of blood levels of total cholesterol, low-density lipoproteins (LDL), high-density lipoproteins (HDL), triglycerides (TG). Blood for biochemical analysis was taken in the morning on an empty stomach after 8–10 hours of overnight fasting. After blood clotting, it was centrifuged at room temperature for 15 minutes at a speed of 1500 rpm. The obtained blood serum was analyzed using an Architect c4000 biochemical analyzer (Abbott Diagnostics, Abbott Park, IL, USA) using the manufacturer's standard reagent kits.
3. Results and Discussion
- The incidence of prediabetes significantly exceeds the registered rate and has actually reached pandemic proportions in a number of regions, varying in different populations and age groups. Therefore, the timely implementation of screening programs to detect early carbohydrate metabolism disorders, optimization of type 2 diabetes risk scales, and identification of new predictors of high risk of type 2 diabetes in individuals with existing risk factors (e.g., overweight, obesity, or prediabetes) are extremely relevant today and have important medical and social significance.As a result of the oral glucose tolerance test (OGTT), prediabetes was diagnosed in 113 people. In patients with prediabetes, the average HbA1c value was 5.9 ± 0.4%. At the same time, the average HbA1c value in people with IFG was 5.6 (0.3), in people with IGT 6.1 (0.3), in people without NMDA - 5.7 (0.4). The negative predictive value (NPV) of using HbA1c for diagnosing prediabetes was low - 17% (95% CI: 6-33). As part of laboratory studies, blood lipid profile parameters were assessed in all patients. In general, the group of patients with IFG and people without NMDA were characterized by a more favorable lipid profile compared to the groups with type 2 diabetes and IGT. Triglyceride and LDL levels increased as the severity of HF increased (Table 1).
|
4. Conclusions
- Given the growing number of patients with carbohydrate metabolism disorders, the relevance of the problem of timely diagnosis of these conditions is obvious. Early detection of the risk of developing diabetes mellitus in patients from the prediabetes group is extremely important.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML