-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2242-2244
doi:10.5923/j.ajmms.20241409.24
Received: Aug. 16, 2024; Accepted: Sep. 1, 2024; Published: Sep. 18, 2024

Successful Treatment of Acute Liver Failure Caused by Alcohol Associated Liver Disease: A Case Report from Ferghana, Uzbekistan
Rakhimov Anvarjon Aliyorovich1, 2, Khalilov Azizjon Marufjonovich1, 2, Baltabayev Alisher Murodilovich1, 2, Djurayev Jasur Ravshanovich3
1Department of Internal Medicine, Central Asian Medical University, Ferghana, Uzbekistan
2Hospital of Central Asian Medical University, Uzbekistan
3Department of Preventive Service, Kyoto University, Japan
Correspondence to: Rakhimov Anvarjon Aliyorovich, Department of Internal Medicine, Central Asian Medical University, Ferghana, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Acute liver failure (ALF) resulting from alcohol associated liver disease poses significant clinical challenges in Ferghana, Uzbekistan. This paper presents a case report of a 41-year-old male with ALF secondary to alcohol associated liver disease, managed successfully at the Hospital of Central Asian Medical University. The patient exhibited typical symptoms of jaundice, ascites and moderate hepatic ecephalopathy(stage 2) upon admission, with laboratory findings confirming severe liver dysfunction(total bilirubin: 548 µmol/L (conjugated: 396 µmol/L, unconjugated: 152 µmol/L, ALT (alanine aminotransferase): 56 U/L, AST (aspartate aminotransferase): 175 U/L, WBC (white blood cell count): 35.0 × 10^9/L, ESR (erythrocyte sedimentation rate): 32 mm/hour.) Treatment involved a multidisciplinary approach including pharmacological therapy with prednisolone(1mg/kg), azathioprine(50mg/day), and rifaximin(800 mg/day), alongside supportive care with diuretics and albumin. Clinical outcomes demonstrated a marked improvement in liver function and resolution of acute liver failure over a four-month period, highlighting the effectiveness of early intervention and comprehensive management strategies.
Keywords: Acute liver failure, Alcoholic fatty liver disease, Jaundice, Ascites, Pharmacological therapy, Supportive care
Cite this paper: Rakhimov Anvarjon Aliyorovich, Khalilov Azizjon Marufjonovich, Baltabayev Alisher Murodilovich, Djurayev Jasur Ravshanovich, Successful Treatment of Acute Liver Failure Caused by Alcohol Associated Liver Disease: A Case Report from Ferghana, Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2242-2244. doi: 10.5923/j.ajmms.20241409.24.
1. Introduction
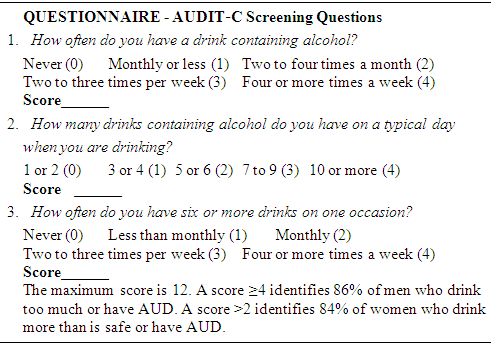
- Acute liver failure is a rare but life-threatening critical illness that occurs most often in patients who do not have preexisting liver disease. With an incidence of fewer than 10 cases per million persons per year in the developed world, acute liver failure is seen most commonly in previously healthy adults in their 30s and presents unique challenges in clinical management. The clinical presentation usually includes hepatic dysfunction, abnormal liver biochemical values, and coagulopathy; encephalopathy may develop, with multiorgan failure and death occurring in up to half the cases. [1] The alcohol associated liver disease covers a spectrum of disorders beginning from the fatty liver, progressing at times to alcoholic hepatitis and culminating in alcoholic cirrhosis, which is the most advanced and irreversible form of liver injury related to the consumption of alcohol. [2]This case study aims to explore the clinical course, management strategies, and outcomes of ALF due to alcohol associated liver disease in a hospital setting in Ferghana, Uzbekistan.Setting:The study was conducted at the Hospital of Central Asian Medical University, Ferghana, Uzbekistan. This tertiary care hospital serves a diverse patient population, including those with acute and chronic liver diseases, with a focus on multidisciplinary care and medical education.Case Presentation:Patient Background: 41-year-old male with a history of chronic alcohol abuse (QUESTIONNAIRE -AUDIT-C screening questions).
 Presented with jaundice and ascites, moderate hepatic encephalopathy (stage 2) indicative of severe liver dysfunction. [3]Clinical Course:Physical Examination: General: Patient appears lethargic and disoriented. Skin: Jaundiced, with yellowish discoloration of the skin and sclerae. Abdomen: Distended abdomen with shifting dullness and fluid wave suggestive of ascites.Neurological Examination: Evidence of moderate hepatic encephalopathy, including altered consciousness, confusion, and impaired cognitive function (stage 2 on West Haven criteria).Laboratory results:Upon admission, laboratory results confirmed acute liver failure (ALF) indicated by significantly elevated bilirubin levels, liver enzymes, and inflammatory markers. Initial measurements showed a total bilirubin of 548 µmol/L, with conjugated bilirubin at 396 µmol/L and unconjugated bilirubin at 152 µmol/L. Alanine Aminotransferase (ALT) was 56 U/L, Aspartate Aminotransferase (AST) was 175 U/L, White Blood Cell Count (WBC) was 35.0 × 10^9/L, and Erythrocyte Sedimentation Rate (ESR) was 32 mm/hour.After one week of therapy, there was a noted improvement, with total bilirubin decreasing to 403 µmol/L (conjugated: 212 µmol/L, unconjugated: 191 µmol/L), ALT at 108 U/L, AST at 77 U/L, WBC remained elevated at 35 × 10^9/L, and ESR decreased to 22 mm/hour.By two months, there was further improvement in liver function: total bilirubin reduced to 192 µmol/L (conjugated: 138 µmol/L, unconjugated: 54 µmol/L), ALT was 108 U/L, AST slightly elevated to 111 U/L, WBC decreased to 18.2 × 10^9/L, and ESR further decreased to 20 mm/hour.After four months, significant recovery was evident with total bilirubin normalizing to 26 µmol/L (conjugated: 12 µmol/L, unconjugated: 14 µmol/L), ALT at 44 U/L, AST at 45 U/L, WBC decreased to 7.1 × 10^9/L, and ESR decreased to 18 mm/hour. These sequential improvements indicate successful management of the acute liver failure over the course of treatment.Diagnosis:Acute Liver Failure (ALF) Diagnosis:Criteria met: rapid onset of jaundice, ascites, hepatic ecephalopathy, and severe liver dysfunction. [4]Underlying cause confirmed as alcohol associated liver disease based on patient history and imaging studies.Management:Treatment Protocol:Pharmacological Therapy: Prednisolone: Initially started at 1 mg/kg/day with a gradual tapering regimen to manage inflammation associated with the liver condition.Azathioprine: Prescribed at a daily dose of 50 mg to suppress the immune response and prevent further liver damage.Rifaximin: Administered at a daily dose of 800 mg to prevent hepatic encephalopathy, a complication involving cognitive impairment due to liver dysfunction.Supportive Care:Albumin: Given as a 20% solution to expand blood volume and provide oncotic support, aiding in the management of fluid balance and preventing complications like spontaneous bacterial peritonitis.Diuretics: Spironolactone: Administered daily at 200 mg to reduce fluid retention and manage ascites, a common symptom of liver cirrhosis.Furosemide: Used daily at 80 mg to promote diuresis and further manage fluid overload.Monitoring: Continuous assessment for signs of hepatic encephalopathy, with prompt intervention using lactulose to manage elevated ammonia levels and prevent neurological complications.Clinical Course and OutcomesProgression Over Time:Improvement in Liver Function: Regular monitoring of liver function tests shows progressive improvement, indicating reduced inflammation and enhanced hepatic function.Resolution of Ascites and Jaundice: Effective management with diuretics and albumin has led to the gradual resolution of ascites (abdominal fluid accumulation) and jaundice (yellowing of the skin and eyes due to bilirubin buildup).Reduction in Total Bilirubin Levels: Continuous treatment has resulted in a gradual decrease in total bilirubin levels, reflecting improved liver function and clearance of bilirubin from the bloodstream.Overall Management Strategy:This comprehensive management approach integrates pharmacological therapies, supportive care measures, and procedural interventions tailored to address the specific challenges posed by the patient's liver condition. Regular monitoring and adjustment of treatment protocols based on clinical responses are essential to optimize outcomes and prevent disease progression. The observed clinical improvements underscore the effectiveness of the multidisciplinary management plan in mitigating symptoms and enhancing quality of life for the patient. Continued vigilance and adherence to the treatment regimen are crucial to sustain these positive outcomes over the long term.
Presented with jaundice and ascites, moderate hepatic encephalopathy (stage 2) indicative of severe liver dysfunction. [3]Clinical Course:Physical Examination: General: Patient appears lethargic and disoriented. Skin: Jaundiced, with yellowish discoloration of the skin and sclerae. Abdomen: Distended abdomen with shifting dullness and fluid wave suggestive of ascites.Neurological Examination: Evidence of moderate hepatic encephalopathy, including altered consciousness, confusion, and impaired cognitive function (stage 2 on West Haven criteria).Laboratory results:Upon admission, laboratory results confirmed acute liver failure (ALF) indicated by significantly elevated bilirubin levels, liver enzymes, and inflammatory markers. Initial measurements showed a total bilirubin of 548 µmol/L, with conjugated bilirubin at 396 µmol/L and unconjugated bilirubin at 152 µmol/L. Alanine Aminotransferase (ALT) was 56 U/L, Aspartate Aminotransferase (AST) was 175 U/L, White Blood Cell Count (WBC) was 35.0 × 10^9/L, and Erythrocyte Sedimentation Rate (ESR) was 32 mm/hour.After one week of therapy, there was a noted improvement, with total bilirubin decreasing to 403 µmol/L (conjugated: 212 µmol/L, unconjugated: 191 µmol/L), ALT at 108 U/L, AST at 77 U/L, WBC remained elevated at 35 × 10^9/L, and ESR decreased to 22 mm/hour.By two months, there was further improvement in liver function: total bilirubin reduced to 192 µmol/L (conjugated: 138 µmol/L, unconjugated: 54 µmol/L), ALT was 108 U/L, AST slightly elevated to 111 U/L, WBC decreased to 18.2 × 10^9/L, and ESR further decreased to 20 mm/hour.After four months, significant recovery was evident with total bilirubin normalizing to 26 µmol/L (conjugated: 12 µmol/L, unconjugated: 14 µmol/L), ALT at 44 U/L, AST at 45 U/L, WBC decreased to 7.1 × 10^9/L, and ESR decreased to 18 mm/hour. These sequential improvements indicate successful management of the acute liver failure over the course of treatment.Diagnosis:Acute Liver Failure (ALF) Diagnosis:Criteria met: rapid onset of jaundice, ascites, hepatic ecephalopathy, and severe liver dysfunction. [4]Underlying cause confirmed as alcohol associated liver disease based on patient history and imaging studies.Management:Treatment Protocol:Pharmacological Therapy: Prednisolone: Initially started at 1 mg/kg/day with a gradual tapering regimen to manage inflammation associated with the liver condition.Azathioprine: Prescribed at a daily dose of 50 mg to suppress the immune response and prevent further liver damage.Rifaximin: Administered at a daily dose of 800 mg to prevent hepatic encephalopathy, a complication involving cognitive impairment due to liver dysfunction.Supportive Care:Albumin: Given as a 20% solution to expand blood volume and provide oncotic support, aiding in the management of fluid balance and preventing complications like spontaneous bacterial peritonitis.Diuretics: Spironolactone: Administered daily at 200 mg to reduce fluid retention and manage ascites, a common symptom of liver cirrhosis.Furosemide: Used daily at 80 mg to promote diuresis and further manage fluid overload.Monitoring: Continuous assessment for signs of hepatic encephalopathy, with prompt intervention using lactulose to manage elevated ammonia levels and prevent neurological complications.Clinical Course and OutcomesProgression Over Time:Improvement in Liver Function: Regular monitoring of liver function tests shows progressive improvement, indicating reduced inflammation and enhanced hepatic function.Resolution of Ascites and Jaundice: Effective management with diuretics and albumin has led to the gradual resolution of ascites (abdominal fluid accumulation) and jaundice (yellowing of the skin and eyes due to bilirubin buildup).Reduction in Total Bilirubin Levels: Continuous treatment has resulted in a gradual decrease in total bilirubin levels, reflecting improved liver function and clearance of bilirubin from the bloodstream.Overall Management Strategy:This comprehensive management approach integrates pharmacological therapies, supportive care measures, and procedural interventions tailored to address the specific challenges posed by the patient's liver condition. Regular monitoring and adjustment of treatment protocols based on clinical responses are essential to optimize outcomes and prevent disease progression. The observed clinical improvements underscore the effectiveness of the multidisciplinary management plan in mitigating symptoms and enhancing quality of life for the patient. Continued vigilance and adherence to the treatment regimen are crucial to sustain these positive outcomes over the long term.2. Discussion
- Comparing our management approach with findings from the literature reveals significant insights into the treatment of liver diseases similar to the present case. Research highlights diverse therapeutic protocols and their respective outcomes, underscoring the need for personalized treatment strategies based on disease severity and patient response. [5]Studies exploring cases akin to ours underscore the efficacy of interventions such as corticosteroids like Prednisolone, immunosuppressants such as Azathioprine, and antibiotics like Rifaximin for prophylaxis against hepatic encephalopathy. [6] These approaches align with our regimen, focusing on mitigating inflammation and preventing complications.Geographical disparities influence treatment accessibility and guideline adherence, impacting patient outcomes significantly. For instance, access to liver transplantation and advanced diagnostic tools varies widely between developed and developing regions. [7] Understanding these discrepancies informs global health strategies aimed at improving equity in liver disease management.Challenges and Lessons Learned:Management of Complications Such as Ascites and Hepatic Encephalopathy:Effective management of ascites includes the careful administration of diuretics like Spironolactone and Furosemide, complemented by therapeutic paracentesis when indicated. [8] Hepatic encephalopathy necessitates vigilant monitoring and timely treatment with lactulose to reduce ammonia levels and mitigate cognitive impairment. [9]Importance of Early Diagnosis and Multidisciplinary Care:Early diagnosis through comprehensive liver function tests and imaging studies is pivotal for initiating timely interventions and improving prognosis. [10] Multidisciplinary care involving hepatologists, gastroenterologists, pharmacists, and nutritionists ensures holistic management addressing both disease progression and associated complications.
3. Conclusions
- In conclusion, the management of complex liver diseases demands a tailored approach integrating evidence-based therapies, supportive care, and procedural interventions. By leveraging insights from literature and addressing regional variations, healthcare providers can optimize treatment strategies to enhance patient outcomes effectively. Challenges such as ascites and hepatic encephalopathy underscore the necessity for proactive monitoring and collaborative care, ultimately improving quality of life for patients with liver conditions worldwide. Recommendations:Clinical Implications:Emphasize early intervention and comprehensive management strategies in similar cases.Promote further research into tailored therapies for alcohol associated liver disease associated acute liver failure.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML