B. Kh. Mukhiddinov, Z. B. Kurbaniyazov, P. A. Askarov
Samarkand State Medical University, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The aim of the study was to improve surgical treatment results of patients with gallstone disease and realized intermediate risk of choledocholithiasis. The clinical material based on the results of complex examination and treatment of 107 patients with complicated forms of cholelithiasis, in particular choledocholithiasis, was analyzed. A comparative analysis of the implementation of the standard two-stage and improved one-stage methods of laparoendoscopic correction of choledocholithiasis was carried out. The duration of surgical interventions, hospital stay, and intra- and postoperative complications were taken as comparative parameters. Based on the results of our study, it should be noted that the use of modified one-stage technique of laparoscopic cholecystectomy with the performance of assisted endoscopic papillosphincterotomy in the Rendezvous technique and choledocholithoextraction in patients with cholecystocholedocholithiasis improves the results of surgical treatment and is economically feasible, as it reduces the number of surgeries and hospitalizations for the patient.
Keywords:
Cholelithiasis, Choledocholithiasis, Cholecystectomy, Choledocholithoextraction, Papillosphincterotomy, Rendezvous technique, Laparoendoscopic rendezvous
Cite this paper: B. Kh. Mukhiddinov, Z. B. Kurbaniyazov, P. A. Askarov, Efficiency of Modified Laparoendoscopy Technique in the Treatment of Patients with Cholecistocholedocholithiasis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2210-2214. doi: 10.5923/j.ajmms.20241409.17.
1. Introduction
Gallstone disease (GSD) is one of the most common diseases of the abdominal organs [1]. One form of GSD is cholecystocholedocholithiasis (CCL), which is characterized by the simultaneous presence of stones in the gallbladder and in the common bile duct [2]. According to different authors, the combination of gallbladder and common bile duct stones may occur in 2.8-19% of patients with symptomatic GSD [3].It is thought that once stones are found in the common bile duct, they should be removed to prevent the development of complications. Such diseases as pancreatitis, cholangitis or obstruction of bile ducts with the development of mechanical jaundice syndrome are severe complications of cholangiolithiasis [4-5].In a moderate risk group for the presence of cholangiolithiasis, only 10-50% of cases may actually have it [6]. Most often, intraoperative cholangiography (ICG) is performed in such patients to exclude or confirm the presence of biliary ductal concrements during laparoscopic cholecystectomy (LCE), especially in emergency patients with acute cholecystitis [7-8].The introduction of minimally invasive technologies, such as laparoscopic cholecystectomy, mini-lap cholecystectom, allowed not only to change the strategy of treatment of cholecystocholedocholithiasis, but also in most cases to use minimally invasive techniques for the removal of concrements to resolve choledocholithiasis: endoscopic papillosphincterotomy (EPST) with choledocholithoextraction [9].Currently, the two-stage tactics of treatment of patients with cholecystocholedocholithiasis is generally accepted and can be applied in two options:The 1st option: first of all, a transpapillary intervention is performed (EPST with choledocholite extraction), then cholecystectomy is performed in a delayed order;The 2nd option: first cholecystectomy with drainage of the choledochus is performed, followed by transfistula or transpapillary sanitation of the biliary tract [10].One-stage treatment of patients with combined gallbladder and common bile duct stones is an attractive alternative to the two-stage technique. The technique is economically feasible, as it reduces the duration of inpatient treatment, decreases the number of surgeries per patient, reduces the risk of developing EPST-associated complications and has a higher success rate of hepaticocholedochal sanitation [11].There are several types of single-stage treatment for patients with cholecystocholedocholithiasis. One form of such surgical treatment is laparoendoscopic rendezvous (LER). LER is a one-stage combined laparoscopic and transpapillary endoscopic approach to common bile duct stone. Surgical intervention is an efficient alternative to sequential treatment, which, in addition, minimizes the risk of inadvertent retrograde cannulation and contrast of the main pancreatic duct and thus reduces the risk of postoperative pancreatitis. The advantages of the LER approach have been outlined by a large number of authors who have used and analyzed this mode of surgical intervention. The most important advantages compared with the more popular two-stage treatment (endoscopic retrograde cholangiopancreatography (ERCP) with EPST, followed by laparoscopic cholecystectomy) are a reduced complication rate, especially postoperative pancreatitis, a higher success rate and a shorter hospital stay [9,12].The aim of the study was to improve surgical treatment results of patients with gallstone disease and realized intermediate risk of choledocholithiasis.
2. Material and Methods
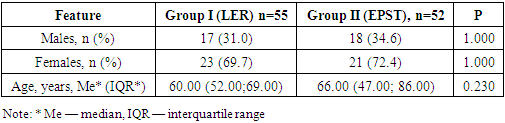
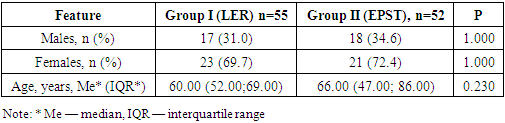
107 patients with cholecystocholangiolithiasis who were treated at the multidisciplinary clinic of Samarkand State Medical University for the period from 2017 to 2023 were included in the study. The patients were divided into 2 groups as follows: Group I consisted of 55 patients who underwent hybrid surgical intervention - laparoscopic cholecystectomy and assisted endoscopic papillosphincterotomy using the Rendezvous technique with choledocholithoextraction (LER group).Group II consisted of 52 patients in whom transapillary intervention - endoscopic papillosphincterotomy with choledocholithoextraction (EPST group) was performed to remove concrements from the common bile duct. The distribution of patients by gender and age are presented in Table 1.Table 1. The distribution of patients by gender and age
 |
| |
|
Women predominated in both study groups: 23 (69.7%) in Group I and 21 (72.4%) in Group II. In Group I, the male-to-female ratio was 1:2.3 (30.3% and 69.7%, respectively), while in Group II it was 1:2.6 (27.6% and 72.4%, respectively). By gender, the study groups were comparable; p= 1.000. The age of the patients included in the study ranged from 22 to 92 years. In the first group, patients' age ranged from 22 to 85 years, with a median of 59.00 (IQR 54.00; 68.00); in the second group, patients' age ranged from 22 to 92 years, with a Me of 69.00 (IQR 46.00; 84.00). The age structure in the studied groups was comparable; p= 0.230.In patients of Group I the correction of cholecystocholedocholithiasis was performed according to the modified method of hybrid laparoendoscopic surgical intervention using the Rendezvous technique, without using the radiologic complex. During this surgical intervention, the gallbladder was removed laparoscopically and the common bile duct was sanitized by endoscopic access through the papilla duodeni major.Two surgical teams, surgical and endoscopic, participated in the surgery. The intervention was performed under general anesthesia with tracheal intubation and ventilation. The patient was placed on the operating table in a supine position with legs apart (“French position”), thoracic region elevated 15-20 degrees (G.R. Fowler position), with a slight tilt of 10-15 degrees of the operating table to the left.The teams were arranged so that the relationship of the axes of observation and surgical exposure of neither the surgeon nor the endoscopist changed compared with standard surgical interventions (Figure 1).  | Figure 1. Location of operating teams and equipment |
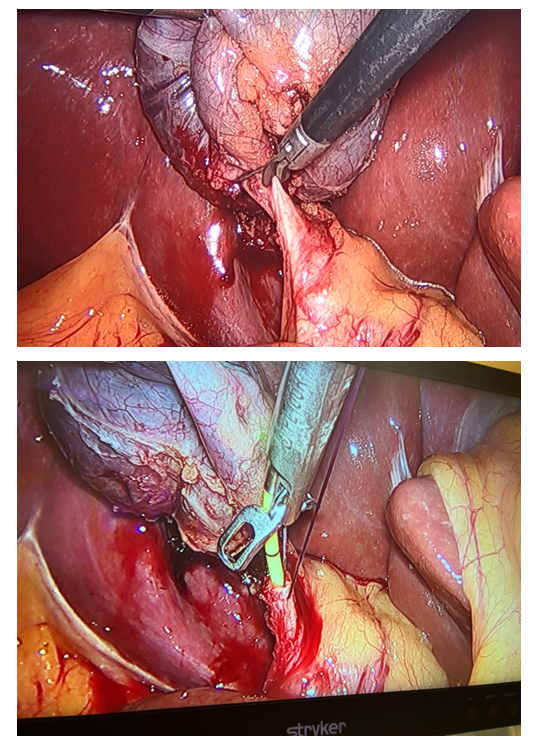
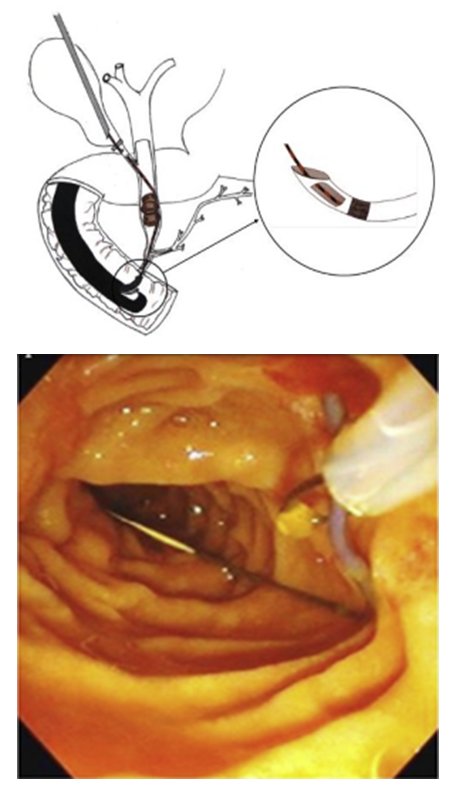
In addition, the surgeon could comfortably control the endoscopist's manipulations by observing his actions in the endoscopy stand monitor.The surgical intervention was conventionally divided into four consecutive stages: 1) the first laparoscopic stage; 2) the joint laparoscopic and endoscopic team (Rendezvous) stage; 3) the endoscopic stage; 4) the second laparoscopic stage.Abdominal puncture was performed paraumbilically above the umbilical ring with a Veress needle. To control the passage of the anterior abdominal wall, the “double click” method was used, then pneumoperitoneum was applied until the resting pressure reached 12 mm Hg. We placed four trocars at typical points for performing cholecystectomy. We performed dissection of anatomical structures in the area of the gallbladder neck (Calot's triangle). The visceral peritoneum was opened up to the middle of the gallbladder, the gallbladder neck and body were separated from the liver bed. After isolation of the vesical artery, it was clipped with a 5 mm titanium clip and crossed with an L-shaped hook using monopolar cutting. Next, the cystic duct was isolated at its maximum length. During the second stage of the surgical intervention (Rendezvous), joint work of the surgical and endoscopic teams was necessary. The surgeon made an incision in the cystic duct just below the previously applied clip and inserted a 0.035 Fr endoscopic wire 450 cm long into the cystic duct through a 3 mm diameter trocar. Then he passed it antegradely through the papilla duodeni major into the lumen of the duodenum (Figure 2). 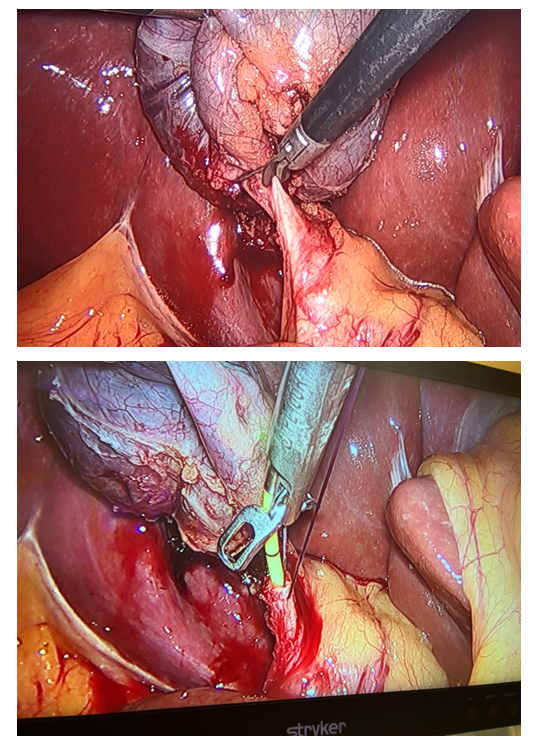 | Figure 2. Insertion of an endoscopic string into the lumen of the duodenum |
After the string was passed through the papilla duodeni major, the endoscopist routinely passed the videoduodenoscope into the duodenum and visualized the papilla duodeni major with the string in its lumen. From the side of the duodenal lumen, the string was captured with a modified hollow endoscopic bougie (Figure 3).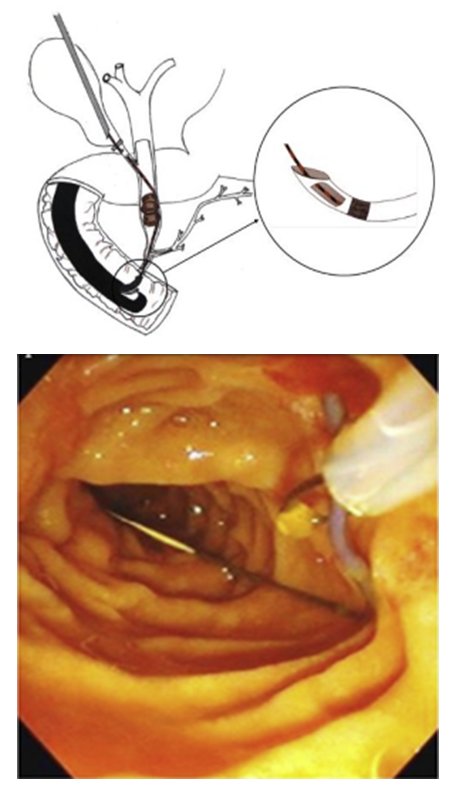 | Figure 3. Catching the string in the lumen of the duodenum |
The papillotome was lowered along the string and inserted into the ampulla of the papilla duodeni major, thus performing selective intubation of the common bile duct. Retrograde endoscopic papillosphincterotomy (EPST) was performed in a standard manner. The papillotome was then removed, leaving an endoscopic string in the bile ducts. After removal of the biliary duct stones, the surgical team was again involved in the surgery. All patients were performed nasobiliary drainage. During the fourth stage, laparoscopic cholecystectomy “from the neck up” was performed. To perform the surgery we used the endovideoscope unit Karl Storz TELECAM SL II, Germany; endoscopic halogen illuminator Karl Storz HALOGEN 150, Germany; carbon dioxide insufflator with microprocessor control system and self-testing INS-002 by “Fotek”, Russia; surgical aspirator AIH6-01 by Fotek, Russia; portable high-vacuum aspirator Eschman VP-25, Germany; universal multipurpose coagulator FORCE FX by Medtronic, Germany.To perform the transduodenal stage, we used the EVIS EXERA III endoscopic system with TJF-Q180V video duodenoscope with a 4.2 mm working channel, OLYMPUS, Japan; electrosurgical high-frequency generator EGS-100 OLYMPUS, Germany.Categorical variables were presented as absolute numbers and percentages, continuous variables are presented as Me (median) and IQR (interquartile range). Fisher's exact test was used to evaluate qualitative traits. In analyzing quantitative data, Shapiro-Wilk normality test was used to test for the presence of normal distribution. Mann-Whitney U-test was used to compare continuous data due to the lack of conditions to apply parametric criteria.Statistical processing of the data was carried out using the statistical program EZR (R commander version 2.5-1, EZR version 1.38 dated by 01.02.2019).
3. Results and Discussion
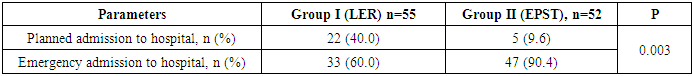
The majority of patients (n=47(75.8%)) were hospitalized for emergency reasons, which to a certain extent indicates the relevance of the problem of cholecystocholedocholithiasis and characterizes the difficulties in treating such patients. In Group I (LER), the ratio of planned to emergency patients was 1:1.5; in Group II (EPST), the proportion of emergency patients was significantly higher at 93.1%. This difference was due to the fact that patients in the EPST group received surgical care 24 hours a day, while patients in the LER group were operated on during the daytime with a narrow range of experienced specialists who were part of the combined team (Table 2).Table 2. The distribution of patients according to the order of care
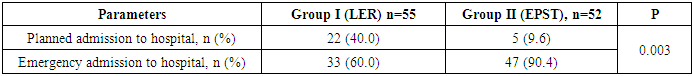 |
| |
|
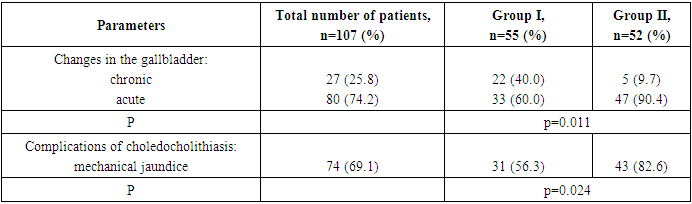
In Group I, the number of patients with acute changes in the gallbladder wall prevailed over chronic ones (60.6% and 39.4%, respectively). The main part (89.7%) in Group II consisted of patients with catarrhal changes in the gallbladder. According to the character of changes in the gallbladder wall the groups were not comparable; p = 0.011.All patients in both groups belonged to the group with medium risk of cholangiolithiasis development (Table 3).Table 3. Characteristics of gallstone disease in groups of patients
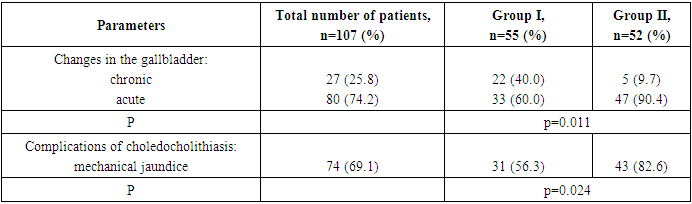 |
| |
|
According to the main characteristics taken into account, namely gender, age, presence of concomitant pathology, severity of inflammatory syndrome in the blood, levels of amylase, urea, PTI, diameter of the common hepatic duct, size of stones, both groups were statistically comparable.The obtained differences - by the order of admission to hospital, severity of inflammation in the gallbladder wall, bilirubin level in blood serum do not interfere with the assessment of the treatment result on the development of postoperative EPST associated complications and the severity of their course.The intraoperative period in the LER and EPST groups was compared in terms of duration of endoscopic papillosphincterotomy with choledocholithoextraction; intraoperative complications associated with the transpapillary stage.In the LER group, the mean duration of EPST with choledocholithoextraction was 15.0 (IQR 10.0; 20.0) minutes. In the EPST group, the mean time to perform sphincterotomy with stone removal from the common bile duct was 30.0 minutes (IQR 20.0; 45.0). Thus, a statistically significant average of 2 times less time was required to perform the transpapillary step at LER (р < 0.001).Intraoperative complications associated with endoscopic retrograde papillosphincterotomy (bleeding, intraoperative "wedge" of the basket with a calculus, retroduodenal perforation) were not observed in both groups.Postoperative period course in LER and EPST groups was compared according to the presence and severity of postoperative complications associated with the transpapillary stage; frequency of staying in ICU and duration of ICU stay; success of biliary tract sanation; duration of hospital stay.In all 55 patients of Group I, no risk factors for pancreatitis related to the technique of transpapillary intervention were identified. Most risk factors for postmanipulation pancreatitis are associated with retrograde impact on the papilla duodeni major, which is excluded when performing EPST in the Rendezvous technique.Thus, the analysis revealed statistically significant differences in the incidence of total postoperative complications between the groups (p=0.017) and the development of postoperative EPST-associated pancreatitis (p=0.044). When preoperative EPST was performed, the chance of developing postoperative complications increased 6.98 times (95% CI: 1.4-35.7) and the chance of developing postoperative pancreatitis increased 8.35 times (95% CI: 0.94-74.1), indicating the safety of the laparoendoscopic rendezvous technique and superiority over standard endoscopic papillosphincterotomy.In the ICU department, 10 (18.2%) patients from the LER group and 2 (3.6%) patients from the EPST group were observed after surgery (р=0.109). The mean duration of patient's stay in ICI was 1.0 (IQR 1.0; 1.0) in both groups (р=0.683). The SOFA index of patients admitted to the ICU in the LER group averaged 3.0 points (IQR 1.25; 4.0) and in the EPST group — 3.0 (IQR 3.0; 3.0) (р=1.000). In both groups, the SOFA index has a low score, indicating low severity of multiorgan failure. The APACHE II score of resuscitation patients in both groups also gave us a low score of 9.00 (IQR 8.00; 12.25) and 11.0 (IQR 11.0; 11.0) in the LER and EPST groups, respectively (p=0.614), indicating a low prognosis for an unfavorable outcome.Endoscopic papillotomy was performed in all patients of both groups, no failures of this stage of transpapillary intervention were observed.The success rate of biliary tract sanation in one stage in the LER group was statistically higher and made up 85.7% (n=47), in the EPST group this indicator was 67.7% (n=35) (р=0.035).In 8 (14.3%) patients of the LER group and in 15 (29.1%) patients of the EPST group, complete sanitation could not be achieved during primary transpapillary intervention.The duration of hospital stay of patients in the laparoendoscopic rendezvous group ranged from 4 to 14 days, EPST group - from 4 to 21 days. The average bed-day in the main group was 7.0 days (IQR 6.0; 8.0), and in the EPST group - 8.0 days (IQR 5.0; 11.0) (р=0.100).In 29 (87.9%) patients of the LER group and in 20 (69.0%) patients of the EPST group, the postoperative period was uneventful; all of them were discharged in satisfactory condition under the supervision of a surgeon and gastroenterologist at their place of residence. The mean hospital stay for these patients in the LER group was 6.0 bed days (IQR 5.0; 8.0) and in the EPST group it was 7.5 bed days (IQR 5.0; 9.25). The development of postoperative complications in 4 (12.1%) patients of the LER group resulted in a statistically significant increase in hospital stay to 13.0 bed days (IQR 11.5; 14.0) (р=0.003). In 9 (31.0%) patients of the EPST group, the development of complications did not lead to a statistically significant prolongation of hospital stay and amounted to 10.0 bed days (IQR 7.0; 16.0) (р=0.274).
4. Conclusions
Based on the results of our study, it should be noted that the use of modified one-stage technique of laparoscopic cholecystectomy with the performance of assisted endoscopic papillosphincterotomy in the Rendezvous technique and choledocholithoextraction in patients with cholecystocholedocholithiasis improves the results of surgical treatment and is economically feasible, as it reduces the number of surgeries and hospital admissions for a patient.
Conflict of Interests
The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
ACKNOWLEDGEMENTS
The authors express their gratitude to the management of the multidisciplinary clinic of Samarkand State Medical University for the material provided for our study.
References
| [1] | Kurbaniyazov Z. B., Askarov P. A. Analysis of the results of surgical treatment of patients with injuries of the main bile ducts // Achievements in clinical and experimental medicine. – 2018. – №. 1. – p. 94-100. |
| [2] | Lupaltsov V. I. et al. Modern aspects of surgical tactics in the treatment of patients with cholelithiasis complicated by mechanical jaundice // Orenburg Medical Bulletin. – 2016. – Vol. 4. – №. 3 (15). – p. 51-53. |
| [3] | Sahu D., Mathew M.J., Reddy P.K. Outcome in Patients Undergoing Laparoscopic Cholecystectomy Following ERCP; Does Timing of Surgery Really Matter? J Minim Invasive Surg Sci., 2015, № 4, e25226. |
| [4] | Sotnichenko B. A., Makarov V. I., Savintseva N.V. Endovideosurgical treatment of patients with complicated forms of acute cholecystitis // Annals of Surgical Hepatology. – 2007. – Vol. 12. – №. 2. – p. 75-78. |
| [5] | Kurbaniyazov Z. B., Arziev I. A., Askarov P. A. Improvement of surgical tactics in the correction of biliary stasis after cholecystectomy using minimally invasive technologies // Bulletin of Science and Education. – 2020. – №. 13-3 (91). – p. 70-74. |
| [6] | Abramova A. G. Significance of minimally invasive methods in the treatment of complicated forms of cholelithiasis : diss. -Yaroslavl State Medical University of the Ministry of Health of Russia, 2017. |
| [7] | Mukhiddinov B.Kh., Kurbaniyazov Z.B., Askarov P.A. Modern approaches to surgical treatment of cholecystocholedocholithiasis. \\ Problems of biology and medicine. - 6 (150), 459-465. |
| [8] | Teremov S.A., Mukhin A.S. Experience of surgical treatment of patients with complicated forms of cholelithiasis. // Bulletin of experimental and clinical surgery. – 2013. – Vol. 6. – №. 3. – p. 399-404. |
| [9] | Khodzhimatov G. M. et al. Comparative evaluation of surgical methods of treatment of patients with acute calculous cholecystitis complicated by mechanical jaundice // Lymphology: from fundamental research to medical technologies. – 2016. – p. 250-252. |
| [10] | Repin V.N. et al. Two-stage endoscopic operations for complicated cholelithiasis // Medical almanac. – 2008. – №. 1. – p. 54-55. |
| [11] | Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos) / Yokoe M., Hata J., Takada T. [et al.] // J Hepatobiliary Pancreat Sci. - 2018. - Vol. 25 (1). - P. 41-54. - Doi: 10.1002/jhbp.515. |
| [12] | Sahoo M.R., Kumar A.T., Patnaik A. Randomised study on single stage laparo-endoscopic rendezvous (intra-operative ERCP) procedure versus two stage approach (pre-operative ERCP followed by laparoscopic cholecystectomy) for the management of cholelithiasis with choledocholithiasis. Journal of Minimal Access Surgery, 2014, № 10, рр. 139–143. https:// doi.org/ 10.4103/0972-9941.134877. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML