-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2205-2209
doi:10.5923/j.ajmms.20241409.16
Received: Aug. 20, 2024; Accepted: Sep. 10, 2024; Published: Sep. 10, 2024

Miracle Medical Treatment for Diabetic Foot Saving from Amputation
Faruk Erzengin1, Evren Bursuk2
1Department of Cardiology, Previous Dean, Istanbul Medical Faculty, University of Istanbul, Istanbul, Turkey
2Program of Biomedical Technologies, Vocational School of Technical Sciences, University of Istanbul Cerrahpasha, Istanbul, Turkey
Correspondence to: Faruk Erzengin, Department of Cardiology, Previous Dean, Istanbul Medical Faculty, University of Istanbul, Istanbul, Turkey.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

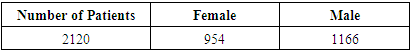
Throughout human history, Diabetes mellitus and its complications have affected a wide range of people. The most important of these complications is the Diabetic foot complication, which affects both disability, fatality and economically, and this study focuses on healing with only medical treatment without the need for amputation. Erzengin's solution for atheroma, consisting of 12 synthetic and 26 herbal ingredients, was applied to diabetic foot patients.When necessary, debridement was performed and Erzengin's solution for atheroma was administered to 2120 (954 female and 1166 male) diabetic foot patients and 100% success was achieved. This severe condition, which has been a major health problem of humanity until today and eventually led to amputation or death, was completely resolved with only medical treatment (Erzengin's solution for atheroma), and definitive recovery was achieved. This is a revolution in medicine.
Keywords: Erzengin solution for atheroma, Diabetic foot, Stopping amputation for diabetic foot
Cite this paper: Faruk Erzengin, Evren Bursuk, Miracle Medical Treatment for Diabetic Foot Saving from Amputation, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2205-2209. doi: 10.5923/j.ajmms.20241409.16.
1. Introduction
- Despite the steady progress in the treatment of atherosclerotic and atherothrombotic cardiovascular diseases, peripheral arterial disease (PAD), diabetic foot, coronary artery diseases, myocardial infarctions, cerebrovascular arterial disease, cerebrovascular occlusion and target organ infarts etc continue to be significant causes of morbidity and mortality, especially in industrialized countries. The term atherosclerosis refers to the thickened and hardened lesions, which have lipids and calcifications in the intimae and media of elastic and muscular arteries. To date, the primary cause of arterial atherosclerotic calcification has not yet been elucidated. It is generally accepted that atherosclerotic and calcified lesions first appear and develop within the innermost layer of the arteries (at the intimae). In 1995, the American Heart Association (AHA) described that the earliest lesions of atherosclerosis (fatty streaks or type III lesions) are present in the intimae of the aorta from childhood. Today, it is known that atherosclerosis begins as early as fetal life, especially in the fetuses of hypercholesterolemic mothers [1]. Formation and progression of atherosclerotic plaques and calcifications in all arterial beds of intimae have been well documented by many authors, such as V. Fuster and E. Falk [1,2,3,4], who subdivided the formation and progression of these plaques into several phases. During the progression of the atherosclerotic disease, the oxidative modified LDL (oxLDL), the inflammatory and immune response is accompanied by a fibro-proliferative response in which the vascular smooth muscle cells play dominant roles [1,2,3,4,5,6,7,8,9,10,11,12,13]. OxLDL has many proinflammatory properties, which explain the local up regulation of inducible endothelial cell adhesion molecules – even before lesion formation – in hypercholesterolemic atherosclerosis and plaque unstability leading to atherothrombotic events [1,2,3,4,5,6,7]. The extent to which atheroma masses or atheromatous components are produced depends on various factors such as genetics, diabetes, hypercholesterolemia, tobacco smoking, hypertension, abdominal obesity, gender, aging, high plasma uric acid level, chemical irritants, infections, high level sv CRP and fibrinogen, circulating vasoactive amines, and immune complexes, elevated heart rate etc.As mentioned in an international report on the social aspects of atherosclerosis [8], the risks factors for atherosclerotic vascular diseases that can be classified as major risk factors and emerging risk factors. Age, sex, high plasma uric acid levels, smoking, hypertension, low level HDL-cholesterol, elevated heart rate and diabetes are the major risk factors that accelerate the atheromatous process, while emerging risk factors include chemical irritants, infections, high sv CRP and fibrinogen levels, circulating vasoactive amines, and immune complexes that are associated with atherosclerotic complications. Thus, patients who have the emerging factors undergo invasive procedure that either involve stent implantation or arterial surgery [8].In this study, it is necessary to mention Diabetes mellitus, which is involved in the etiology of atherosclerosis, and diabetic foot, which is its complication. diabetes mellitus; It is defined as a syndrome in which there is insulin deficiency and/or insulin unresponsiveness with hyperglycemia, leading to impaired metabolism [14,15,16,17,18,19]. The American Diabetes Association considers diabetes mellitus in 4 main groups:1. Type I Diabetes mellitus (It is due to insulin deficiency.)2. Type II Diabetes mellitus (There is a decrease in insulin secretion with insulin resistance.)3. Other specific types of diabetes mellitus (MODY= Adult-Onset Diabetes of Youth,)4. Gestational Diabetes mellitus.Among these groups, Type I and II Diabetes mellitus are the most common types.Complications of diabetes mellitus; divided into acute and chronic. Acute complications of diabetes mellitus can be counted as hypoglycemia, diabetic ketoacidosis coma, hyperosmolar hyperglycemic nonketotic coma, Somogy and Dawn effects [14,15,16,17,18,19].Chronic complications of diabetes mellitus are due to its effect on the vessels. These chronic complications; It can be divided into microvascular (retinopathy, nephropathy, neuropathy, etc.) and macrovascular (coronary artery disease, stroke and peripheral artery diseases) and infection [14,15,16,17,18,19].All artheriopathies and neuropathies are most common complications of Diabetes mellitus. There are different types of diabetic neuropathy as hyperglycemic neuropathy, distal symmetrical polyneuropathy, autonomic neuropathy and mononeuropathy. Distal symmetrical polyneuropathy with sensory, motor and autonomic nerve involvement is one of the most common neuropathies. In this type, there is neuropathic pain and loss of sensation that causing foot ulcers and subsequent gangrene formation and lastly amputation. This type of neuropathy is in the form of gloves and socks, and both sensory and vibration, proprioception and temperature losses are observed. Diabetic ulcers are mostly in the lower extremities and most of them go to ischemia induced gangrene and then amputation [14,15,16,17,18,19,20,21,22,23,24,25].The morbidity and mortality rates of macrovascular complications of diabetes mellitus are very high. As mentioned above, it is the combination of insulin resistance, hyperglycemia, hypertriglyceridemia, low HDL, high LDL lipoprotein oxidation, inflammation and endothelial damage that contribute to the formation of atherosclerosis in Diabetes mellitus. These complications cause myocardial infarctions, strokes and peripheral arterial disease (PAD) [14,15,16,17,18,19,20,21,22,23,24,25].PAD, neuropathy, gangrene and amputation are especially seen in those with Type 2 Diabetes mellitus, and PAD has already started in most cases at the time of diagnosis. Those that affect the development of PAD; age, time elapsed after diagnosis of Diabetes mellitus, poor glycemic control, obesity, Metabolic syndrome, genetics, stress, physical inactivity…etc. Due to the easier occlusion of small arteries and arterioles, gangrene occurs especially in the foot and toe areas of the lower extremities and leads to amputation. The results of the surgical treatment (debridement, bypass, etc.) of the diabetic foot are not very encouraging. Mortality rates after amputation are significantly higher. The 5-year mortality rates after major amputation are roughly between 39% and 80%. Mortality is particularly associated with age, gender, HbA1c, infection, and renal failure. When planning before amputation surgery, it should be operated at the appropriate level, taking into account that the prosthesis will be attached. Getting used to these prostheses; It is determined by factors such as age, other diseases, psychological acceptance, dialysis, and both physical and psychological rehabilitation is required after the prosthesis is placed. Moreover, the economic burden of the prosthesis is also rather high. Complications that may be faced by people with prosthesis implanted after diabetic amputation include early and late postoperative complications, prosthesis compatibility problem, deep vein thrombosis, ulcer, infection, and prosthesis wearing out [14,15,16,17,18,19,20,21,22,23,24,25].Objective: The aim of this study is to cure the helpless disease which is atherosclerosis obliterans such as peripherial arterial atherosclerotic disease, and Diabetic foot.
2. Materials -Methods
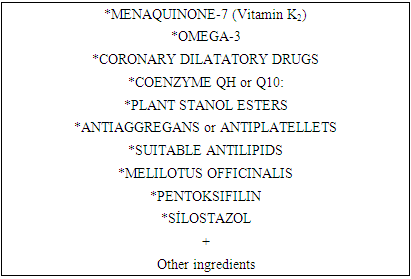
- Until this time, as mentioned above, the results of both invasive (stent, bypass, amputation) and non-invasive (treatments) of the diabetic foot have been extremely unsuccessful and depressing. As it is known, the current treatment of atherosclerosis obliterans is of two types. The first is the botanical origin treatments preferred in the Far East, and the other is the synthetic origin treatments used in Continental Europe. Recently, another treatment is the mix (botanical plus synthetic drugs) treatment method preferred by us and the USA. We decided to treat the diabetic foot patient’s with our medical solution. Our solution is composed of 12 synthetic and 26 herbal ingredients and named as Erzengin's solution for atheroma (Table 1).
|
|
3. Results
- The number of all cases treated since 07.07.1997 is more than 30000 and 2120 (954 female and 1166 male) of these cases were diabetic foot patients and treated with this treatment (Table 2). This solution was administered orally to patients once a day. Doppler arteriography (duplex system), lower extremity MR and CT angiography examinations were performed before the treatment of these diabetic foot patients and these examinations were repeated after the treatment. These repeated examinations proved that our treatment was 100% successful. As an example, before and after photos of 2 diabetic foot patients who recovered with this treatment are shown. Accordingly, the figures for the first diabetic foot patient before and after treatments are as follows (Figure 1a-b and Figure 2a-b).
 | Figure 1 a-b. Diabetic foot before treatment for the first patient |
 | Figure 2 a-b. Diabetic foot after treatment for the first patient |
 | Figure 3. Diabetic foot before treatment for the second patient |
 | Figure 4 a-b. Diabetic foot after treatment for the second patient |
4. Conclusions
- Throughout history, humanity has faced the problem of diabetic foot, having no solution and causing disability or death. In this study; we have shown that the diabetic foot can be saved from amputation by applying only debridement when necessary, and medical treatment. This work; It will not only save human health, but also prevent economic losses by increasing the quality of life. In terms of what is known about diabetic foot, this study is a revolution in medicine.
ACKNOWLEDGEMENTS
- This study did not receive support from any person or organization. The author(s) declared no potential conflicts of interest with respect to the research, autorship, and/or publication of this article.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML