-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2177-2182
doi:10.5923/j.ajmms.20241409.11
Received: Aug. 2, 2024; Accepted: Sep. 1, 2024; Published: Sep. 10, 2024

Immunobiochemical Features of Pulmonary Hypertension in Patients with Diseases of the Bronchopulmonary System
Tasheva Feruza Olimdjonovna1, Khamdamov Bakhtiyor Zarifovich1, Fayzullaeva Nigora Yahyayevna2, Raufov Alisher Anvarovich2
1Bukhara State Medical Institute, Bukhara, Uzbekistan
2Institute of Human Immunology and Genomics, Uzbekistan
Correspondence to: Khamdamov Bakhtiyor Zarifovich, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance: The study focuses on cytokines and biochemical markers in pulmonary hypertension (PH) in patients with bronchial asthma (BA), chronic obstructive pulmonary disease (COPD), and their combination. Objective: To identify the immune and biochemical features of PH in these patients. Methods: A total of 95 patients with PH were examined, including 17 with BA, 35 with COPD, and 43 with ACOPD. Levels of IL-4, IL-17A, IL-18, TNFα, IFNγ, CRP, fibrinogen, NT-proBNP, and ET-1 were studied. Results: Statistically significant differences in the levels of these markers were found between the groups. Conclusions: Cytokines play a key role in the pathogenesis of PH and can serve as markers of disease severity. This can help in developing new treatment and diagnostic methods. The results can be used to improve clinical management of patients with PH.
Keywords: Pulmonary hypertension, Bronchial asthma, Chronic obstructive pulmonary disease, Cytokines, Biochemical markers
Cite this paper: Tasheva Feruza Olimdjonovna, Khamdamov Bakhtiyor Zarifovich, Fayzullaeva Nigora Yahyayevna, Raufov Alisher Anvarovich, Immunobiochemical Features of Pulmonary Hypertension in Patients with Diseases of the Bronchopulmonary System, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2177-2182. doi: 10.5923/j.ajmms.20241409.11.
Article Outline
1. Relevance
- A fundamentally important question in modern practical medicine is the connection between the formation of a layer of chronic diseases, such as BA/COPD and hypertension/CHD, with processes occurring in the cardiorespiratory system or with shifts in the immune system [3,6,7,10,11,12,24,25,26]. According to many authors, the cause of the overlap or layering of bronchial asthma and chronic obstructive pulmonary disease and the development of vascular complications are various immune disorders that cause a decrease in the body’s resistance to microbial infection [1,4,8,13,14,15,16,22].A detailed study of cytokines helps to determine their significant and diverse role in the development of immune, allergic and inflammatory reactions in diseases of the cardiorespiratory system. The understanding of the pathogenesis of pulmonary and cardiovascular diseases is complemented by increasingly new data on the nature and functions of these mediators. As the role of cytokines becomes clearer, it becomes possible to control the inflammatory process and other pathophysiological consequences of lung injury [2,5,9,17,18,19,20,21,23].
2. Purpose of the Study
- To study the features of cytokine status and biochemical markers in pulmonary hypertension in patients with bronchial asthma, COPD and the intersection of BA and COPD.
3. Materials and Research Methods
- We selected 95 patients with pulmonary hypertension (PH) to study the state of the immune system. Of these, 17 patients with asthma, 35 patients with COPD and 43 patients with ACO. 20 practically healthy people made up the control group. Clinical material was collected at the Bukhara Regional Multidisciplinary Medical Center and at the Bukhara branch of the Republican Scientific and Practical Center for Emergency Medical Care.To determine the concentrationIL-4, IL-17A, IL-18, TNFα, IFNγ, CRP, fibrinogen, NT-proBNP, EN1 in the blood serum of the study groups was used using the three-stage “sandwich” method - this is a type of three-phase ELISA.Statistical processing of the research results was carried out using the SPSS v16.0, R, PLINK and Haploview 4.2 software packages.
4. Results of the Study and Their Discussion
- In our studies, we conducted a comparative analysis of pro- and anti-inflammatory cytokines in the studied groups (IL-4, IL-17A, IL-18, TNFα, IFNγ) (Fig. 1).
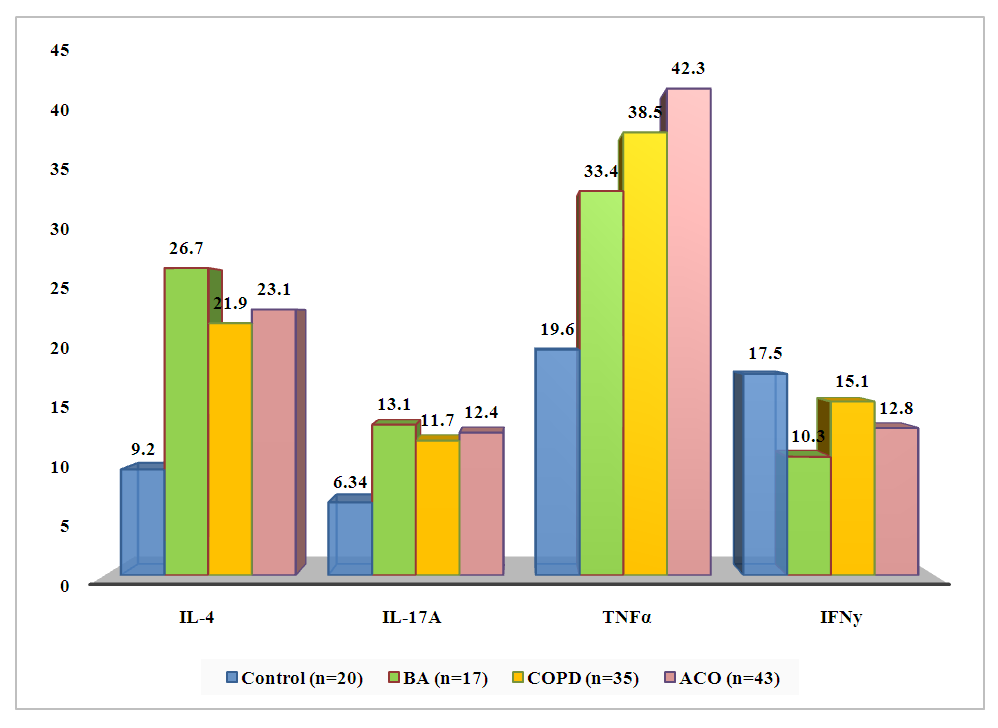 | Figure 1. Comparative analysis of pro- and pro-inflammatory cytokines in the group with asthma, COPD and ACO in combination with PH |
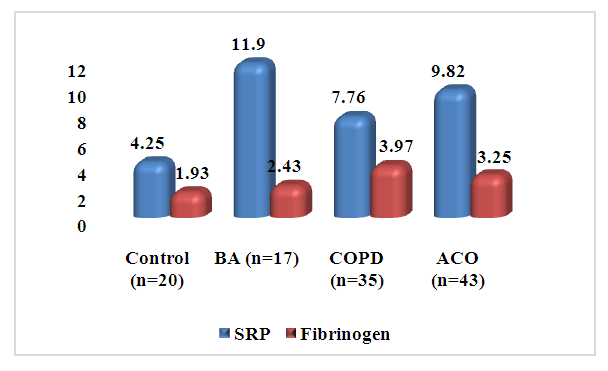 | Figure 2. Levels of CRP and fibrinogen in those examined (mg/l, g/l) |
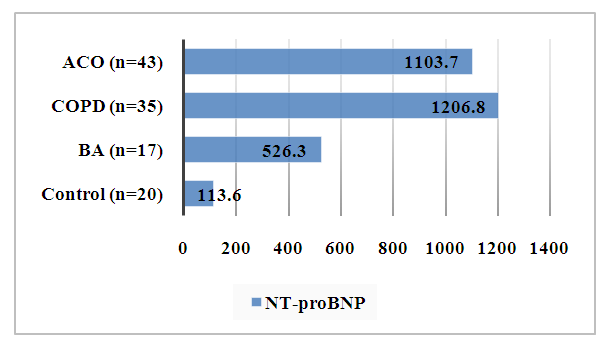 | Figure 3. NT-proBNP level in those examined (pg/ml) |
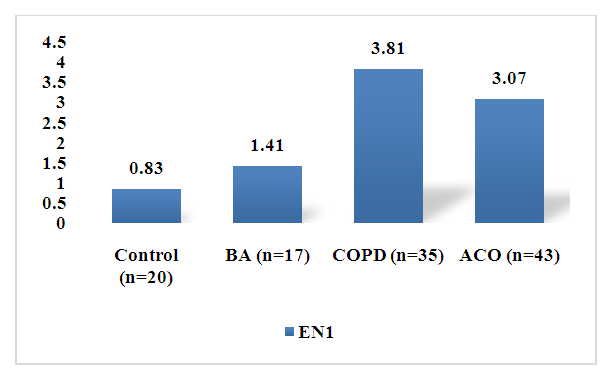 | Figure 4. Endothelin-1 level a mong those examined (pg/ml) |
5. Conclusions
- The study showed that patients with PH associated with asthma, COPD and ACO experienced significant changes in the levels of CRP, fibrinogen, NT-proBNP and EN1 compared with the control group. These markers can be used to assess disease severity and prognosis in patients with PH. Higher levels of these markers in patients with COPD and ACO compared with patients with asthma indicate greater inflammation and vascular damage in these patient groups. This highlights the need for early diagnosis and adequate treatment to prevent the progression of PH and its associated complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML