-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2171-2176
doi:10.5923/j.ajmms.20241409.10
Received: Jul. 30, 2024; Accepted: Aug. 20, 2024; Published: Sep. 10, 2024

Features of the Clinical Course of the Osteo-Articular Form of Tuberculosis
Khamdamov Bakhtiyor Zarifovich, Bozorov Shuhrat Istamovich
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Khamdamov Bakhtiyor Zarifovich, Bukhara State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

According to WHO data, which controls the fight against tuberculosis worldwide, there are 20-30 million patients with active tuberculosis on Earth. Every year, about 9 million people get sick again, and more than 3 million people die. Osteoarticular tuberculosis accounts for 3-5% of all tuberculosis patients. This disease develops slowly and is often associated with irreversible destruction and deformation of bones and joints. The study aims to investigate the clinical and functional features of the osteoarticular form of tuberculosis.
Keywords: Osteoarticular tuberculosis, Clinic, Laboratory tests
Cite this paper: Khamdamov Bakhtiyor Zarifovich, Bozorov Shuhrat Istamovich, Features of the Clinical Course of the Osteo-Articular Form of Tuberculosis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2171-2176. doi: 10.5923/j.ajmms.20241409.10.
Article Outline
1. Relevance
- According to WHO, which controls the fight against tuberculosis in the world, there are currently 20-30 million patients with active tuberculosis of all localizations on Earth. Every year, up to 9 million people get sick again, and more than 3 million people die. There is no visible trend towards stabilization or improvement of these indicators in the world [1,5,7,14]. Osteoarticular tuberculosis accounts for up to 3-5% of all patients suffering from tuberculosis, which amounts to 270-450 thousand people suffering from osteoarticular tuberculosis per year. Of the tuberculosis patients on the planet, from 300 to 900 thousand people have specific osteoarticular lesions [2,4,9,16].The level of diagnosis of CST using modern methods is extremely low, which is associated not only with the complexity of identifying the pathology, but also with the difficulty of its bacteriological and histological verification, which does not exceed 60% [3,6,8,13]. A feature of CST is the high degree of disability of patients (up to 70%), even despite the possibility of its complete cure with modern surgical and conservative methods [8,10,13,18]. The complexity of the situation is explained by the fact that the disease develops slowly, flows with periods of relative well-being, and the need to confirm tuberculosis is thought about only when irreversible destruction and deformation of bones and joints develops or complications develop, which often confine people to bed [11,15,20].For practical healthcare, it remains relevant to determine the immunological and molecular genetic aspects, study the processes of development of antibiotic resistance to Mycobacterium tuberculosis, optimize the diagnosis, treatment and prevention of the osteoarticular form of tuberculosis.
2. Purpose of the Study
- Study of clinical and functional features of the osteoarticular form of tuberculosis.
3. Materials and Research Methods
- To solve this problem, a comprehensive examination was carried out on 223 patients aged 18-87 years with osteoarticular forms of tuberculosis, who were examined and treated in the period 2022 - 2024 at the Bukhara Regional Center for Phthisiology and Pulmonology. The diagnosis was made based on clinical and functional data in accordance with the international consensus on the diagnosis and treatment of bronchopulmonary diseases. Diagnoses were verified based on a thorough history, clinical, laboratory (general blood count, urine), biochemical blood test, bacteriological examination of sputum, instrumental (chest x-ray, electrocardiography, spirography, picfluometry). Particular attention was paid to the duration of the pathological process, previous and concomitant diseases.
4. Research Results
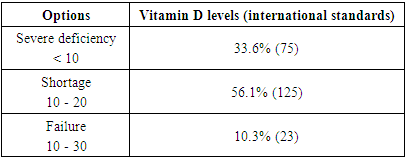
- When analyzing the data obtained by age of patients with CST, we obtained the following results: patients from 18 to 30 years old accounted for 5.39% (n=12), from 30 to 59 years old – 53.8% (n=120), from 60 years and older were 40.8% (n=91). (Fig. 1.)
 | Figure 1. Age distribution of patients with CST (%), (P<0.05) |
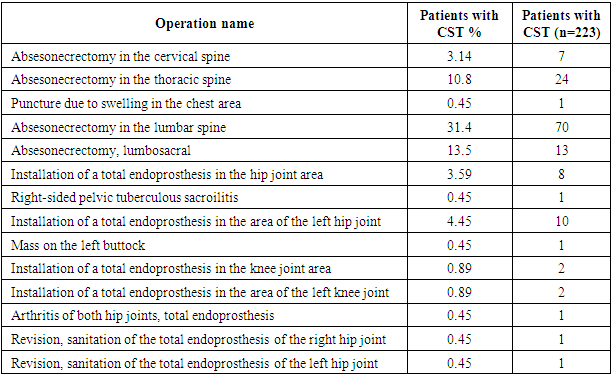
 | Figure 2. Distribution of groups by gender of patients with CST (%), (P<0.05) |
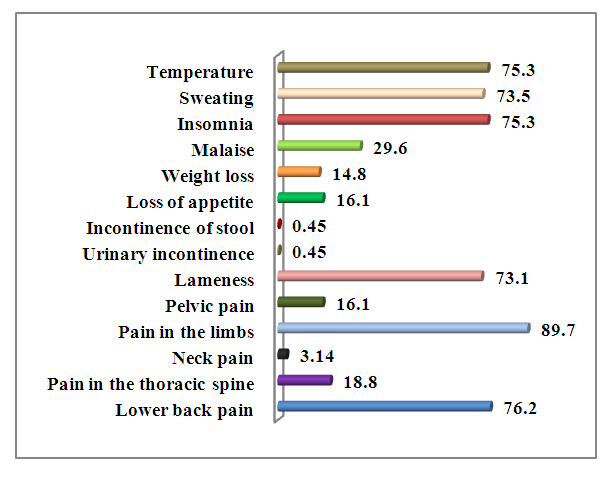 | Figure 3. Main complaints of the examined patients (%), (P<0.05) |
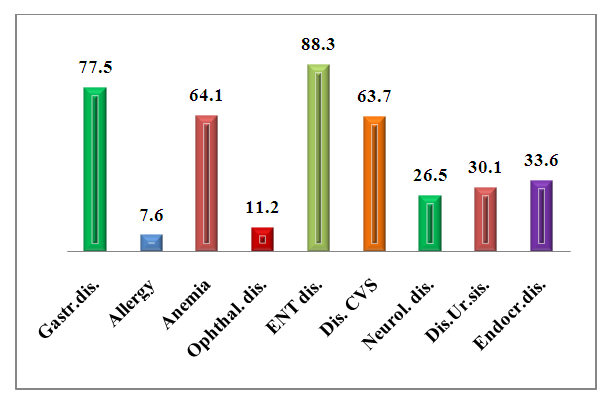 | Figure 4. Concomitant pathology inpatients with CST (%), (P<0.05) |
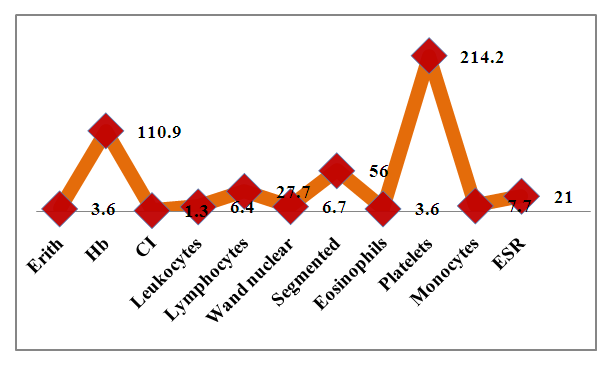 | Figure 5. Parameters of general blood test in patients with CST, (P<0.05) |
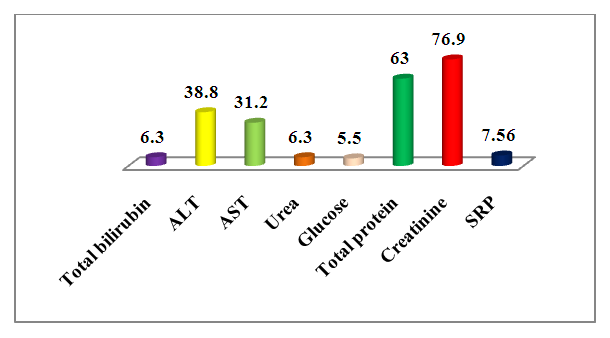 | Figure 6. Biochemical blood test parametersin the examined patients, (P<0.05) |
|
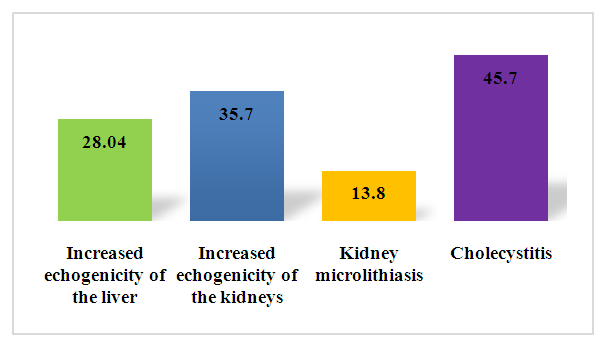 | Figure 7. Ultrasound diagnostics of organs abdominal cavity, (%), P≥0.05 |
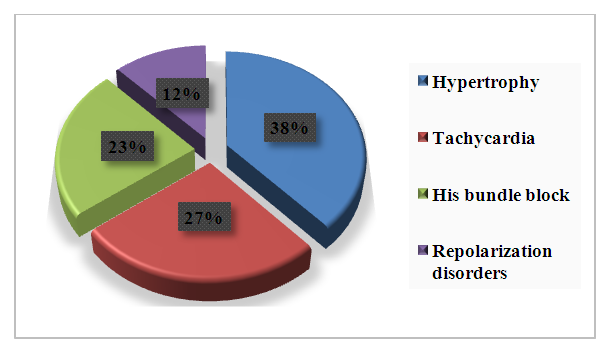 | Figure 8. ECG changes in patients with CST, (%), P≥0.05 |
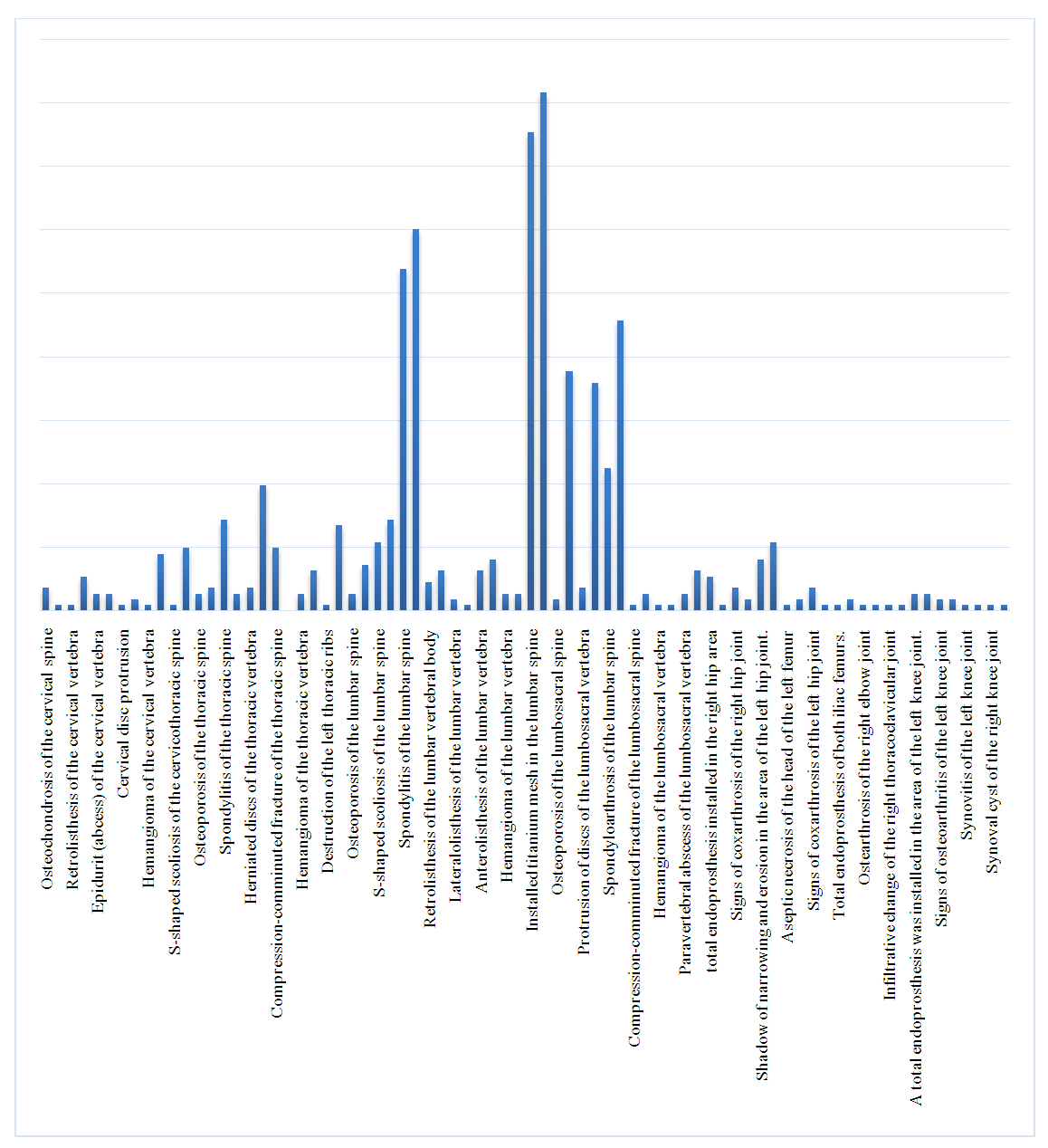
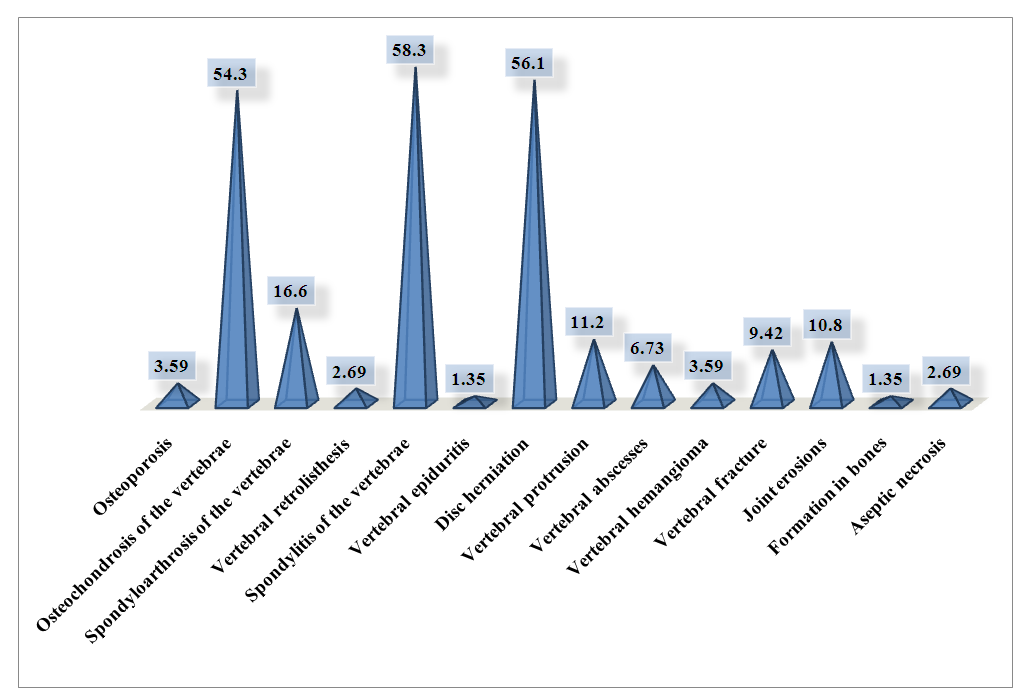 | Figure 9. X-ray signs examined with CST, (%) |
|
 | Figure 10. Histology of tissue after surgery in patients with CST, % |
5. Conclusions
- Thus, our studies allowed us to draw the following conclusions: patients with CST were characterized by the prevalence of such complaints as pain in the joints of the arms and legs and restrictions on their movement; Frequent diseases of the ENT organ and cardiovascular system and minor damage to the organs of vision and the genitourinary system; The analysis of laboratory data was characterized by moderate leukocytosis and increased ESR, as well as CRP; Instrumental studies revealed slight damage to the parenchymal organs, disturbances in the rhythm and conductivity of the heart and moderate osteoporosis with the phenomena of narrowing of the interarticular spaces and focal changes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML