-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2163-2165
doi:10.5923/j.ajmms.20241409.08
Received: Aug. 20, 2024; Accepted: Sep. 3, 2024; Published: Sep. 6, 2024

Differential Diagnosis of Acute Leukemia in Children
Iriskulov B. U., Tadjibaeva R. B., Abdukhalikova N. F., Otazhanova A. N., Jakhsimuratova Kh. T.
Tashkent Medical Academy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents studies on the peculiarities of the course of acute leukemia in children and differential diagnosis of ALL and ALL in the Republic of Uzbekistan. The studies were conducted among children with acute leukemia in the Oncohematology Department of the Center of Children's Hematology, Oncology and Clinical Immunology.
Keywords: OML, OLL, Blast cells, Leukemic infiltration, Myeloperoxidase, Nonspecific esterase, SHIK-positive substance
Cite this paper: Iriskulov B. U., Tadjibaeva R. B., Abdukhalikova N. F., Otazhanova A. N., Jakhsimuratova Kh. T., Differential Diagnosis of Acute Leukemia in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2163-2165. doi: 10.5923/j.ajmms.20241409.08.
1. Introduction
- Acute leukemia is a malignant tumor disease of the blood system primarily affecting the bone marrow. The tumor substrate is represented by immature blast cells displacing normal elements in the bone marrow and infiltrating various organs and tissues. Acute leukemia is a clonal disease arising from a single mutated hematopoietic cell, which refers to progenitor cells. Among malignant neoplasms of hematopoietic and lymphoid tissue, which make up half of all malignant tumors in children, leukemia accounts for up to 40%. Increase in the incidence of OL is observed at the age of 2 to 5 years with a gradual decrease in the number of patients to 7 years. Boys are more frequently affected than girls [1].Despite numerous studies, the etiology of this disease has not been accurately established to this day. According to the clonal theory, the growth of a leukemic population occurs from a single cell and the rate of growth depends on the proportion of actively proliferating cells, their generation time, the number of cells with a limited lifespan, and the rate of cell loss. When the leukemic population reaches a certain mass, inhibition of differentiation occurs and proliferative activity prevails over normal hematopoiesis [3].Numerous studies in this area have revealed that various risk factors can trigger the onset of this disease. The most common of which are: 1. Genetic factors. They are related to changes in DNA. DNA is responsible for implementing and storing the genetic program. Mutations in DNA can lead to the development of the disease. Genetic syndromes. Some genetic syndromes increase the risk of leukemia in children. 2. Congenital disorders of the immune system. These include ataxia-telangiectasia, Wiskott-Aldrich syndrome, Schwachman-Daimond syndrome, and Bloom syndrome. 3. Cases of leukemia in close relatives. Having a sibling with leukemia slightly increases the likelihood of developing leukemia. 4. Lifestyle factors. Smoking, obesity, drinking a lot of alcohol, and lots of sun exposure are important risk factors for cancer in adults but do not play a role in most childhood tumors. 5. Environmental factors. The most common of these, radiation and certain chemicals can increase a child's risk of developing leukemia (as well as other tumors). 6. Children who have had an organ transplant have an increased risk of developing certain cancers, including ALL. Other factors: exposure to electromagnetic fields, living near nuclear power plants, infections in early childhood, age of the mother at the time of birth, etc. [2].
2. Purpose of the Study
- Studying the peculiarities of the course of acute leukemia in children. To carry out differential diagnostics of OLL and OML.
3. Materials and Methods
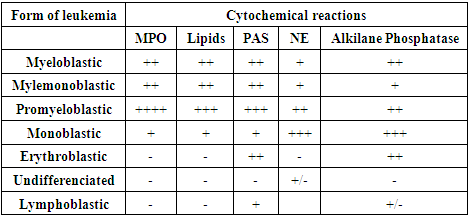
- The study was conducted among 30 children with acute leukemia in the Oncohematology Department of the Center for Pediatric Hematology, Oncology and Clinical Immunology.The study was based on statistical data from the official websites of World Cancer Research Fund International, Global Cancer Observatory and World Health Organization.In the differential diagnosis of OLL and OML, investigations can be characterized by the following results: Physical examination. When examining the physical condition of patients, clinical manifestations are characterized by pallor of the skin, rapid fatigability, dyspnea. A characteristic manifestation of hemorrhagic syndrome was polymorphous hemorrhages (petechiae, ecchymoses, hematomas) on the skin and mucous membranes, painless enlargements of peripheral lymph nodes are noted. Fever may be due to the leukemia itself or to the course of a bacterial, viral, or fungal infection. Hyperplastic syndrome includes enlargement of peripheral lymph nodes as palpable dense, painless conglomerates. Infiltration of the liver and spleen results in hepatosplenomegaly and may present with abdominal pain, increased abdominal volume, nausea, and anorexia. Leukemic infiltration of the periosteum and joint capsule, bone infarcts, and tumor-induced increase in bone marrow volume lead to the development of bone pain [4].Radiologic studies reveal characteristic changes, especially in the tubular bones, near large joints. Pathologic fractures of the tubular bones or spine may be the first manifestation of the disease. Arthralgia and joint swelling may be mistaken for symptoms of rheumatoid arthritis or other diseases, and bone lesions may be mistaken for osteomyelitis [4].Laboratory examination of peripheral blood. Changes in the peripheral blood count in acute leukemia depend on the tumor mass. There may be suppression of all sprouts of hematopoiesis, as well as each separately or in combination.The leukocyte count on initial examination may vary, but is often normal or slightly decreased. Leukocytosis is observed in 25-30% of cases. Blast cells may be absent, determined in small numbers or make up a significant part of the cellular composition (up to 95-98%). The study of red blood demonstrates anemia, which is normochromic in nature. The sharpest decrease in the number of erythrocytes, hemoglobin indices is detected in erythromyelosis. The number of platelets is different: normal, increased or decreased. For example, in the promyelocytic variant of acute leukemia, the lowest platelet counts are observed.Cytogenetic and molecular genetic studies of bone marrow cells. Molecular biology techniques are aimed at targeting specific, often minimal DNA or m-RNA alterations in tumor cells. Clonal chromosomal abnormalities occur in 90% of pediatric ALL cases. Approximately half of the detectable changes are reciprocal translocations accompanied by the formation of chimeric genes and synthesis of abnormal proteins. Clonal abnormalities occur in 80-85% of pediatric ALL patients.Cytochemical study of bone marrow cells. An important stage is the determination of the variant of acute leukemia, necessary for the selection of an adequate program of special treatment. The object of cytochemical study is blast cells of bone marrow, peripheral blood and cerebrospinal fluid. A panel of cytochemical reactions is carried out, including the study of myeloperoxidase activity, nonspecific esterase, the presence of SHIK-positive substance (PAS-reaction), determination of lipids in blast cells [2]. Alkaline phosphatase (ALP) activity in neutrophilic leukocytes is also studied in the process of CML diagnosis.MyeloperoxidaseIt is an enzyme localized in specific azurophilic granularity in the cytoplasm of granulocytic sprout cells, and is therefore a specific marker of myeloid cells. Reaction principle: peroxidase, being an enzyme - lysosomal catalase, catalyzes oxidation of benzidine, intensely colored compounds are formed. Evaluation of the reaction: in acute myeloblastic leukemia (AML), the enzyme activity is positive, ranging from slight and moderate to pronounced; in acute lymphoblastic leukemia (ALL), it is negative [2].Nonspecific esteraseEsterases are enzymes (hydrolases) that cleave simple esters of N-free alcohols and organic acids and are localized in lysosomes. Reaction principle: alpha-naphthylacetate esterase accelerates the hydrolytic cleavage of alpha-naphthylacetate esterase to acetic acid and alpha-naphthol, which, combining with diazonium salt, forms a brown-black staining, insoluble in water. Evaluation of the reaction: enzyme activity is manifested by black-brown staining of the cytoplasm. The reaction is used for the purpose of differential diagnosis of OML, since the enzyme activity is usually negative in lymphoblasts [2].PAS (PAS)-reaction according to the McManus methodGlycogen, being a mucopolysaccharide, is determined in all cells of the granulocytic sprout. The character of distribution is different: in myeloid and monocytoid cells the PAS-positive substance is diffusely located in the cytoplasm of cells, in lymphocytic cells - in the form of granules. Reaction principle: the mechanism of SHIC reaction is based on oxidation of glycol groups or their amino- or alkylamino derivatives to aldehydes by iodic acid, which, when interacting with Schiff's reagent, form a red-colored product. Evaluation of the reaction: Schiff-positive substance of red color is located in the cytoplasm of cells diffusely, in the form of granules, clumps. Myeloblasts are characterized by diffuse reaction. In lymphoblasts - in the form of granules of various sizes, up to clumps on a colorless background. In monoblasts the reaction is negative or finely dispersed on a diffuse background [2].LipidsLocalized in the cytoplasm of cells. Positive reaction is detected in the form of granules in cells of the granulocytic sprout, starting with myeloblast. Single granules may be observed in monocytoid cells. Reaction principle: phospholipids are detected when lipophilic dyes that dissolve in intracellular lipids are used. Evaluation of the reaction: sudanophilic granules are detected in cells of granulocytic sprout in the form of black granules in blast cells of granulocytic genesis. In lymphoblasts, cytochemical reaction to lipids is usually negative [2].For detailed visualization we present the following table:
4. Conclusions
- According to the results of the study it was found that the cases of diagnosis of acute lymphoblastic leukemia and acute myeloblastic leukemia in 30 children under the supervision of a hematologist of the Center for Pediatric Hematology, Oncology and Clinical Immunology revealed no significant differences in the clinical picture, results of instrumental studies in these diseases. The results of laboratory tests play a major role in differential diagnostics of OLL and OLM, namely:1. In cytochemical study of OLL blast cells the reaction to myeloperoxidase and lipoproteins is negative in 100% of cases, in OML - positive;2. Cytogenetic and molecular genetic studies of bone marrow cells revealed the presence of various chromosome abnormalities characteristic of OLL and OML.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML