-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(9): 2159-2162
doi:10.5923/j.ajmms.20241409.07
Received: Aug. 21, 2024; Accepted: Sep. 2, 2024; Published: Sep. 6, 2024

Videothoracoscopy for Surgical Treatment of Tumors and Mediastinal Cysts
N. N. Nazarov1, Madazimov M. M.2, A. L. Makhmudov3, A. A. Turgunboev4, I. Kh-A. N. Nazirjonov3
1Andijan State Medical Institute, Assistant of the Department of 1st Faculty and Hospital Surgery, Andijan, Republic of Uzbekistan
2Department of General Surgery, Doctor of Medical Sciences, Professor, Andijan State Medical Institute
3Clinic "Fanomed" Thoracic Surgeon, Andijan, Republic of Uzbekistan
4Andijan State Medical Institute, Assistant of the Department of Surgical Diseases, Andijan, Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

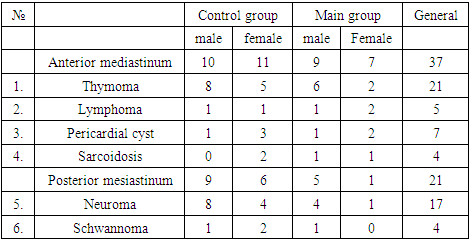
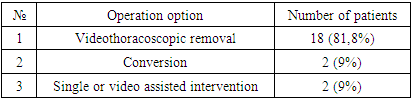
The treatment of 58 patients with tumors and cysts of the mediastinum aged from 17 to 67 years is presented. The patients were divided into two groups: control group - 36 and main group - 22. Localization was in the anterior mediastinum in 37 patients, in the posterior mediastinum in 21 patients. Video-assisted thoracoscopic interventions were performed in 22 patients, conversion in 2 patients, single-port or video-assisted thoracoscopy in 2 patients. Results: There were no complications observed in patients undergoing video-assisted thoracoscopic surgery. The data obtained indicate the high safety and effectiveness of video-assisted thoracoscopic operations in patients with mediastinal tumors due to the low incidence of intra- and postoperative complications. Videothoracoscopic interventions make it possible to remove large tumors in the absence of ingrowth or ingrowth of mediastinal structures.
Keywords: Videothoracoscopy VTS, Single-port thoracoscopy, Video-assisted thoracoscopy VATS, Robotic videothoracoscopy RVTS
Cite this paper: N. N. Nazarov, Madazimov M. M., A. L. Makhmudov, A. A. Turgunboev, I. Kh-A. N. Nazirjonov, Videothoracoscopy for Surgical Treatment of Tumors and Mediastinal Cysts, American Journal of Medicine and Medical Sciences, Vol. 14 No. 9, 2024, pp. 2159-2162. doi: 10.5923/j.ajmms.20241409.07.
Article Outline
1. Introduction
- The roots of thoracoscopy go back to 1910, when the Swedish physician Han Christian Jacobeus first looked into the pleural cavity through the small opening of a modified cystoscope [1,3] to perform pleural adhesiolysis for tuberculosis. Thus, a new way of diagnosing and treating chest diseases was opened. The method was reborn with the advent of new instruments in the early 1990s, and a new approach called video-assisted thoracic surgery (VATS) [2,5].Over the next two decades, up to this point, a revolution in thoracoscope design unfolded before our eyes. These innovations are the fruits of the joint efforts of surgeons and engineers. With unprecedented visual clarity [1,7], comparable surgical productivity [1,8], equivalent or improved postoperative outcomes [4,9], and subsequent cost reductions, thoracopic surgery in its various forms is beginning to attract more surgeons to this area. VTS has proven to be an excellent surgical approach in many centers. As a result, this approach is gradually replacing open thoracotomy as the standard of care for the diagnosis and treatment of a number of chest diseases.However, the field faces two major challenges, namely limited agility and poor control intuition. We analyzed the strengths and weaknesses of VTS in parallel with traditional thoracotomy in the treatment of mediastinal tumors and cysts.Mediastinal tumors are a group of benign and malignant tumors of various structures, located within the anatomical limits of the mediastinum and of non-organ origin. The frequency of mediastinal tumors in the structure of oncological diseases is about 1%. Malignant and benign are found and diagnosed in a ratio of 4: 1. Mediastinal tumors are detected mainly in young and middle age; men and women are affected equally often. Open diagnostic operations (mediastinotomy, diagnostic thoraco- and sternotomy) are performed less and less often due to their traumatic nature, and the role of videothoracoscopy as a universal diagnostic alternative is still not fully defined.Complete surgical resection of mediastinal tumors requires excellent knowledge and management. Large tumors in proximity to vital structures require a high level of training and sufficient knowledge to assess the risks and benefits during certain surgical procedures. Currently, anterior and posterior mediastinal tumors are recognized as ideal candidates for minimally invasive resection.However, there is no consensus among surgeons regarding the best minimally invasive technique between VTS, VATS, and RATS. VTS provides better impact due to high definition, three-dimensional images and the possibility of using a fourth thoracoport. These intraoperative benefits include minimally invasive techniques using VTS to reduce mortality and morbidity, improve quality of life, and shorten length of hospitalization [5,6].
2. Materials and Methods of Research
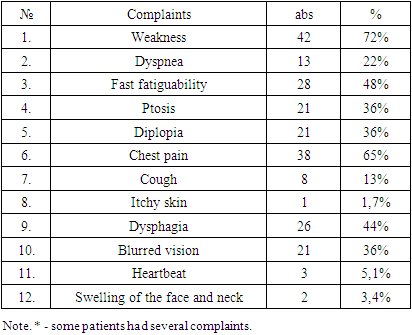
- From 2020 to 2023, 58 patients with mediastinal diseases, aged from 17 to 67 years, were under our supervision at the Fanomed clinic. The patients were divided into two groups: the main group and the control group. Upon admission, patient 7 had no complaints. The remaining patients had the complaints presented in Table 1.
|
|
3. Results of the Study
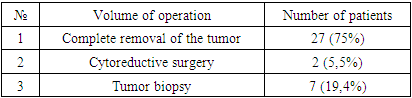
- In patients in the control group with thymic formations, longitudinal sternotomy and extended thymectomy were performed in 10 cases. In one case, due to tumor growth into the pericardium and the right atrium, it was possible to partially remove the thymus gland, leaving part of the tumor. In the postoperative period, one patient developed suppuration of the postoperative wound, mediastinitis, which was eliminated by conservative methods.Mortality occurred in one patient in the postoperative period on day 3; the cause of death was massive pulmonary embolism. In other cases, a lateral thoracotomy of 5 m/r was performed. Pericardial cysts in all 4 cases were located on the right side and were completely removed. In 4 cases in patients with sarcoidosis and lymphoma, the operation ended with tumor resection and biopsy.In patients in the control group with neoplasms of the posterior mediastinum, lateral thoracotomy and tumor removal were performed. Table 3.
|
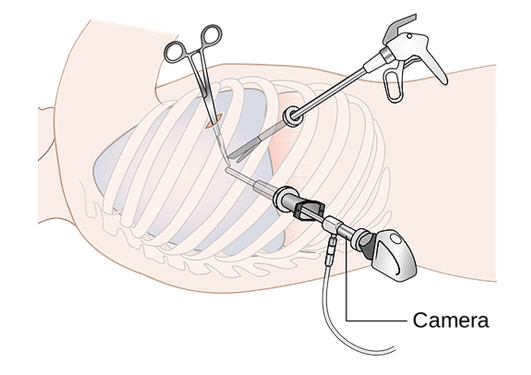 | Figure 1. Diagram of the location of thoracoports |
|
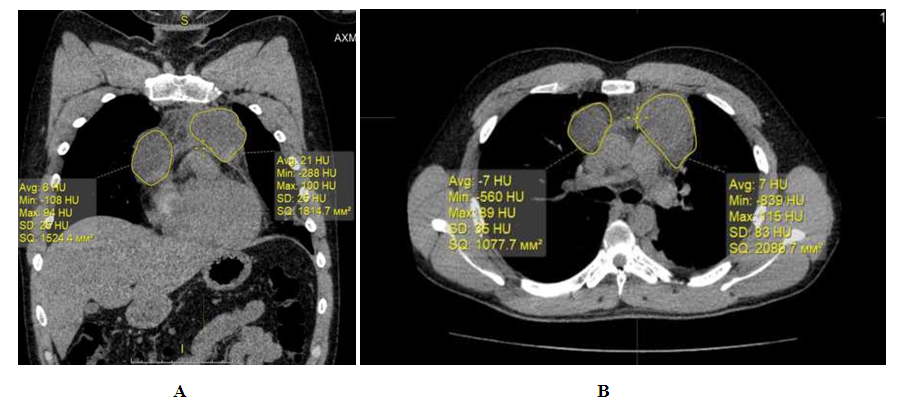 | Figure 2. MSCT image (A,B) of a complete pericardial cyst on the right, a protrudicular cyst on the left |
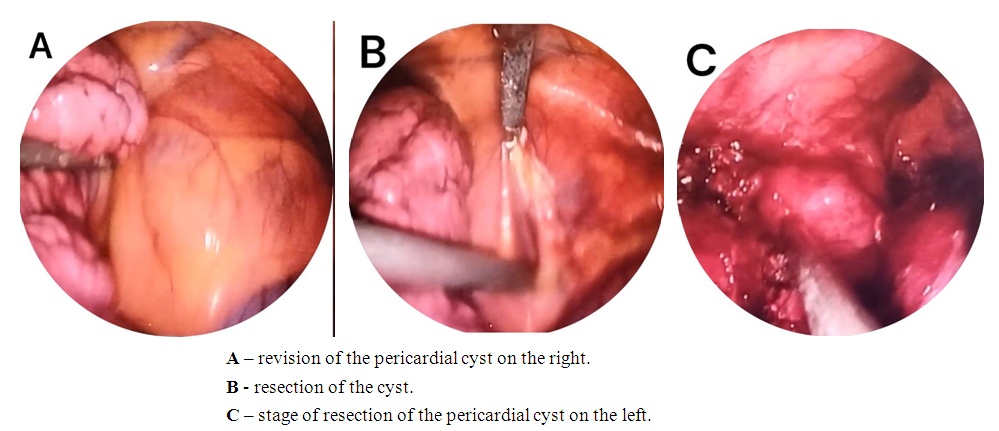 | Figure 3. Stages of video-assisted thoracoscopic surgery in this patient |
4. Conclusions
- Videothoracoscopy is an effective and safe method in patients with mediastinal masses, which indicates a low incidence of intra and postoperative complications. In this case, the choice of access (videothoracoscopy, one port or video-assisted intervention) should be determined strictly by the localization, size of the formation, and its relationship with surrounding vital organs.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML