-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(8): 2127-2132
doi:10.5923/j.ajmms.20241408.37
Received: Aug. 9, 2024; Accepted: Aug. 28, 2024; Published: Aug. 30, 2024

The Role of Hormonal Imbalance in the Development of Abnormal Uterine Bleeding in Women Associated with Ovulatory Dysfunction
Abraeva N. N.1, Shukurov F. I.2
1Assistant of the Department of Obstetrics and Gynecology Termez Branch, Tashkent Medical Academy, Tashkent, Uzbekistan
2Doctor of Medical Sciences, Head of the Department of Obstetrics and Gynecology, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Shukurov F. I., Doctor of Medical Sciences, Head of the Department of Obstetrics and Gynecology, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim: To study the role of hormonal imbalance in the development of abnormal uterine bleeding (AUB) in women associated with ovulatory dysfunction. Materials and Methods: The study included 100 women with AUB associated with ovulatory dysfunction, of which 50 women were of early reproductive age (Group I) and 50 women were of late reproductive age (Group II). The control group consisted of 30 healthy women without menstrual cycle disorders and signs of ovulatory dysfunction. The study involved the collection of anamnesis, gynecological examination, transvaginal ultrasound, hormonal analysis (determination of estradiol, progesterone, FSH, LH, prolactin, and testosterone levels), and biochemical blood analysis. Statistical processing was performed using SPSS version 25.0. Results: The average age of women with AUB of early reproductive age was 28.3 ± 4.1 years, and for women of late reproductive age, it was 39.5 ± 3.7 years. Body mass index (BMI) was comparable across all groups. Hormonal analysis showed that estradiol, FSH, LH, and prolactin levels were significantly higher, while progesterone levels were significantly lower in women with AUB associated with ovulatory dysfunction compared to the control group. Correlation analysis revealed significant associations between hormone levels and clinical manifestations of ovulatory dysfunction. Conclusion: Women with abnormal uterine bleeding caused by ovulatory dysfunction exhibit characteristic hormonal changes, including high levels of estradiol, low levels of progesterone, and elevated levels of FSH, LH, and prolactin. These changes can serve as markers for the diagnosis and prognosis of AUB and for the development of targeted therapeutic strategies. Regular monitoring of hormonal indicators and a comprehensive approach to treatment are necessary to optimize clinical outcomes in women with AUB associated with ovulatory dysfunction.
Keywords: Abnormal uterine bleeding, Ovulatory dysfunction, Hormonal imbalance, Diagnostic markers, Therapeutic strategies
Cite this paper: Abraeva N. N., Shukurov F. I., The Role of Hormonal Imbalance in the Development of Abnormal Uterine Bleeding in Women Associated with Ovulatory Dysfunction, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 2127-2132. doi: 10.5923/j.ajmms.20241408.37.
Article Outline
1. Introduction
- Abnormal uterine bleeding (AUB) is one of the most common gynecological conditions, significantly impacting women's health and quality of life [1]. These disturbances may manifest as changes in the duration, intensity, and frequency of menstrual cycles, leading to discomfort and serious medical issues [2]. One of the key causes of AUB is ovulatory dysfunction, which results in the disruption of the normal menstrual cycle and hormonal balance [3]. Ovulatory dysfunction is characterized by irregular or absent ovulation, leading to a deficiency of progesterone and a relative excess of estrogens [4]. This hormonal imbalance is the primary factor causing abnormal uterine bleeding [5]. Normally, after ovulation, progesterone levels increase, promoting the transformation of the endometrium and preventing its excessive growth [6]. In the case of ovulatory dysfunction, this mechanism is disrupted, leading to endometrial hyperplasia and its instability [7]. Recent studies have shown that hormonal changes play a key role in the pathogenesis of AUB caused by ovulatory dysfunction [8]. Specifically, levels of estradiol, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) are important markers that allow the assessment of the reproductive system's condition and the identification of ovulatory disorders [9-11]. For example, a study by Jones and Sung (2023) demonstrated that women with AUB exhibit significant deviations in LH and FSH levels compared to the control group [12]. Another study by Zhang et al. (2023) confirmed that low progesterone levels are one of the main factors predisposing women to the development of AUB [13].Despite existing data, the role of hormonal changes in the pathogenesis of AUB caused by ovulatory dysfunction remains insufficiently studied [14]. Further research is needed to gain a more detailed understanding of these mechanisms and to develop effective diagnostic and therapeutic approaches [15-17]. In particular, it is important to conduct a comprehensive analysis of the hormonal status in women with various forms of AUB to identify specific patterns associated with ovulatory dysfunction [18]. The relevance of this study is driven by the high prevalence of AUB among women of reproductive age and the significant challenges in diagnosing and treating this condition [19]. Understanding the hormonal mechanisms underlying these disorders will allow the development of more effective diagnostic and therapeutic approaches aimed at restoring the normal menstrual cycle and improving the quality of life of patients [20].This study will conduct comprehensive clinical and laboratory investigations, including the analysis of estradiol, progesterone, LH, FSH, and other hormones in women with AUB caused by ovulatory dysfunction [21]. A comparative analysis of hormonal indicators in women with a normal menstrual cycle will also be conducted to identify significant differences and pathogenic mechanisms underlying this pathology [22]. The results of the study will provide a deeper understanding of hormonal changes in AUB associated with ovulatory dysfunction and will contribute to the development of new diagnostic and therapeutic approaches aimed at improving women's reproductive health [23]. This, in turn, may lead to a significant reduction in the incidence of AUB and an improvement in patients' quality of life [24].The aim of this study is to investigate the role of hormonal imbalance in the development of abnormal uterine bleeding in women associated with ovulatory dysfunction.
2. Materials and Methods
- The study included 100 women with abnormal uterine bleeding associated with ovulatory dysfunction. Among them, 50 women with AUB were in early reproductive age (Group I), and 50 women with AUB were in late reproductive age (Group II). The control group consisted of 30 healthy women without menstrual cycle disorders and signs of ovulatory dysfunction. Inclusion criteria were: age between 20 and 45 years, a confirmed diagnosis of ovulatory dysfunction accompanied by abnormal uterine bleeding, absence of current acute infectious diseases, and signed informed consent to participate in the study. Exclusion criteria were: the presence of chronic diseases in the exacerbation stage, intake of hormonal drugs in the last three months, oncological diseases, and the presence of autoimmune diseases. All study participants underwent a comprehensive clinical and laboratory examination, including medical history collection and gynecological examination. Transvaginal ultrasound (TVUS) was performed to assess the structure and thickness of the endometrium and to detect possible pathological changes. Hormonal assessment included the determination of serum levels of estradiol, progesterone, FSH, LH, prolactin, and testosterone, as well as a biochemical blood test to assess overall health. Hormonal studies were performed by enzyme-linked immunosorbent assay (ELISA) using commercial kits. Estradiol, progesterone, FSH, LH, prolactin, and testosterone levels were measured in serum collected from the patients on the 3rd-5th day of the menstrual cycle. Data were statistically analyzed using SPSS software version 25.0. The main statistical methods included descriptive statistics to calculate means and standard deviations, Student's t-test for independent samples in normally distributed data, the Mann-Whitney U test for non-normally distributed data, ANOVA for multivariate analysis, and correlation analysis to identify relationships between hormonal indicators and clinical manifestations. Differences were considered statistically significant at a significance level of p < 0.05. Additionally, regression analysis methods were used to identify predictive factors for the development of AUB associated with ovulatory dysfunction.
3. Research Results
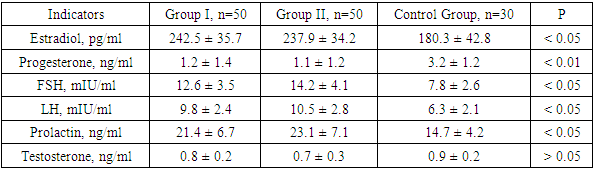
- The study resulted in the following data on the hormonal status of women with abnormal uterine bleeding (AUB) caused by ovulatory dysfunction. The mean age of women with AUB in early reproductive age (Group I) was 28.3 ± 4.1 years, while the mean age of women with AUB in late reproductive age (Group II) was 39.5 ± 3.7 years. In the control group, the mean age of women was 30.1 ± 3.9 years. The body mass index (BMI) was comparable across all groups, with 24.6 ± 2.8 kg/m² in Group I, 25.1 ± 2.9 kg/m² in Group II, and 23.9 ± 2.5 kg/m² in the control group. The distribution by BMI categories showed the following results: in Group I, a normal BMI (18.5–24.9 kg/m²) was observed in 60% of women, overweight (25–29.9 kg/m²) in 30%, and obesity (≥30 kg/m²) in 10%. In Group II, a normal BMI was observed in 55% of women, overweight in 35%, and obesity in 10%. In the control group, a normal BMI was observed in 65% of women, overweight in 25%, and obesity in 10%.A detailed analysis of hormonal studies in women with AUB caused by ovulatory dysfunction revealed differences in hormone levels across the groups. The mean estradiol levels in serum were significantly higher in women with AUB caused by ovulatory dysfunction compared to the control group. In Group I, the estradiol level was 242.5 ± 35.7 pg/ml, in Group II — 237.9 ± 34.2 pg/ml, while in the control group, it was 180.3 ± 42.8 pg/ml (p < 0.05).Progesterone levels were significantly lower in women with AUB caused by ovulatory dysfunction. In Group I, it was 1.2 ± 1.4 ng/ml, in Group II — 1.1 ± 1.2 ng/ml, and in the control group — 3.2 ± 1.2 ng/ml (p < 0.01). FSH levels were higher in women with AUB caused by ovulatory dysfunction compared to the control group. In Group I, the FSH level was 12.6 ± 3.5 mIU/ml, in Group II — 14.2 ± 4.1 mIU/ml, while in the control group, it was 7.8 ± 2.6 mIU/ml (p < 0.05).The mean LH levels in serum were higher in women with AUB caused by ovulatory dysfunction compared to the control group. In Group I, the LH level was 9.8 ± 2.4 mIU/ml, in Group II — 10.5 ± 2.8 mIU/ml, and in the control group — 6.3 ± 2.1 mIU/ml (p < 0.05). Prolactin levels were significantly higher in women with AUB caused by ovulatory dysfunction. In Group I, the prolactin level was 21.4 ± 6.7 ng/ml, in Group II — 23.1 ± 7.1 ng/ml, while in the control group, it was 14.7 ± 4.2 ng/ml (p < 0.05). The mean testosterone levels in serum did not show significant differences between the groups. In Group I, the testosterone level was 0.8 ± 0.2 ng/ml, in Group II — 0.7 ± 0.3 ng/ml, and in the control group — 0.9 ± 0.2 ng/ml (p > 0.05) (see Table 1).
|
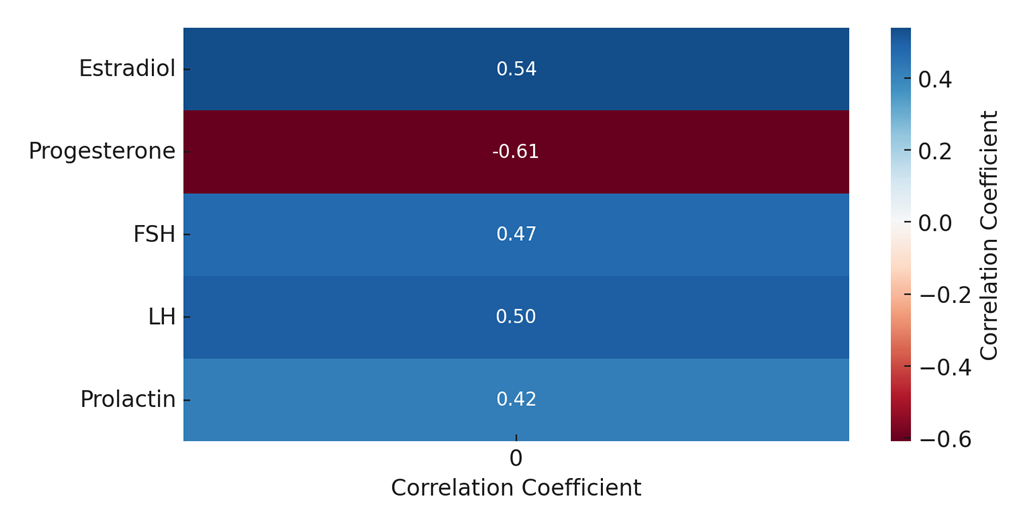 | Figure 1. Correlation Between Hormone Levels and Clinical Manifestations of AUB Caused by Ovulatory Dysfunction |
4. Discussion
- The results of our study demonstrated a significant impact of hormonal imbalance on the development of AUB in women associated with ovulatory dysfunction. The primary changes in hormonal status identified in women with AUB caused by ovulatory dysfunction were high levels of estradiol, low levels of progesterone, as well as elevated levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), and prolactin.High levels of estradiol in women with AUB caused by ovulatory dysfunction support the hypothesis of the role of hyperestrogenism in the pathogenesis of endometrial disorders. The increase in estradiol levels was associated with an increase in the severity of AUB clinical manifestations, highlighting its significance as a prognostic marker. Hyperestrogenism contributes to endometrial hyperplasia and instability, leading to heavy and irregular bleeding. These data are consistent with previous studies, which also point to the key role of estrogens in the development of endometrial disorders and AUB [7].Low progesterone levels in women with AUB caused by ovulatory dysfunction indicate an insufficient luteal phase, leading to impaired secretory transformation of the endometrium. This causes its hyperplasia and instability, which in turn leads to abnormal bleeding. The strong negative correlation between progesterone levels and the severity of clinical manifestations of AUB caused by ovulatory dysfunction underscores the importance of progesterone in maintaining a normal menstrual cycle and endometrial functionality. Progesterone deficiency is one of the key factors predisposing to the development of AUB caused by ovulatory dysfunction and may serve as an important marker for diagnosing and prognosing this pathology.The high levels of FSH identified in women with AUB caused by ovulatory dysfunction reflect a compensatory response of the body to reduced ovarian function and the absence of ovulation. The increase in FSH levels is an attempt to stimulate follicular growth; however, in chronic anovulation, this mechanism does not lead to successful ovulation. This contributes to prolonged and irregular menstrual cycles. The correlation between FSH levels and the duration of anovulatory cycles highlights its significance as a prognostic marker of chronic anovulation and predisposition to the development of AUB caused by ovulatory dysfunction.Elevated LH levels are also associated with the duration of anovulatory cycles. This indicates disruptions in the regulation of the hypothalamic-pituitary-ovarian axis, leading to ovulatory dysfunction and, consequently, to the development of AUB caused by ovulatory dysfunction. Elevated LH levels may serve as a marker for determining the duration of anovulatory periods and the need to correct hormonal imbalances.Elevated prolactin levels in women with AUB caused by ovulatory dysfunction indicate its role in the pathogenesis of ovulatory dysfunctions. Hyperprolactinemia can inhibit gonadotropin secretion, leading to ovulatory dysfunctions and frequent abnormal bleeding. The correlation between prolactin levels and the frequency of AUB caused by ovulatory dysfunction confirms its significance as a marker for assessing the risk of developing this pathology.Our study underscores the importance of a comprehensive assessment of hormonal status in women with anovulatory dysfunction for developing individualized diagnostic and therapeutic strategies. Regular monitoring of estradiol, FSH, and progesterone levels in clinical practice can contribute to the early diagnosis and effective treatment of AUB caused by ovulatory dysfunction. Using these hormonal indicators as markers will allow timely identification of women at risk and the implementation of corrective measures, which will improve clinical outcomes and the quality of life of patients.
5. Conclusions
- The results of our study showed that women with abnormal uterine bleeding caused by anovulatory dysfunction have characteristic changes in hormonal status, including high levels of estradiol, low levels of progesterone, high levels of FSH, LH, and prolactin. These hormonal changes can serve as markers for diagnosing and prognosing AUB caused by ovulatory dysfunction, as well as for developing targeted therapeutic strategies. Our data highlight the need for regular monitoring of hormonal indicators and a comprehensive approach to treating women with abnormal uterine bleeding to optimize clinical outcomes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML