Egamov Yuldashali Suleymanovich1, Durdiev Khamdam Bazarovich2, Botirov Akramjon Kodiraliyevich3, Otakuziev Axmadillo Zokirovich4
1Head of the Department of Surgical Diseases and Civil Defence, Doctor of Medical Sciences, Andijan State Medical Institute, Uzbekistan
2Surgeon at an Emergency Medical Center in the Republic of Karakalpakstan, Uzbekistan
3Head of the Department of Surgical Diseases, Doctor of Medical Sciences, Andijan State Medical Institute, Uzbekistan
4Department of Surgical Diseases, Andijan State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Chronic colostasis (CC) or chronic constipation (CC) is a heterogeneous pathology that combines a complex of general and gastrointestinal symptoms. It is alarming that there have been no further significant improvements in results over the past 20 years. The authors, based on an analysis of the world literature, conclude that the problem of surgical treatment of CC is far from being resolved and many debatable issues remain. Treatment of these patients should be differentiated, and indications for surgical treatment should be well substantiated. This state of affairs is due to a number of controversial tactical and technical issues. Therefore, there is an urgent need to optimize surgical tactics. All of the above served as the subject of this research.
Keywords:
Chronic colostasis, Chronic constipation, Colon, Hemicolectomy, Colonectomy
Cite this paper: Egamov Yuldashali Suleymanovich, Durdiev Khamdam Bazarovich, Botirov Akramjon Kodiraliyevich, Otakuziev Axmadillo Zokirovich, Immediate and Long-Term Results of Surgical Treatment for Chronic Colostasis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 2123-2126. doi: 10.5923/j.ajmms.20241408.36.
1. Relevance of the Problem
Chronic colostasis (CC) or chronic constipation (CC) is a heterogeneous pathology that combines a complex of general and gastrointestinal symptoms [2]. It is alarming that no further significant improvements in results have been observed over the past 20 years [1]. In the vast majority of cases, chronic CC requires surgical treatment. However, the operations are technically complex and are marred by a high rate of unsatisfactory results, which reaches 13-30% [3,6]. In the long term, after performing segmental resections (SR), 21-40% experience a return of signs of constipation [5] or, conversely, the development of persistent diarrhea - 8-20% of cases, and after colectomy with the formation of ileorectoanastomosis, this figure can reach 25% [4,6]. This research is dedicated to improving immediate and long-term results.The aim of the research is to improve the immediate and long-term results of surgical treatment for chronic colostasis by optimizing surgical tactics.
2. Research Materials and Methods
An analysis of the results of examination and treatment of 396 patients suffering from chronic constipation (colostasis) who were undergoing inpatient treatment in the coloproctology department of the Department of Surgery and Civil Defense of the Andijan State Medical Institute and the Ellikkala district Medical Association of the Republic of Karakalpakstan was carried out. The sample of patients upon admission was conditionally divided into two groups:- comparison group – 172 (43.4%) patients with CC in the period from 2015 to 2018, the treatment of which was limited to subsequent standard patient management. - the main group - 224 (56.6%) patients with CC operated on in the period 2019 to 2023, who used an improved treatment and diagnostic algorithm, as well as a modified method of “submersible” intussusception bell anastomosis. To achieve the goal and objectives of the research, general clinical, laboratory, biochemical, instrumental and statistical research methods were carried out according to protocols approved by the Ministry of Health of the Republic of Uzbekistan and Karakalpakstan.
3. Results and Their Discussion
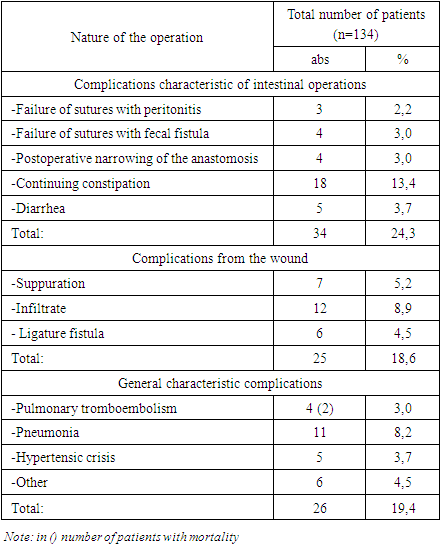
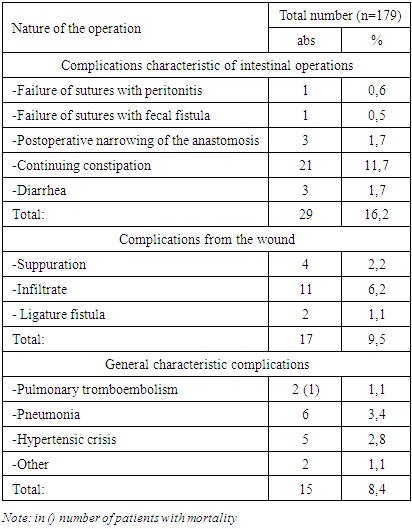
Immediate results. In patients with CC, complications that arose in the groups (comparison and main) were divided into two subgroups, which allows for a full analysis of the treatment results:- postoperative complications specific to operations, i.e. associated with surgery on the large intestine (local); postoperative complications associated with anesthesia, surgical trauma, opening of the abdominal cavity;- postoperative (wound) complications. - complications associated with concomitant diseases that may occur in other organs and systems of the body (general).Table 1. The nature of postoperative complications in the comparison group
 |
| |
|
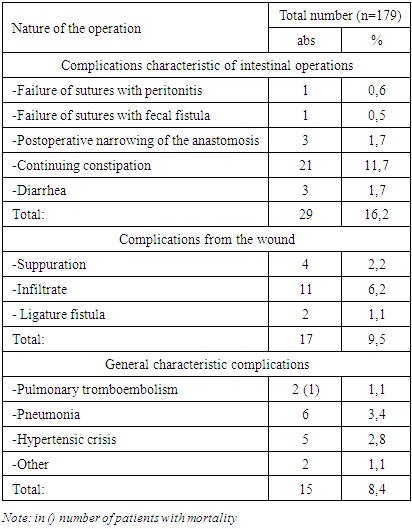
In the comparison group, complications associated with the operation were noted in 34 (25.3%) patients. Of these, suture failure with the development of peritonitis occurred in 3 (2.2%), where relaparotomy was performed in all cases. Suture failure with fecal fistula was noted in 4 (3.0%) patients, which required relaparotomy in all cases. Postoperative narrowing of the anastomosis was noted in 4 (3.0%). Continued constipation was noted in 18 (13.4%) patients, which determines the effectiveness of operations for CC. Diarrhea was noted in 5 (3.7%) patients.In the comparison group, purulent-septic complications (complications from the wound) were diagnosed in 25 (18.6%) patients. Of these, there was wound suppuration in 7 (5.2%), wound infiltration in 12 (8.9%) and ligature fistula in 6 (4.5%) patients.In 26 (19.4%) patients in the comparison group, postoperative complications of a general nature and mortality associated with it were noted. Thus, pulmonary embolism in the comparison group was diagnosed in 4 (3.0%) cases with a fatal outcome in 2 (1.5%) cases. Postoperative pneumonia was diagnosed in 11 (8.2%) patients, hypertensive crisis in 5 (3.7%) patients. Other complications in 6 (4.5%) patients.In the main group, as a result of the use of optimized surgical tactics, complications associated with the operation were noted in 29 (16.2%) patients. Of these, suture failure with the development of peritonitis occurred in 1 (0.6%), where relaparotomy was performed in all cases. Suture failure with fecal fistula was observed in 1 (0.5%) patient. Postoperative narrowing of the anastomosis was noted in 3 (1.7%). Continued constipation was noted in 17 (9.5%) patients, which is significantly lower than in the comparison group. Diarrhea was noted in 7 (3.3%) patients. A comparative analysis showed that in the main group, compared to the comparison group, the frequency of postoperative complications associated with surgery decreased by 9.1% (from 25.3 to 16.2%) (Table 2).Table 2. The nature of postoperative complications in the main group
 |
| |
|
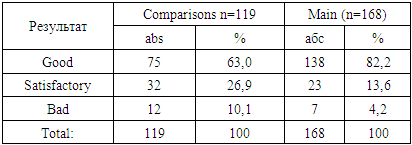
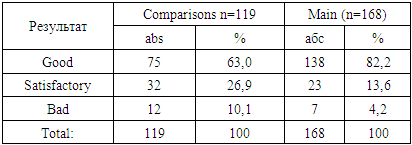
Purulent-septic complications (complications from the wound) in the main group were diagnosed in 17 (9.5%) patients. Of these, there was wound suppuration in 4 (2.2%), wound infiltration in 11 (6.2%) and ligature fistula in 2 (1.1%) patients. A comparative analysis showed that in the main group compared to the comparison group, the frequency of purulent-septic complications decreased by 9.1% (from 18.6 to 9.5%).Postoperative general complications and mortality in the main group were observed in 15 (8.4%) patients. Thus, pulmonary embolism in the comparison group was diagnosed in 2 (1.1%) cases with a fatal outcome in 1 (0.6%) case. Postoperative pneumonia was diagnosed in 6 (3.4%) patients, hypertensive crisis in 5 (2.8%) patients. Other complications in 2 (1.1%) patients. A comparative analysis showed that in the main group, compared to the comparison group, the frequency of overall complications and mortality decreased by 11.0% (from 19.4 to 8.4%).Long-term results. The assessment of long-term results was based on the analysis of data on the frequency of bowel movements, the nature of stool, the dynamics of these parameters, as well as the need for additional drug treatment. In addition, the task was to obtain information about complications in the long-term postoperative period.The results were rated as good, satisfactory or unsatisfactory depending on the absence or presence of symptoms of colostasis, intestinal dyspepsia and the need and duration of conservative treatment. We studied long-term results starting from 1 month after surgery and for periods of 6, 12 months, up to 3 years or more. At the same time, the results of treatment of patients were assessed by the number and nature of bowel movements at various periods after the intervention. Long-term results of treatment of patients were considered depending on the type of surgery undergone.Long-term results of surgical treatment of CC were observed in the comparison group in 119 (90.1%) of 132 and in 168 (94.4%) of 178 patients of the main group in periods from 1 month to 3 years and after surgery. The situation according to the described indicator in patients in the comparison group, the frequency of stool appearance in patients in the first months after the intervention was 1 time per day. Upon further observation, a decrease in the number of bowel movements was noted, starting from 3 months after surgery, to one episode every 2-3 days or less. Subsequently (by 6 months), in all patients, the frequency of bowel movements decreased to 1-2 times a week or less and remained at this level throughout the entire observation period. As the time period (more than 3 years) passed after the intervention increased, the number of patients with a clear stool pattern increased, however, their number was less than in the main group.In the comparison group, 2/3 of the patients had formed stools in the first months after the intervention; 1/3 had firm stools. Three years later, the situation was exactly the opposite: 63.0% (75 of 119) of patients retained formed stools, and 26.9% (32 of 119) had dense stools. The need to use oil suppositories or microenemas was noted by 10.1% (12 out of 119) of patients, while, as previously shown, the frequency of bowel movements in these patients did not exceed 1-2 times a week.In the main group, formed stools were observed in all patients in the first months after the intervention. After three years, 82.2% (138 of 168) of patients retained formed stools, and 13.6% (23 of 168) had dense stools. The need to use oil suppositories or microenemas was noted by 4.2% (7 out of 168) of patients (Table 3).Table 3. Characteristics of long-term results
 |
| |
|
The proposed surgical tactics provided good results in almost 138 (82.2%) patients of the main group. In the comparison group, good results were observed only in 75 (63.0%) patients. The criteria for good results in all studied groups were the absence of symptoms of colostasis with a frequency of defecation once every 1-2 days, formed or semi-formed stool, as well as the absence of the need for additional drug therapy aimed at regulating stool. Satisfactory results meant maintaining the frequency of bowel movements within 1-2 days (hard stools), noted in 32 (26.9%) patients in the main group and in 62 (52.1%) patients in the comparison group. A reduction in stool frequency to 1 time every 4-5 days or less, and the ineffectiveness of conservative treatment was regarded as an unsatisfactory result.Poor results were observed in 7 (4.2% of 168) patients in the main group, and in 12 (10.1% of 132) patients in the comparison group. All patients in the comparison group, constantly or periodically, continued conservative treatment. A number of patients in this group required the use of laxatives, prokinetics and even enemas, which is associated with the development of colostasis symptoms in the long term after the intervention or with a change in the character of stool.In the patients of the main group, the surgical treatment provided a completely acceptable result; in no case did the patients experience stool retention. This effect persisted several years after the intervention, which indicates the correctness of the chosen surgical tactics. In the main group, the need to follow a diet, take normokinetics, enzymes, and prebiotics remained in 4.7% (8 out of 168) of cases in the first months after the intervention. Subsequently, most patients refused medication support. Noteworthy is the decrease in the use of laxatives by 34.4% (from 38.6 to 4.2%). In the comparison group, 121 (96.6%) patients required dieting, normokinetics, enzymes, and prebiotics.The analysis of long-term results carried out in this chapter indicated a clear link between the results and the nature and scope of the intervention undergone. However, to identify other possible reasons affecting treatment results, additional comparative statistical analysis was carried out. A comparative analysis of the results of surgical treatment of chronic CC in the main group made it possible to improve the frequency of good results by 19.2% (from 63.0% to 82.2%), reduce the frequency of satisfactory results by 13.3% (26.9% to 13.2%). 6%) and bad – by 5.9% (10.1% to 4.2%) and achieve the research aim.
4. Summary
Thus, the use of optimized surgical tactics for chronic colostases made it possible to reduce the frequency of postoperative complications associated with surgical intervention decreased from 25.3 to 16.2%, purulent-septic complications decreased from 18.6 to 9.5%, general complications and mortality decreased from 19.4 to 8.4% and an improvement in long-term good results from 63.0% to 82.2% of cases.
References
| [1] | Ivashkin V.T., Shelygin Yu.A., Maev I.V. and others. Diagnosis and treatment of constipation in adults (Clinical recommendations of the Russian Gastroenterological Association and the Association of Coloproctologists of Russia) // Russian Journal of Gastroenterology, Hepatology, Coloproctology. – 2020. –T. 30, No. 6. –P. 69-85. |
| [2] | Nechai I.A. Treatment of chronic colonic stasis (constipation) 2023. https://koloproktolog.ru/stati-o-zabolevaniyakh/khronicheskij-tolstokishechnyj-staz-zapor. |
| [3] | Sakulin K.A., Karpukhin O.Yu. Treatment and diagnostic algorithm for resistant forms of cologne constipation in adults // Bulletin of modern clinical medicine. –2021. -T. 14, No. 3. –P. 38-43. |
| [4] | Khatkov I.E., Kuzmina T.N., Sabelnikova E.A. and others. Resected intestinal syndrome is a term that defines the strategy for treating nutritional deficiency //Dr. RU. – 2020. – T. 19, No. 7. – P. 59-67. |
| [5] | Tsimogiannis K.E., Karlbom U., Lundin E., Graf W. Long-term outcome after segmental colonic resection for slow transit constipation // International journal of colorectal disease. –2019. –Vol. 34, № 6. –P. 1013-1019. |
| [6] | Xie X.Y., Sun K.L., Chen W.H. et al. Surgical outcomes of subtotal colectomy with antiperistaltic caecorectal anastomosis vs total colectomy with ileorectal anastomosis for intractable slow-transit constipation // Gastroenterology report. –2019. –Vol. 7, № 6. –P. 449-454. |
| [7] | Yang Y.P., Shi J., Zhao Z.Y. et al. Subtotal colectomy with antiperistaltic cecosigmoidal anastomosis may be another suitable option for slow transit constipation: Experiences from Chinese people // Medicine. –2020. –V. 99, № 7. – P. 1-6. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML