-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(8): 2085-2088
doi:10.5923/j.ajmms.20241408.29
Received: Aug. 3, 2024; Accepted: Aug. 18, 2024; Published: Aug. 22, 2024

Lipid Profile Status in Patients with Non-Alcoholic Fatty Liver Disease after Bariatric Surgery
Shagazatova Barno Khabibullaevna1, Rakhimova Sitora Khikmatovna2
1MD, DSc, Professor, Tashkent Medical Academy, Tashkent, Uzbekistan
2Basic Doctoral Student, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study is dedicated to analyzing the lipid profile status in patients with non-alcoholic fatty liver disease (NAFLD) in the context of bariatric surgery. Obesity is associated with insulin resistance and a pro-inflammatory state, which contributes to the development of atherogenic dyslipidemia. The aim of the study was to evaluate changes in the lipid profile in patients with morbid obesity before and after gastric bypass and sleeve gastrectomy. The study included 44 patients who were treated in the endocrinology department of TMA and Medion Family Hospital from 2022 to 2024. The evaluation was based on biochemical indicators and lipid profiles before and after surgery. The results showed significant improvement in the lipid profile and reduction in atherogenicity 24 months after surgical intervention, confirming the high effectiveness of these methods in improving metabolic parameters in obese patients.
Keywords: Obesity, Non-alcoholic fatty liver disease, Bariatric surgery, Gastric bypass, Sleeve gastrectomy, Lipid profile, Insulin resistance, Metabolic disorders
Cite this paper: Shagazatova Barno Khabibullaevna, Rakhimova Sitora Khikmatovna, Lipid Profile Status in Patients with Non-Alcoholic Fatty Liver Disease after Bariatric Surgery, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 2085-2088. doi: 10.5923/j.ajmms.20241408.29.
1. Introduction
- Obesity is a global public health problem, significantly increasing the risk of developing various metabolic and cardiovascular diseases. According to data obtained from a review conducted by Huaizhu Wu and C. Ballantyne, obesity leads to insulin resistance and chronic inflammation affecting various tissues, including adipose, skeletal muscles, liver and brain [13]. Studies have repeatedly confirmed the association of obesity with the presence of insulin resistance in peripheral tissues and a pro-inflammatory condition caused mainly by the release of various cytokines and hormones by adipose tissue [7]. These factors contribute to the development of atherogenic dyslipidemia, characterized by low levels of high-density lipoprotein cholesterol (HDL), hypertriglyceridemia and elevated levels of low-density lipoprotein cholesterol (LDL).In the context of the growing prevalence of morbid obesity and concomitant disorders of carbohydrate metabolism, surgical methods of treatment, such as gastric bypass surgery and drainage resection, are becoming more and more in demand. The effectiveness of these methods in relation to changes in the lipid profile has been evaluated in various studies. For example, a study conducted by K. Herzog and colleagues showed that Roux-en-Y gastric bypass (RYGB) causes significant changes in lipid metabolism, which indicates a significant effect of surgery on the metabolic profile of patients [6]. The study by M. Piché and the College analyzed the implementation of various methods of bariatric surgery on the lipid profile and lipoprotein metabolism. The author noted a significant improvement in the lipid profile, including a decrease in total cholesterol, LDL and triglycerides, as well as an increase in HDL levels after surgery (Piché et al., 2021).The introduction of bariatric surgery in obese people in Uzbekistan determined the purpose of our study - to study the state of the lipid profile against the background of surgical interventions.The purpose of the study. To study the state of the lipid profile in patients with morbid obesity before and after bariatric surgery in Uzbekistan.
2. Materials and Methods
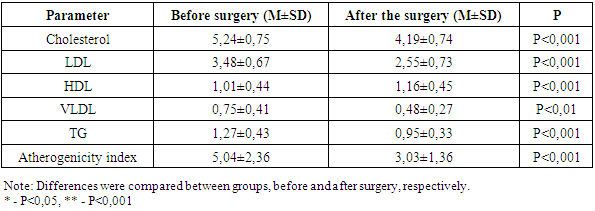
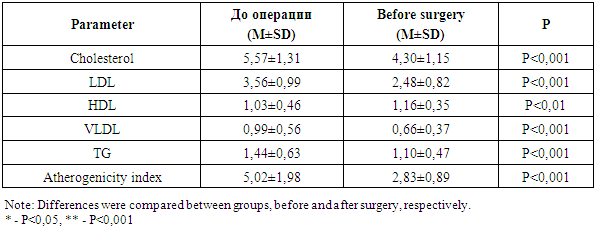
- The number of examined patients was 44 patients who were on inpatient and outpatient treatment at the Department of Endocrinology of TMA and CHK Medion Family Hospital, where surgical interventions were performed, in the period from 2022 to 2024. The age of the patients was 38.59±8.77 years. There were 4 men (9.1%) and 40 women (90.9%). The average weight of the patients was 108.88±15.70 kg, and the BMI before surgery was 40.19±5.97 kg/m2.The patients were divided into two groups depending on the method of surgery:ü Gastric bypass (n=19.44%)ü Drain resection (n=25.56%)Patients taking hypolipidemic drugs were excluded from the study. The indication for the type of surgical intervention was the presence of morbid type of obesity or impaired carbohydrate metabolism in patients.The patients underwent a liver examination using a fibroscan. In the same group, along with studying the condition of the liver, we also analyzed the lipid profile in groups of patients with different surgical approaches.All patients underwent general clinical research methods, including assessment of lipid metabolism, both before and after surgery.The analysis of the lipid profile was carried out in the laboratory of the Department of Endocrinology THERE and the CHEKA Medion Familia Hospital. The following parameters were measured: total cholesterol, low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL), very low-density lipoprotein cholesterol (VLDL), triglycerides (TG), the atherogenicity index was calculated.The follow-up period of the patients was 24 months. Statistical data analysis was performed using the IBM® SPSS Statistics 25.0 software package. The normality of the data distribution was checked using the Kolmogorov-Smirnov test. The Mann-Whitney criterion and the Fisher exact criterion were used for comparative analysis. Quantitative data were presented as an average value ± standard deviation. The differences were considered statistically significant at a significance level of p < 0.05.
3. Results and Discussion
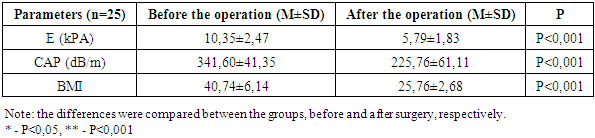
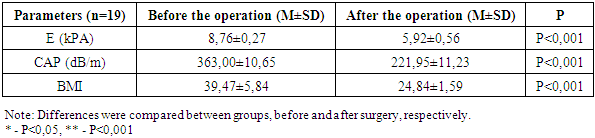
- Our study involved 44 patients, of whom 90.9% were women and 9.1% were men. The average age of the participants was 38.59 years, the average weight was 108.88 kg, and the average body mass index (BMI) before surgery was 40.19 kg/m2. The patients were divided into two groups depending on the type of surgery: gastric bypass and drainage resection. The dynamics of BMI changes showed a significant decrease in BMI in the group of patients who underwent surgical resection (Table 1).A decrease in BMI occurred by 63.2% after surgery (P<0.01).
|
|
|
|
4. Conclusions
- Our study confirms the significant positive effect of bariatric surgery on the lipid profile and overall metabolic status of patients with morbid obesity and non-alcoholic fatty liver disease.Both gastric bypass and drainage resection resulted in significant improvements in the lipid profile, including a decrease in total cholesterol, LDL and triglycerides, as well as an increase in HDL levels. These changes contribute to reducing the risk of cardiovascular diseases and improving the overall metabolic status of patients.Thus, bariatric surgery is an effective method of treating morbid obesity, contributing to theimprovement of both the lipid profile and the overall metabolic state of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML