Xaitov Qaxramon Najmitdinovich1, Sultanov Akram Abduxalikovich2
1Department of Skin Venereal Diseases, Children's Skin Venereal Diseases and AIDS, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
2Department of Dermatovenereology and Cosmetology, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Sultanov Akram Abduxalikovich, Department of Dermatovenereology and Cosmetology, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article is devoted to the method of early and timely treatment of cutaneous leishmaniasis in the practice of dermatovenerologists and general practitioners, which serves to correctly organize the approach to early treatment of this disease in primary health care and inpatient conditions, to prevent complications, and to take preventive measures. The methods given in this recommendation are of particular practical and scientific importance in improving the effectiveness of treatment of cutaneous leishmaniasis, systematic introduction of prevention of serious complications, improvement of service quality.
Keywords:
Cutaneous leishmaniasis, Medical care, Epidemic, Prevention, Carrier
Cite this paper: Xaitov Qaxramon Najmitdinovich, Sultanov Akram Abduxalikovich, Methods of Local Treatment of Cutaneous Leishmaniosis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 2074-2081. doi: 10.5923/j.ajmms.20241408.27.
1. Introduction
In Uzbekistan, cutaneous leishmaniasis is one of the widespread parasitic diseases with a significant share in the country's pathology. A high rate of zoonotic cutaneous leishmaniasis is observed in Turkmenistan and Uzbekistan from the Central Asian countries, where tens and hundreds of new cases of this disease are recorded every year in endemic areas [1,9].Epidemiological studies have shown certain seasonality for cutaneous leishmaniasis. The first patients appear at the end of May, then the incidence increases and reaches a maximum in September-October, then a gradual decrease in the incidence is noted, and in winter, as usual, one-and-a-half cases of zoonotic cutaneous leishmaniasis can be observed, and this applies to patients who seek medical care late [2,13].Leishmaniasis (leishmanioses) is a group of protozoan diseases transmitted from humans and animals [4,21].About 500 species of mosquitoes are known, 30 of which are carriers of leishmaniasis. Leishmaniasis (or leishmania) is a group of diseases caused by intracellular protozoa of the genus Leishmania [5,11].According to the characteristics of their morphological structure, leishmaniasis agents are divided into amastigote and promastigote forms. The development cycle of amastigote forms takes place in the organism of humans and other mammals, and that of promastigote forms takes place in the organism of mosquitoes of the genus Phlebotomus.Leishmaniasis is still one of the most neglected diseases in the world, mainly affecting the poorest of the poor in developing countries; it is estimated that 350 million people are at risk of leishmaniasis and about 2 million new cases are diagnosed annually [6,18].Two forms of human leishmaniasis are distinguished: damage to the lymphohistiocytic system, recurrent fever, cachexia, worsening anemia, leukopenia, visceral leishmaniasis (leishmaniosis visceralis), which is characterized by a sharp enlargement of the spleen and mainly affects the skin (mucous membranes), the process is characterized by the appearance of ulcers and cutaneous leishmaniasis (leishmaniosis cutanea), which is later manifested by scarring. Both forms include different geographic and clinical-epidemiological variants [7,20].There are many local names of the disease, which are mainly derived from geographical names (Ashkhabad, Kokan, Baghdad, Eastern ulcer, Aleppo ulcer, Pendi ulcer, etc.), previously this disease was often called Borovsky's disease.The epidemiology of leishmaniasis depends on the characteristics of the parasite species, the local ecological characteristics of the places of infection, the current and previous exposure of the human population to the parasite, and the widely variable behavior of people [8,12].Ta’kidlash joizki, teri leyshmaniozi qo‘zg‘atuvchisining tabiiy rezervuarlari qizil dumli va katta qumsichqonlar, tashuvchilari esa iskabtopar chivinlardir (Phlebotomus papatasi). Katta qumsichqonlarning teri leyshmaniozi bilan zararlanish darajasi turli o‘choqlarda 12,3-98,2%, qizil dumli qumsichqonlarniki esa 9,2-15,2% ni tashkil qiladi. O‘zbekiston hududida leyshmaniyaning uch turi aniqlangan: L.major, L.turanica, L.gerbilli. Odamlarda zoonoz teri leyshmaniozining tipik kechishini faqat L.major chaqiradi, ammo L.turanica odamlarda dermatozning kechishini keltirib chiqarishi mumkin va keyinchalik L.major ga nisbatan immunitet hosil bo‘lishiga olib kelishi mumkin [10,22].In cutaneous leishmaniasis, the incubation period can be from several days to 3-4 weeks, and in rare cases, 1-2 months.The pathological process begins primarily at the point of entry of the pathogen into the skin, as a result of which P.V. A granuloma called leishmanioma develops by Kozhevnikov. Leishmanioma develops cyclically and self-heals: incubation, proliferation (papule, tubercle, infiltrate), destruction (wound) and reparation (scarring) stage. Many foci of injury are explained by superinfection, secondary leishmaniomas appear after primary leishmaniomas, and multiple simultaneous bites of female wasps during blood-sucking [13].An important clinical sign of cutaneous leishmaniasis is leishmaniomas, the number of which is highly variable.It should be noted that cutaneous leishmaniasis is one of the few protozoan diseases, the infection of which leads to the development of stable, long-term and strong immunity.Issues of immunity in cutaneous leishmaniasis have been discussed for many years [8,14,23]. Most authors explain the presence of persistent immunity of cutaneous leishmaniasis with the development of a cellular immune response in the human body as a result of the transferred disease [15]. In addition to cellular immunity, humoral immunity is also of particular importance, and it can affect the synthesis of special antibodies [8,9,19].Widely variable profiles of Th1 and Th2 cytokines are found in local cutaneous leishmaniasis lesions and detected in vitro as an immune response to Leishmania antigens. IL-10 and IL-13 are associated with chronic wounds. IL-4 rarely shows stable presence and is detected in low concentrations. IL-10 has been reported to be produced mainly by monocytes and CD4+, CD25+ T-regulatory 18 cells in wounds induced by L. braziliensis and L. guyanensis. The role of T-regulatory cells in human leishmaniasis is still unclear, but these cells are more involved in chronic lesions (WHO report, 2010) [20,21].Thus, this problem is of great scientific and practical interest and, taking into account the growth of cutaneous leishmaniasis in our region, allows us to rightly include this problem in the field of activity of the dermatovenerology service and help us to solve the epidemiological, pathogenetic, therapeutic and other aspects of this disease.Diagnosis of the disease is of great importance in any pathology, it should be affordable for everyone with high sensitivity, low cost and specificity.The diagnosis of leishmaniasis is based on the identification of the pathogen in the pathological material taken from the patient, and in some cases, the use of allergic skin reactions and immunological methods.The above-mentioned methods of diagnosing leishmaniasis do not have the same effectiveness and differ in their specificity and sensitivity. Currently, along with the use of new sensitive and specific tests such as polymerase chain reaction (PSR), classical methods are also used. A comparative study of the effectiveness of diagnostic methods in cutaneous and visceral leishmaniasis continues.The microscopic method used in leishmaniasis is characterized by its simplicity, cheapness and acceleration of results. The microscopic method in cutaneous leishmaniasis is based on the detection of amastigote forms in smears taken from the scraping of the patient's skin or obtained by aspiration, and in visceral leishmaniasis, the detection of these forms in smears prepared from biopsies taken from the spleen, bone marrow, lymph nodes, and in some cases - from venous blood and stained by the Giemza method.. However, the specificity of this method is underestimated.The advantage of detecting parasites in a smear using a microscopic method is that this method is simple, economical, and results can be obtained in a short time. The disadvantage of the method is that it is difficult to detect parasites in the examined material due to the small number of parasites in the field of vision in chronic skin wounds. At the same time, the atypical morphology of parasites also complicates the diagnosis.The golden method of diagnosing leishmaniasis, as in other infectious diseases, remains culture, that is, the cultural (parasitological) method. However, the diagnostic value of the method is reduced by the dependence of its sensitivity on the level of parasite density in the studied material. Thus, it is very difficult to detect promastigotes in the examination of wound samples in cutaneous leishmaniasis and venous blood samples in visceral leishmaniasis. In the asymptomatic form of visceral leishmaniasis, the detection of promastigotes in culture sometimes takes up to 6 months, which complicates the timely treatment of this disease, but is of great preventive value [22].In the diagnosis of leishmaniasis, especially in visceral leishmaniasis, immunological methods based on the detection of antibodies against the pathogen in blood serum are widely used [4,10].Another line of treatment for cutaneous leishmaniasis is the use of sulfone drugs used to treat leprosy patients, particularly dapsone or DDS (diaminodiphenylsulfone), which has been used since 1941. Dapsone was administered at a dose of 200 mg per day to 120 patients with cutaneous leishmaniasis, resulting in clinical recovery in 82% of patients. The anti-leishmaniasis effect was assumed to be related to the effect of dapsone on the synthesis of phospholipids and folic acid [4].Thus, there are various systemic and local methods of treatment of cutaneous leishmaniasis, which have a certain etiotropic and clinical effect, while the incidence of metalleishmaniasis depends on the initial clinical presentation of cutaneous leishmaniasis. may be, therefore, the development of pathogenetically based, complex therapy methods continues, as it is necessary to take into account the degree of expression of residual scar atrophy of the skin after cutaneous leishmaniasis. The purpose of the study. Improvement of the method of pathogenetic treatment of cutaneous leishmaniasis and development of preventive measures based on the study of immuno-microbiological research.
2. Materials and Methods
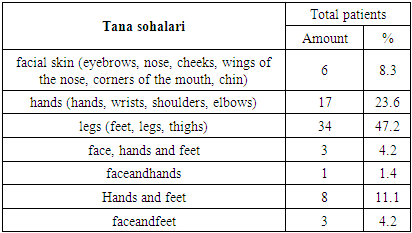
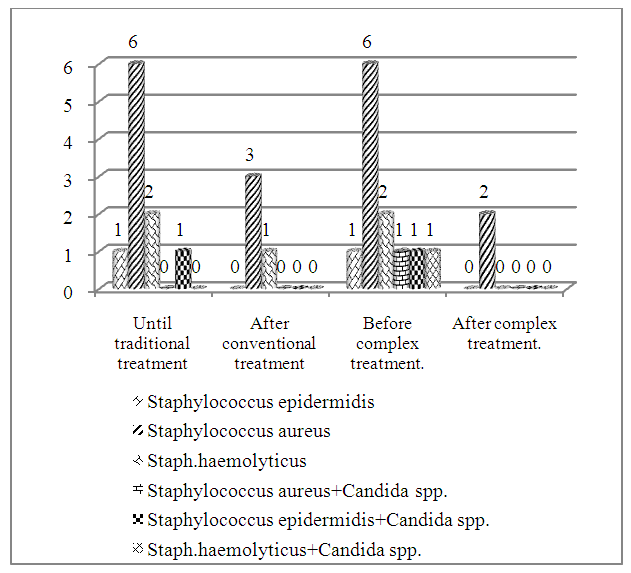
72 patients aged 1 to 82 years with cutaneous leishmaniasis were observed, of which 36 (50.0%) were men and 36 (50.0%) were women.The duration of the disease was from 1 to 4 months, including 9 (12.5%) patients up to 2 months and 63 (87.5%) patients from 3 to 4 months (Fig. 1).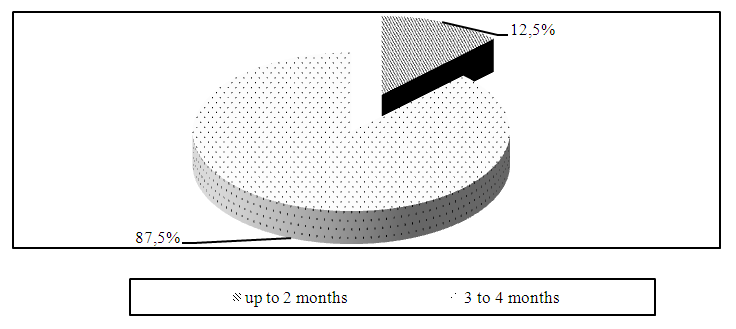 | Figure 1. Distribution of patients with cutaneous leishmaniasis according to the duration of the disease |
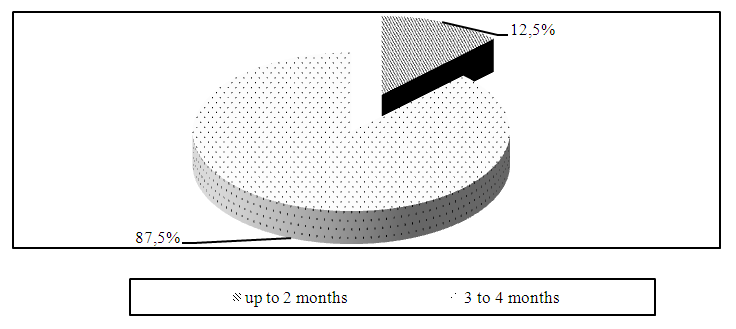
The analysis of the distribution of patients according to the clinical forms of cutaneous leishmaniasis showed that tubercular form was detected in 50 (69.4%) patients and ulcerative leishmaniomas in 22 (30.6%) patients (Fig. 2).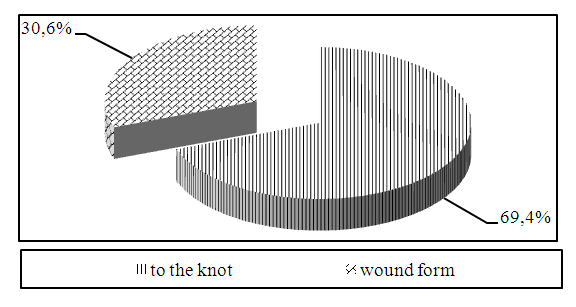 | Figure 2. Distribution of patients according to the clinical form of cutaneous leishmaniasis |
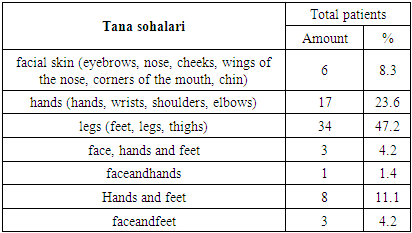
Material and methods. Before starting the treatment, the patients underwent a complete clinical and laboratory examination, including a microscopic examination of exudates from the lesions to identify Borovsky's corpuscles.Microscopic examination revealed leishmania in smears taken from the affected area of the skin in all patients. L. infantum was detected in all patients in the determination of the species composition.Among the examined patients, damage to the skin of the face (eyebrows, nose, cheeks, nosebleeds, corner of the mouth, chin) in 6 (8.3%) patients, damage to the skin of the hands (paws, wrists, shoulders, elbows) in 17 (23, 6%), leg skin (paws, calves, thighs) - 34 cases (47.2%), 3 cases (4.2%) on the face, upper and lower arms, 1 case of damage to the skin of the face and limbs (1.4%), damage to the skin of the limbs was recorded in 8 (11.1%), damage to the skin of the face and feet - 3 (4.2%) patients (Table 1).Table 1. Patients with cutaneous leishmaniasis distribution by affected areas of the body
 |
| |
|
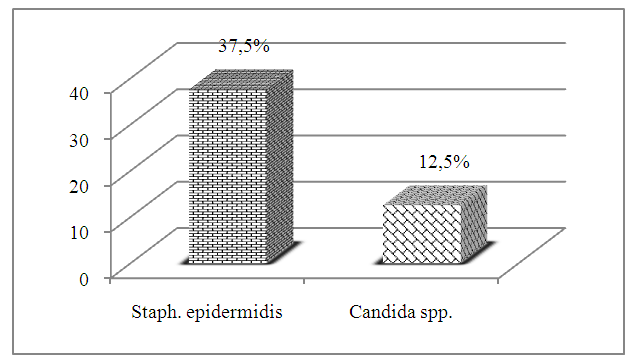
It is known that the accompanying microflora in some cases can affect the clinical course of the pathological process on the skin. Therefore, it is important to study the role of the secondary microflora in foci of cutaneous leishmaniasis and the mechanism of its influence on the clinical appearance of the disease.Therefore, we studied the condition of the accompanying microflora of the skin in lesions in patients with cutaneous leishmaniasis.The condition of skin microflora in 72 patients with cutaneous leishmaniasis was compared with the data of 16 practically healthy individuals (control group). Among the examined patients, 50 patients had tubercular form of cutaneous leishmaniasis and 22 patients had ulcerated leishmaniomas.In the study of secretions obtained by washing the skin from individuals in the control group, Staphylococcus epidermidis was found in 6 (37.5%) patients and Candida Spp. in 2 (12.5%) patients. determined, which constitutes the microbial landscape of the skin in practically healthy individuals (Fig. 3).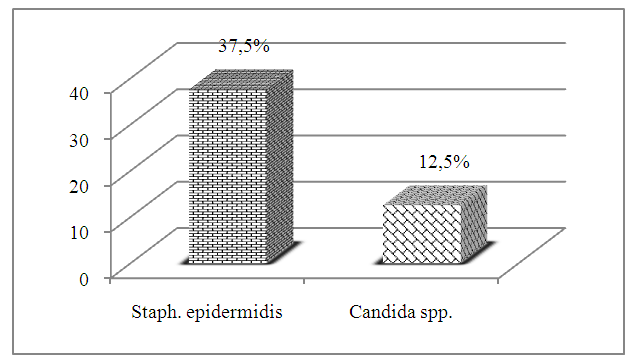 | Figure 3. The frequency of observation of accompanying microflora in skin washing fluid in individuals of the control group |
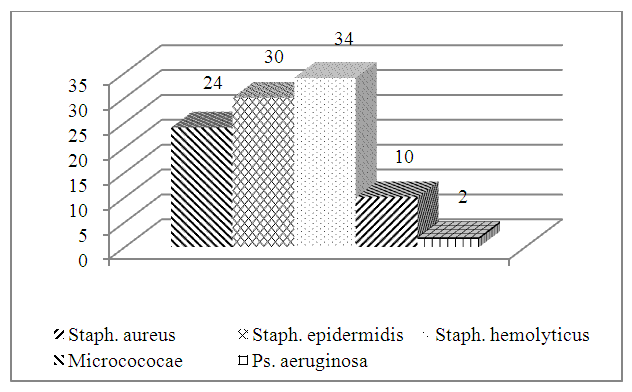
The study of the condition of accompanying skin microflora depending on the clinical forms of skin leishmaniasis in patients showed that as a result of the cultural study of secretions obtained from washing the skin, different microflora were identified in the foci of damage.Studies conducted in patients with tubercular form of cutaneous leishmaniasis showed that in 15 (30.0%) cases - Staphylococcus epidermidis, 12 (24.0%) cases - Staphylococcus aureus, 17 in (34.0%) cases – Staph. haemolyticus, in 5 (10.0%) cases – Microcococae and in 1 (2.0%) case – Ps. aeruginosa was found (Fig. 4).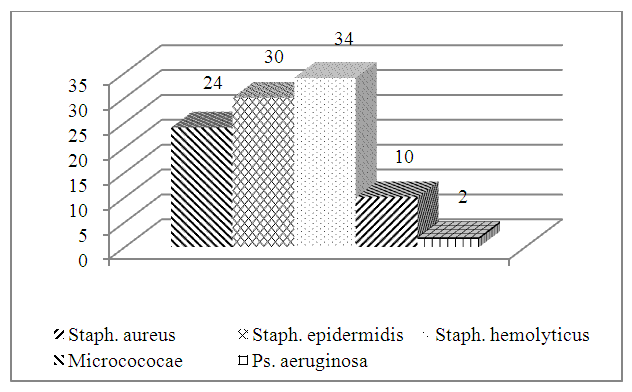 | Figure 4. The frequency of observation of accompanying microflora in secretions obtained during skin washing in patients with tubercular form of cutaneous leishmaniasis (%) |
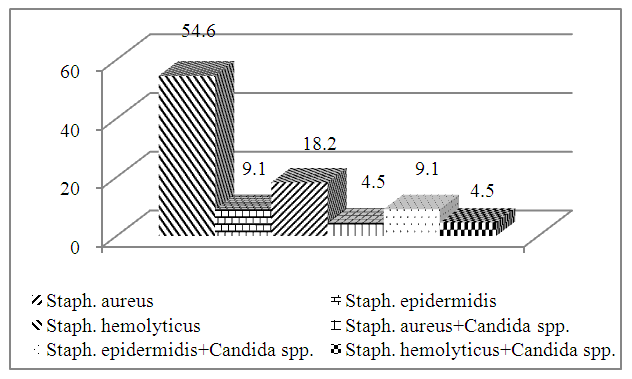
The study of microflora determined in skin washes of patients with ulcerative leishmanioma showed that in patients with this clinical form of the disease, Staphylococcus epidermidis was present in 2 (9.1%) patients, Staphylococcus aureus – 12 (54.6%), Staph.haemolyticus – 4 In (18.2%) cases, a combination of Staphylococcus aureus and Candida spp. - in 1 (4.5%) case, a combination of Staphylococcus epidermidis and Candida spp. – in 2 (9.1%) cases and Staphylococcus aureus and Candida spp. compound - found in 1 (4.5%) case (Fig. 5).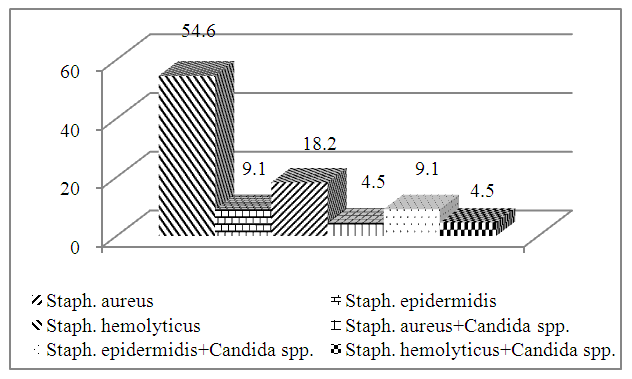 | Figure 5. Frequency of accompanying microflora in skin washes in patients with ulcerative leishmanioma (%) |
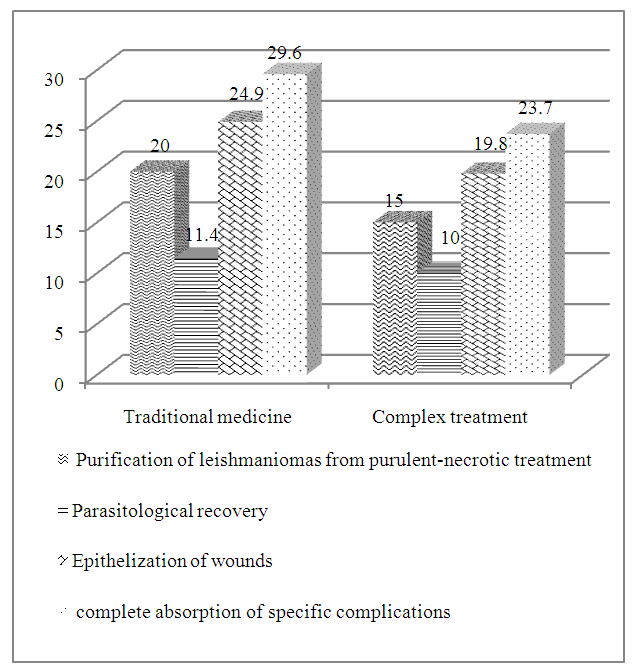
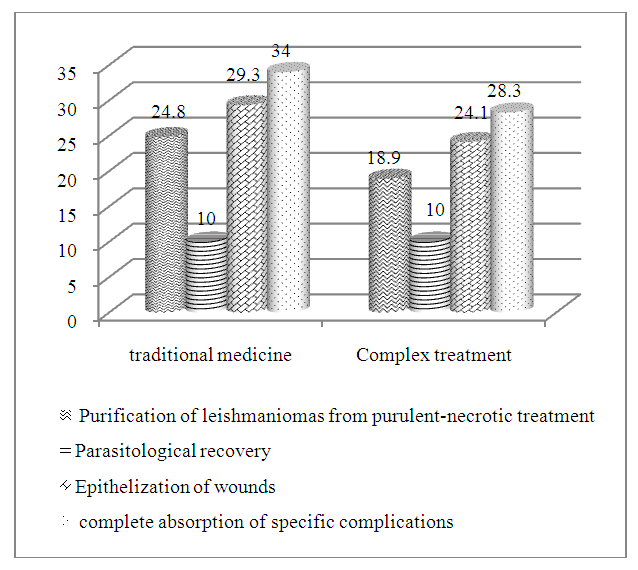
The results of the study showed that in all clinical forms of cutaneous leishmaniasis, the main causative agent is combined with a companion, and this is directly related to the clinical forms of the disease. It should be noted that optimal conditions and the symbiosis of these microorganisms are the main factors contributing to the development and exacerbation of cutaneous leishmaniasis.Taking into account the above, we used the drug "Baneocin" locally to restore the disorders identified in the treatment complex of patients with cutaneous leishmaniasis.Baneocin is a combined antibacterial drug intended for external use. It contains two antibiotics with bactericidal effect - neomycin and bacitracin. Bacitracin is a polypeptide antibiotic that inhibits the synthesis of the cell membrane of bacteria. Neomycin is an aminoglycoside antibiotic that inhibits bacterial protein synthesis. Bacitracin is active against gram-positive (Streptococcus spp. / including hemolytic streptococcus/, Staphylococcus spp.) and some gram-negative microorganisms. Resistance to bacitracin rarely develops. Has good tissue permeability; inactivation by biological products, blood and tissue components is not observed. Neomycin is active against gram-positive and gram-negative bacteria. Due to the use of a combination of these two antibiotics, a wide range of action of the drug and a synergistic effect against a number of microorganisms, for example, staphylococci, are achieved.Baneocin was applied topically 2 times a day for 14 days.According to the method of treatment, the patients were divided into two groups: the first group (conventional group), which was the comparison group and received the main therapy (vitamins, hepatotropic drugs, antifungal drugs) and epithelization-accelerating and local disinfectants 32 patients were included; the second group (complex therapy) included 40 patients who made up the main group, who were prescribed the drug "Baneosin" against the background of traditional therapy.The criteria for the effectiveness of the therapy were the duration of purulent-necrotic treatment of leishmaniomas, parasitological recovery, epithelization of wounds and complete absorption of specific complications of zoonotic cutaneous leishmaniasis.The results of the study showed that the recovery from purulent-necrotic leishmaniasis in patients with the tuberous form of cutaneous leishmaniasis was on average 15.0 ± 0.36 days in the main group, and 20.0 ± 0 in the group of conventionally treated patients. It was equal to 43 days. In this group of patients, parasitological recovery occurred in an average of 11.4 ± 0.75 days after conventional therapy, and epithelization of wounds was completed in 24.9 ± 0.43 days of treatment. And in complex treated patients, parasitological recovery occurred after an average of 10.0 ± 0.00 days, and wound epithelization was completed in 19.8 ± 0.41 days of treatment. In patients of this group, complete absorption of specific complications after traditional therapy occurred in 29.6 ± 0.43 days, and in patients who received complex treatment, in 23.7 ± 0.38 days of treatment.The above indicates that the complex method of treatment of patients with the tubercular form of cutaneous leishmaniasis leads to early removal of leishmaniomas from purulent-necrotic plaques, parasitological healing, epithelization of wounds and complete elimination of specific complications, compared to the traditional method of treatment. it helps.In the patients with ulcerative leishmanioma in the conventionally treated group, leishmanioma clearance from purulent-necrotic stage took an average of 24.8 ± 0.65 days, parasitological recovery - 10.0 ± 0.00 days, wound epithelization - 29, 3 ± 6.3 days, and complete absorption of specific complications corresponded to 34.0 ± 0.61 days of treatment. In the main group, purulent-necrotic treatment of leishmaniomas took an average of 18.9 ± 0.56 days, parasitological recovery took 10.0 ± 0.00 days, wound epithelization took 24.1 ± 0.69 days, and complete resolution of specific complications occurred at 28.3 ± 0.71 days after treatment (Fig. 7).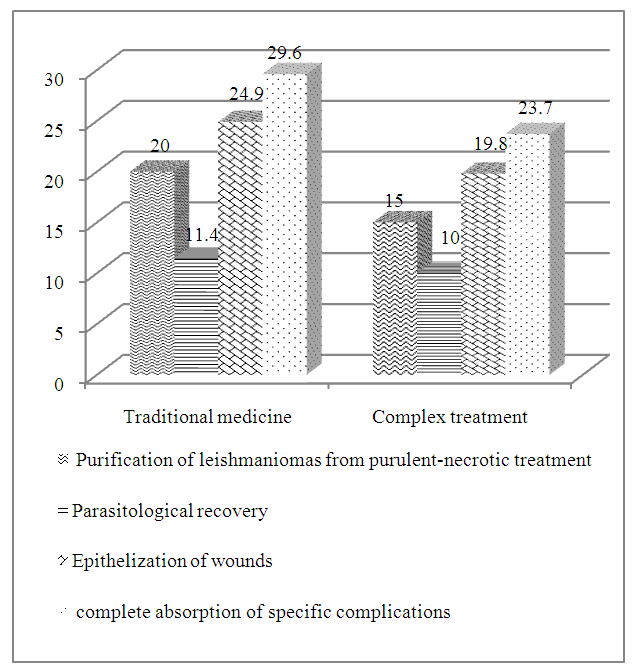 | Figure 6. Periods of remission of pathological symptoms depending on the method of treatment of patients with tuberous form of cutaneous leishmaniasis |
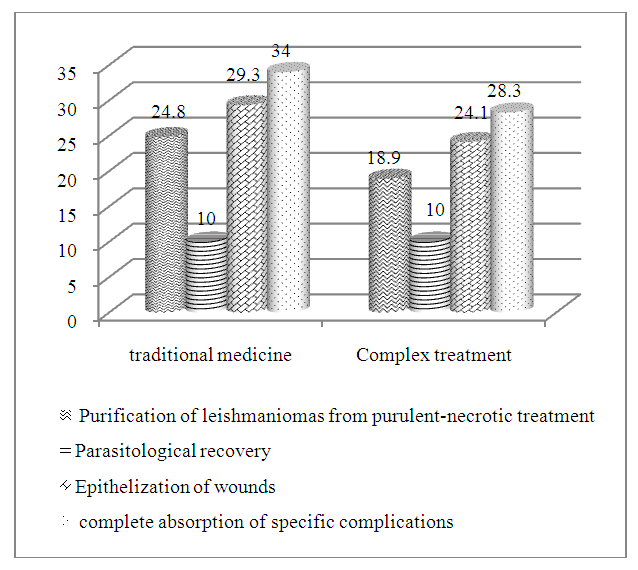 | Figure 7. According to the period of elimination of pathological symptomsmethod of treatment of patients with ulcerative leishmanioma |
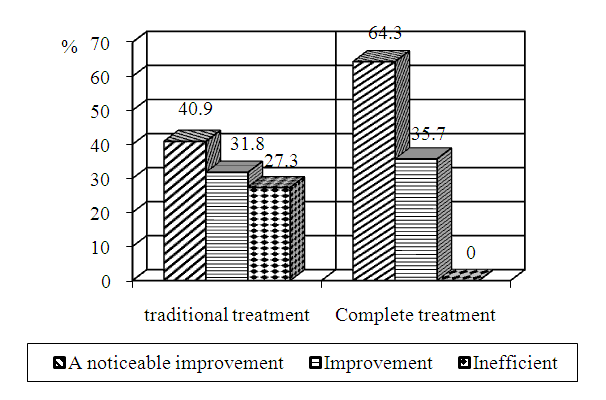
It should be noted that after the treatment method developed in this group of patients, in comparison with traditional therapy, leishmaniomas were cleared from purulent-necrotic appearance, parasitological recovery, epithelization of wounds and complete absorption of specific complications were observed in the early periods of treatment. However, in this examined group, indicators were less pronounced than in patients with tuberous form of cutaneous leishmaniasis.It should be noted that bacteriological studies (detection of leishmania) were carried out at the beginning of treatment, 10, 20 and 30 days after the start of treatment. Leishmania was detected in 100% of cases at the start of treatment in both groups, which was evidence of the diagnosis of zoonotic cutaneous leishmaniasis. A bacteriological study conducted 10 days after the start of treatment showed that simple organisms continued to be detected in 15 (46.9%) of 32 patients treated conventionally, while only 8 (20) of 40 patients treated with complex.9%) this situation was observed. After 20 days of treatment, 5 (15.6%) patients who received conventional treatment continued to detect leishmanias in lesions, and only 3 (7.5%) patients who received complex treatment had simple organisms. After 30 days of treatment, leishmania was isolated from 2 (6.3%) patients who received conventional treatment, while all analyzes showed negative results in the group of patients who received complex treatment. The obtained data show that the parasitological recovery was more pronounced in complex treated patients and occurred earlier.In addition, it was found that healing of leishmaniasis wounds depends on their location, size and clinical form of cutaneous leishmaniasis. When ulcerative leishmaniomas are located on the surface of the limbs, and especially in the area of joints, the periods of purulent-necrotic treatment, epithelization and scarring are slowed down. If the wounds were located on the face and neck, the healing time was shortened, and on the contrary, it was prolonged when located on the distal parts of the limbs, especially the heels. Perhaps this is due to the characteristics of the blood supply and the frequency of injuries and diagnostic errors in these areas.Therefore, the introduction of the local preparation "Baneocin" into the complex of treatment of patients with cutaneous leishmaniasis helps to eliminate the pathological symptoms faster compared to the group of patients receiving traditional therapy.The direct results of the treatment were evaluated according to the following criteria: significant improvement of the condition - complete elimination of pathological symptoms, improvement of the condition - clearing of leishmaniomas from purulent-necrotic appearance, parasitological recovery, ineffective - lack of positive therapeutic effect.Clinical observations showed (Figure 8) that in patients with tuberous tubercular form of cutaneous leishmaniasis, significant improvement was noted in 18 (64.3%) patients in the main group (28 patients) and 10 (35.7%) the patient's condition has improved. However, 9 (40.9%) of the patients (22 patients) who were treated conventionally showed significant improvement, 7 (31.8%) showed improvement, and 6 (27.3%) had no effect.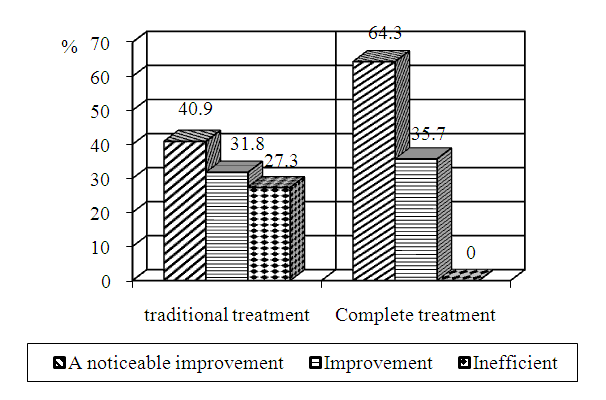 | Figure 8. Results of treatment of patients with nodular form of cutaneous leishmaniasis using complex and traditional therapy |
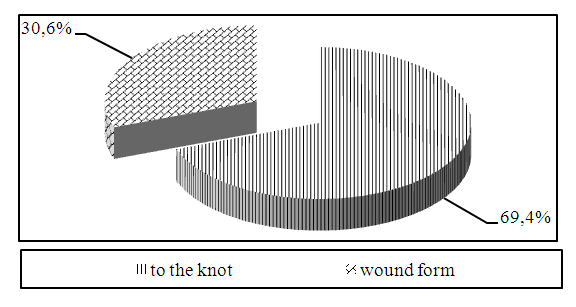
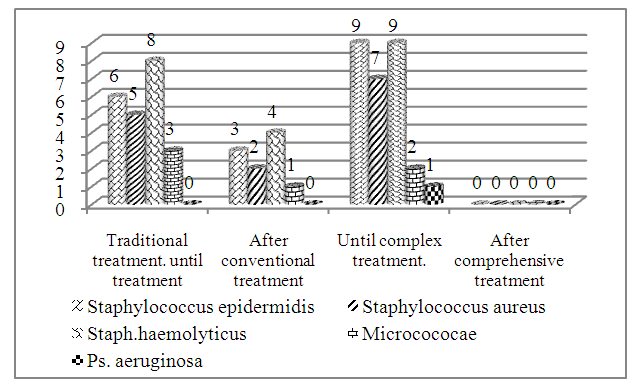
Among patients with ulcerative leishmaniomas (12 patients), significant improvement was noted in 6 (50.0%) patients after complex treatment, 5 (41.7%) patients improved, and 1 (8.3%) patient underwent treatment did not work. Among patients who received conventional treatment (10 patients), significant improvement was observed in 4 (40.0%), improvement in 3 (30.0%) and notreatment effect in 3 (30.0%) patients.Thus, clinical observations show that the complex method developed for the treatment of patients with cutaneous leishmaniasis has a positive therapeutic effect and can be recommended for the treatment of patients with this dermatosis.When studying the microflora of skin washes, it was found that in all studied clinical forms of cutaneous leishmaniasis, there is a combination of microflora that goes along with the main disease.Therefore, we were interested in studying the effect of the used treatment methods on the parameters of the skin microflora.The results of the study of the effect of traditional therapy on the detection of accompanying microflora in skin washes showed (Fig. 10) that during the study of cultures of skin washes before treatment in patients with the tubercular form of cutaneous leishmaniasis, Staphylococcus epidermidis - In 6 cases, Staphylococcus aureus – in 5 cases, Staph.haemolyticus – in 8 cases and Microcococae – in 3 cases were detected. After conventional treatment, Staphylococcus epidermidis was detected in skin washes in 3 cases, Staphylococcus aureus - in 2 cases, Staph.haemolyticus - in 4 cases, and Microcococae - in 1 case.In the treatment method developed for patients with tubercular form of cutaneous leishmaniasis, Staphylococcus epidermidis in 9 cases, Staphylococcus aureus in 7 cases, Staph.haemolyticus in 9 cases, Microcococae in 2 cases and Ps. aeruginosa - identified in 1 case. After the therapy, all detected microorganisms disappeared in the patients of this group, and the skin of the examined patients became clean (Fig. 9).A study of the effect of conventional therapy on the skin microflora in patients with ulcerative leishmanioma (Fig. 10) showed that, in 1 case of patients in this group, Staphylococcus epidermidis was found in the skin wash, in 6 cases Staphylococcus aureus, Staph.haemolyticus - In 2 cases, Staphylococcus epidermidis and Candida srr. addition - in 1 case. Determined. In the background of the therapy, Staphylococcus epidermidis and Candida spp. not identified, but in 3 cases Staphylococcus aureus and in 1 case Staph.haemolyticus was identified.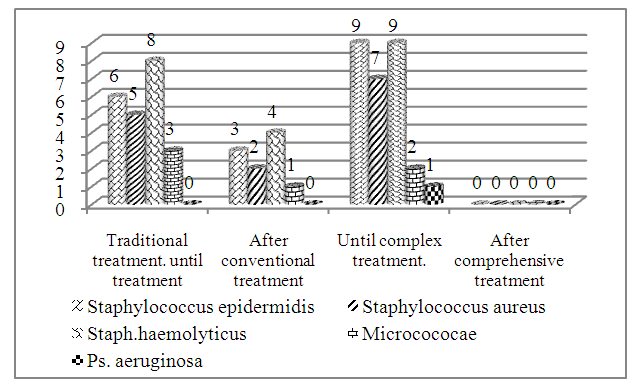 | Figure 9. Effect of therapy on skin microflora of patients with tuberous form of cutaneous leishmaniasis |
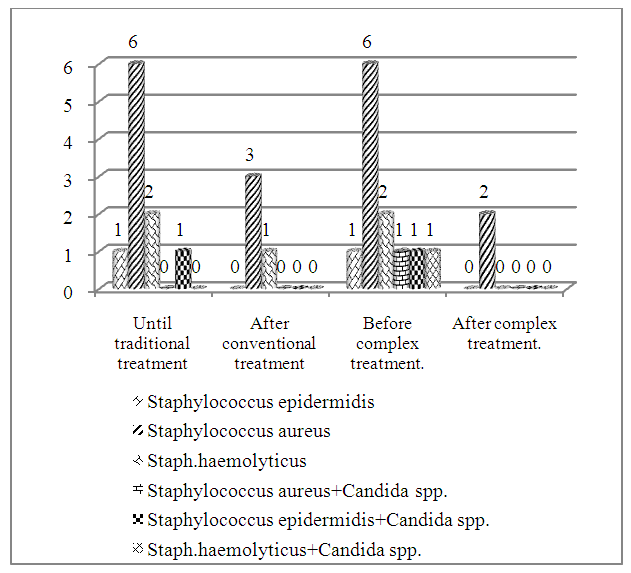
 | Figure 10. The effect of therapy on the microflora of the skin of patients with ulcerative leishmanioma (n) |
The study of the effect of the complex treatment method on indicators of skin microflora (Fig. 10) shows that, during the admission of patients in this group, skin washes showed Staphylococcus epidermidis in 1 case, Staphylococcus aureus in 6 cases, Staph.haemolyticus in 2 cases and Candida spp. with Staphylococcus aureus, Candida spp. with Staphylococcus epidermidis. and Staph.haemolyticus with Candida spp. - Found in 1 case. After treatment, Staphylococcus epidermidis, Staph.haemolyticus and Candida spp were found in skin washes. not detected, Staphylococcus aureus was detected only in 2 cases.
3. Conclusions
The obtained data show that in patients with cutaneous leishmaniasis, regardless of the clinical presentation of the disease, positive changes in the restoration of skin microflora occur after traditional therapy, but the skin is completely free of pathogenic microflora. no clearance was observed. On the contrary, the method developed by us for the treatment of cutaneous leishmaniasis in these groups of patients has a significant effect on cleaning the skin of pathogenic microflora, and this was clearly expressed in patients with the tubercular form of cutaneous leishmaniasis, and in these patients, the microorganisms detected in skin washes after treatment were completely eliminated. disappeared.Thus, the treatment method, developed for the treatment of patients with cutaneous leishmaniasis and including the local application of the drug "Baniocin" in the form of complex applications, has a positive therapeutic effect compared to the group of patients who received the traditional treatment method. "shows, promotes early regression of pathological symptoms, leads to early parasitological recovery and has a pronounced effect on cleansing the skin of pathogenic microflora.
References
| [1] | Abidova Z.M., Umurov F.F., Eshonkulov A.M. Leishmaniasis as a Treatment of Epedemiologic Diseases in the Bukhoro Region // Dermatology and Aesthetic Medicine. - 2017. - №2 (34). - P.100. |
| [2] | Andriyenko E.M., Matveeva E.L., Semenova S.E. Clinical Case of Leishmaniasis in the Practice of a Dermatovenerologist // Problems of Medical Mycology. - St. Petersburg, - 2013. - V.15. - №2. - P.54. |
| [3] | Control of Leishmaniasis // Report at a Meeting of the WHO Expert Committee on Control of Leishmaniasis, WHO Technical Report Series, No. 949, Geneva, March 22-26, 2010. –243 p. |
| [4] | Jalalova N.A. Modern ecological and epidemiological aspects of cutaneous leishmaniasis in Uzbekistan // Infection, immunity and pharmacology. – Tashkent, –2014. – Vol. 1. – №3. – P. 151-154. |
| [5] | Jalalova N.A. Epidemiological assessment of leishmaniasis incidence in Uzbekistan // Infection, immunity and pharmacology. – Tashkent, –2015. – №4. – P. 37-39. |
| [6] | Jalalova N.A., Kasymov I.A., Rakhmatov A.B. Epidemiological assessment of leishmaniasis incidence in Uzbekistan // Journal of theoretical and clinical medicine. – Tashkent, – 2014. – V.2. – №3. – P.32. |
| [7] | Ermak T.N. Leishmaniasis and HIV infection // Epidemiology and infectious diseases. – M., – 2015. – №1. – P.48-52. |
| [8] | Clinical aspects and immuno-cytokine profile of cutaneous leishmaniasis / Ikramova N.D., Abidova Z.M. et al. // Dermatovenereology and aesthetic medicine. – Tashkent, – 2015. – V.25. – №1. – P.45-50. |
| [9] | Cutaneous leishmaniasis: diagnostics, treatment, prevention / Sokolova T.V., Sanakoeva E.G., Gladko O.V., Gladko V.V. //Medical Bulletin of the Ministry of Internal Affairs. -2021. -No. 5 (114). -P. 25-29. |
| [10] | Koledaeva E.V., Maksimova E.D., Onuchina Yu.N. Retrospective analysis of methods for diagnosing and treating leishmaniasis from the beginning of the 20th century to the present // In the collection: Current issues in the history of medicine and health care in Russia, the Middle East and Africa. Collection of articles from the III scientific and practical conference with international participation. Kirov, -2023. -P. 18-22. |
| [11] | Muzhekhoev A.A., Shadieva Ya.M., Dzarmotova Z.I. Methods for treating and diagnosing cutaneous leishmaniasis // Achievements of science and education. -2022. -No. 5 (85). -P. 101-103. |
| [12] | Experience of using AmBisome in the treatment of patients with visceral leishmaniasis / Kovalenko D.A., Abdullaev O.U., Narzieva G.D., Saifiyev F.A. // Infection, immunity and pharmacology. - Tashkent, -2014. - T.1. - No. 3. - P. 247-249. |
| [13] | Rakhmatov A.B., Khikmatov R.S. Innovative technology of external therapy of cutaneous leishmaniasis. - Collection of abstracts of the International scientific and practical conference "Actual problems of dermatovenereology and aesthetic medicine" (Tashkent, September 10-11, 2021). // Dermatovenereology and aesthetic medicine. -2021. - No. 3. - P. 48. |
| [14] | Sabirov U.Yu., Khikmatov R.S. Complex therapy of patients with cutaneous leishmaniasis. - Collection of abstracts of the International scientific and practical conference "Actual problems of dermatovenereology and aesthetic medicine" (Tashkent, September 10-11, 2021). // Dermatovenereology and aesthetic medicine. - 2021. - No. 3. - P. 57-58. |
| [15] | Usarov G.Kh., Khalikov K.M., Sattarova H.G. Changes in the species composition of mosquitoes - carriers of leishmaniasis in Uzbekistan over the past 50 years. - Collection of articles of the International scientific and practical conference "Actual problems of biology and parasitology" (Samarkand, June 2-3, 2023). // Problems of biology and medicine. - 2023. - No. 3.1. – P.415-416. |
| [16] | Khaitov K.N., Abidov H.A., Abidov A.M. Systemic enzyme therapy in the treatment of cutaneous leishmaniasis. – Abstracts of the international scientific and practical conference "Actual problems of dermatovenereology and aesthetic medicine" (Tashkent, September 11, 2020). // Dermatovenereology and aesthetic medicine. – 2020. – №3. – P.78. |
| [17] | Eshboev E.Kh., Nematov A.S., Mustanov Zh.A. Uzbek State University of Culture - Etiology, Epidemiology, and Prevention. –Collection of abstracts of the International scientific and practical conference "Actual problems of dermatovenereology and aesthetic medicine" (Tashkent, September 10-11, 2021). // Dermatovenereology and aesthetic medicine. -2021. -No. 3. -P.70-71. |
| [18] | A historical review of the role of cytokines involved in leishmaniasis /Mirzaei A., Maleki M., Masoumi E., Maspi N. // Cytokine. –2021. –V.145. –P.155297. |
| [19] | Akbari M., Oryan A., Hatam G. Immunotherapy in treatment of leishmaniasis //Immunol. Lett. –2021. –V.233. –P.80-86. |
| [20] | Azeredo-Coutinho R.B., Matos D.C., Armba G.G. Contrasting human cytokine responses to promastigote whole-cell extract and the Leishmania analogue receptor for activated C kinase antigen of L.amazonensis in natural infection versus immunization // Clin. Exp. Immunol. –2008. –V.153. –P.369-375. |
| [21] | Cabrera-Serra M.G., Valladares B., Pinero J.E. In vivo activity of perifosine against Leishmania amazonensis //Acta Trop. –2008. –V.12. –P.109-112. |
| [22] | Detection of Leishmania infantum cryptic infection in asymptomatic blood donors living in an endemic area (Eivissa, Balearic Islands, Spain) by different diagnostic methods /Riera C., Fisa R., Udina M. et al. //Trans. R. Soc. Trop. Med. Hyg. –2004. –V.98. –№2. –P.102-110. |
| [23] | Dogra J.A double-blind study on the efficacy of oral dapsone in cutaneous leishmaniasis //Trans. R. Soc. Trop. Med. Hyg. –1991. –V.85. –P.212-215. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML