-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(8): 2070-2073
doi:10.5923/j.ajmms.20241408.26
Received: Aug. 2, 2024; Accepted: Aug. 18, 2024; Published: Aug. 22, 2024

Outcomes of Perinatal Pathology in Newborn from Mothers with Early Pre-Eclampsia
Abduraim Shamshievich Arzikulov1, Yulduz Gulyamovna Rasul-Zade2, Dilnoza Abduraimovna Melieva1, Abdikadir Gulyamovich Arzibekov1
1Andijan State Medical Institute, Andijan, Uzbekistan
2Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Preeclampsia (PE) is a leading cause of maternal and perinatal morbidity and mortality. PE can be divided into early-onset PE, which requires delivery before 34 weeks' pregnancy, and late-onset PE, which occurs during or after 34 weeks, the former being associated with a higher incidence of adverse outcomes.Purpose of the research:to study the health status of newborns born to mothers with early preeclampsia. Materials and methods:the work was performed at the clinical base of the maternity complex No. 1 in Andijan, Republic of Uzbekistan. We performed an analysis of the birth history of pregnant women with preeclampsia and their newborns (n=112 couples) for the period 2018-2022, including those with early (n=41) and late onset of PE (n=71), data assessing the condition of newborns on the Apgar scale immediately after birth, assessment of the degree of maturity of newborns (prematurity, hypoxic damage to the central nervous system), the incidence of stillbirth. The work used anamnestic, general clinical, obstetric-gynecological, instrumental-functional and laboratory research methods. Results and discussion: Hypoxic damage to the central nervous system (82.9%), malnutrition (19.5%) and extreme prematurity (4.8%), perinatal mortality (4.8%) are significantly more often diagnosed. With the early PE development, during pregnancy up to 33 weeks + 6 days, the structure of perinatal pathology becomes more severe and aggressive. Conclusion:One of the reserves for reducing perinatal complications is identifying pregnant women at high risk of developing PE and perfoming targeted, effective preventive measures, especially during its early development.
Keywords: Early preeclampsia, Perinatal pathology, Hypoxic damage to the central nervous system
Cite this paper: Abduraim Shamshievich Arzikulov, Yulduz Gulyamovna Rasul-Zade, Dilnoza Abduraimovna Melieva, Abdikadir Gulyamovich Arzibekov, Outcomes of Perinatal Pathology in Newborn from Mothers with Early Pre-Eclampsia, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 2070-2073. doi: 10.5923/j.ajmms.20241408.26.
1. Introduction
- Preeclampsia (PE) as a complication of pregnancy, with its consequences threatens not only the pregnant woman, but also the normal course of fetal development. This fact is indicated by numerous research works by scientists in our country and abroad [1,2,3,4,5,6,7,8,9]. The early development of preeclampsia in pregnant women is especially dangerous for the development of the fetus [9]. In the specialized literature there are isolated reports on the consequences of early development of preeclampsia on the health status of the newborn [8,9]. Disorders of the uteroplacental circulation, which, being a pathophysiological manifestation of preeclampsia, lead to the development of hypoxic damage to the central nervous system and, ultimately, to a holistic metabolic disorder of the developing fetus [6]. In newborns from mothers with early preeclampsia, there is a high proportion of perinatal complications of hypoxic damage to the central nervous system, the birth of an immature child with different degrees of prematurity, and cases of stillbirth [7,8,9]. One of the reserves for reducing perinatal complications is identifying pregnant women at high risk of developing preeclampsia and performing targeted, effective preventive measures, especially during its early development. The relevance of the work performed lies in the fact that the frequency of development of severe PE and eclampsia in the city. Andijan has a clear upward trend in this indicator. The incidence of pregnant women with PE and eclampsia during pregnancy in the city. Andijan for the analyzed period is significantly higher than in the whole Republic (7.3% versus 4.0%, (p <0.05)). In general, in the region there is no clear trend towards a decrease in the frequency of PE, especially its severe forms; on the contrary, a moderate increase can be observed [2,4].Thus, the above convincingly indicate the relevance of studying the health status of newborns born to mothers with the early development of preeclampsia in the region.
2. Materials and Methods
- The work was performed at the clinical base of the maternity complex No. 1 in Andijan. All examined patients and their newborns were divided into the following groups: 1) patients with normal pregnancy without clinical and laboratory signs of PE and their newborn infants (n=297); 2) a group of patients with early-onset PE (EOPE) (up to 34 weeks) and their infants (n=41); and 3) newborns born to mothers with late-onset PE (LOPE) (after 34 weeks) (n=71).Women with normal pregnancies were defined as those without a medical, obstetric, or surgical complication during pregnancy, appropriate for gestational age, at term (≥37 weeks' gestation) (1, 5) and without a neonatal complication.Preeclampsia was defined as the onset of hypertension (systolic blood pressure ≥140 mmHg and /or diastolic blood pressure ≥90 mmHg on at least two occasions, 4 hours to 1 week apart) after 20 weeks of pregnancy with proteinuria (≥300 mg per day) in urine collection or at least one dipstick measurement ≥2 +) (1).Newborns born to women with multiple pregnancies, fetuses with chromosomal and/or congenital abnormalities, and newborns born to women with HELLP syndrome or who developed preeclampsia after delivery were excluded.Collecting blood and its use for research purposes were approved by the ethical commission at the Andijan State Medical Institute.An analysis of perinatal outcomes and the structure of perinatal pathology in newborns from mothers in two studied groups of pregnant women was performed in a comparative aspect: a group of newborns born from mothers without PE (screening negative pregnant women with PE n=247%) and in a group of newborns born from pregnant women at risk for PE (screening positive pregnant women with PE n = 162%), including those with early (n=41) and late onset PE (n=71), assessment of the condition of newborns using the Apgar scale immediately after birth, assessment of the degree of prematurity and hypoxic damage to the central nervous system (CNS) using A.V. Volodin’s criteria (2005), the incidence of stillbirths.The severity of perinatal CNS lesions in newborns was assessed according to the accepted classification of the Russian Association of Perinatal Medicine Specialists (2000): for a mild degree (cerebral ischemia of grade I) severity, symptoms of depression/excitation were characteristic for no more than 5-7 days. The group of moderate severity (cerebral ischemia grade II) included newborns with characteristic syndromes of central nervous system depression and/or excitation (more than 7 days), the appearance of seizures, signs of intracranial hypertension and autonomic-visceral disorders. In newborns with severe hypoxia (cerebral ischemia grade III), clinical symptoms of severe depression syndrome were detected, infant agitation for more than 10 days, convulsive syndrome (possible convulsive epistatus), decerebration, dysfunction of the stem parts of the central nervous system, decortication, autonomic-visceral disorders, symptoms progressive intracranial hypertension.Statistical analysis of the data was performed using generally accepted methods of variation statistics on a personal computer using the Microsoft applied statistics software package Excel 2010, Statistica 6.1., SigmaPlot, Medcalc (9.1.0.1). The arithmetic mean (M), the error of the mean (x), and the standard deviation (a) were calculated. Statistical processing methods were used depending on the type of random variables and the research problem. The level of statistical significance when testing the null hypothesis was taken at the corresponding p <0.05.The work used anamnestic, general clinical, obstetric-gynecological, instrumental-functional and laboratory research methods.
3. Results and Its Discussion
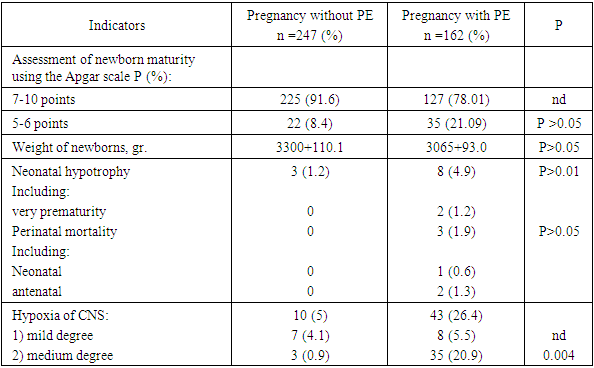
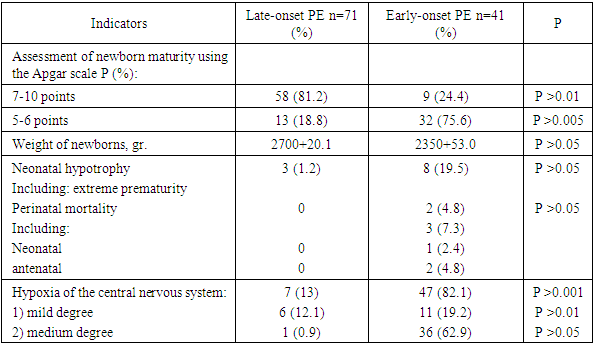
- The results of a study of the perinatal pathology structure in newborns from mothers of the compared subgroups (Table 1) indicate that low indicators of the maturity of the newborn’s body according to the Apgar assessment method and the correlative connections with it of an increase in indicators of hypoxic damage to the central nervous system of moderate severity were diagnosed reliably often in infants of the examined cohort of pregnant patients with screening (+) PE (n = 162, 20.9%; P >0.005), low assessment of newborn maturity (n = 35, 21.09). In the same group, a high incidence of malnutrition was noted (n = 8, 4.9%), including those with a weight less than 1500 - extreme prematurity (n = 2, 1.2%) and perinatal mortality (n = 3, 1.9%).
|
|
4. Conclusions
- In newborns from mothers with early preeclampsia, there is a significantly high proportion of perinatal complications in the form of hypoxic damage to the central nervous system (P >0.2), the birth of an immature child with different degrees of prematurity and extremely low prematurity (P>0.005), cases of stillbirth (P>0.001). In the study group of newborns, birth weight was lower than in the control group (p < 0.001). Most births in the group of newborns born to mothers with preeclampsia are performed by cesarean section.One of the reserves for reducing perinatal complications is identifying pregnant women at high risk of developing preeclampsia and performing targeted, effective preventive measures, especially during its early development.Until now, the main problem of modern obstetrics is the early detection of pregnancies with a high degree of risk of early-onset PE and the adoption of the necessary preventive measures to improve placentation and reduce the incidence of perinatal complications. Mastrolia Salvatore Andrea et al. [13] in their research conclude that, despite some success in reducing the incidence of early PE, overall, trends in improving maternal and perinatal outcomes in women with pregnancies complicated by PE remain insignificant. Another reserve for reducing perinatal complications in patients with early PE, in our opinion, is the organization of personalized PE prevention, identifying women of childbearing age with high-risk indicators. Pregestational care can be especially useful for women who have risks of developing PE (demographic, anamnestic, somatic, psycho-social) to avoid spontaneous pregnancy. Targeted support for these women before conception can make a useful contribution to reducing the incidence of early-onset and severe PE. New cohort studies with a representative sample are required to evaluate the effectiveness of targeted pregestational care to reduce the incidence of PE and perinatal complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML