Utaev Latif Kholmamatovich1, Dusiyarov Muhammad Mukumbayevich2, Askarov Pulat Azadovich2, Khujabaev Safarboy Tukhtabayevich2
1Navoiy Branch of the Republican Emergency Medical Care, Uzbekistan
2Samarkand State Medical University, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The study used retrospective and prospective data of 242 patients who had surgeries for incarcerated hernias of the anterior abdominal wall complicated by intestinal obstruction. Regardless of the type and size of incarcerated ventral hernias, high intra-abdominal pressure (IAP) with the risk of enteral and multiple organ failure is an indication for the use of tension-free methods of plastic surgery. SPK can be prevented by enteral intubation. In the main study group, a significant (p<0.05) tendency to decrease IAP as a result of tension-free plastic surgery and enteral intubation was found. In the comparison group, the initial value of 19.3±1.6 decreased to 17.1±1.3 after surgery, and in the main group, the initial value of 18.8±1.8 decreased to 14.5±1.3 mm Hg. Resolution of intestinal paresis and obstruction can be effectively monitored using abdominal ultrasound.
Keywords:
Strangulated ventral hernias, Intestinal obstruction
Cite this paper: Utaev Latif Kholmamatovich, Dusiyarov Muhammad Mukumbayevich, Askarov Pulat Azadovich, Khujabaev Safarboy Tukhtabayevich, Clinical Features of Intracted Ventral Hernias Complicated by Intestinal Obstruction, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 2000-2003. doi: 10.5923/j.ajmms.20241408.12.
1. Introduction
Treatment of strangulated hernias of the anterior abdominal wall is one of the important areas of emergency surgery, which receives much attention in research and publications. These hernias complicate the course of the disease in 10-17% of patients with hernias and rank second among acute surgical diseases of the abdominal organs after acute appendicitis. However, mortality from strangulated hernias is 15-16 times higher than from acute appendicitis. Statistics from leading research and medical institutions show that, despite achievements, surgical treatment of patients with strangulated abdominal wall hernias gives unsatisfactory results. Postoperative complications reach 50%, and mortality ranges from 2 to 4 percent. This is due to the high frequency of strangulation of intestinal loops, leading to strangulation intestinal obstruction (more than 70%), as well as a large number of elderly patients (about 40%).
2. Materials and Methods
Incorrect choice of the method of plastic surgery, significant tension of the abdominal wall tissues, decrease in the volume of the abdominal cavity and development of abdominal compartment syndrome in 0.8-12% of operated patients are the main reasons for unsatisfactory results of the operation. Purpose of the study. Development of a strategy for diagnosis and operations for strangulated ventral hernias complicated by intestinal obstruction, including the choice of the method of hernioalloplasty. Materials and methods. The work is based on the results of a retrospective and prospective study of 242 patients operated on for strangulated hernias of the anterior abdominal wall of various localizations complicated by the development of intestinal obstruction, who were in patients at the Navoi branch of the RNCEM in 2018- 2023. Patients were subjected to clinical observation, who were divided into two groups depending on the nature and scope of the surgical intervention. The main group consisted of 136 patients with strangulated hernias of the anterior abdominal wall complicated by intestinal obstruction, who underwent surgery using synthetic implants (the method of "tension-free" hernioplasty). This group included patients with different localizations of hernias: 46 (33.8%) with strangulated inguinal hernias, 38 (27.9%) with strangulated umbilical hernias and 52 (38.2%) with strangulated postoperative ventral hernias.The control group included 106 patients with strangulated hernias of the anterior abdominal wall complicated by intestinal obstruction, who underwent traditional autoplasty operations ("tension" hernioplasty). This group also consisted of patients with different localizations of hernias: 30 (28.3%) with strangulated inguinal hernias, 34 (32.1%) with strangulated umbilical hernias and 42 (39.6%) with strangulated postoperative ventral hernias. In the main group, the average age of patients was 56.4 years (plus or minus four years), with an age range from 28 to 81 years. Among them, there were 74 women (54.4%) and 62 men (45.6%). In the control group, the average age of patients was 57.6 (plus or minus 3.1) years, and the age range was from 27 to 78 years. There were 50 men (47.2%) and 56 women (52.8%).
3. Result Discussion
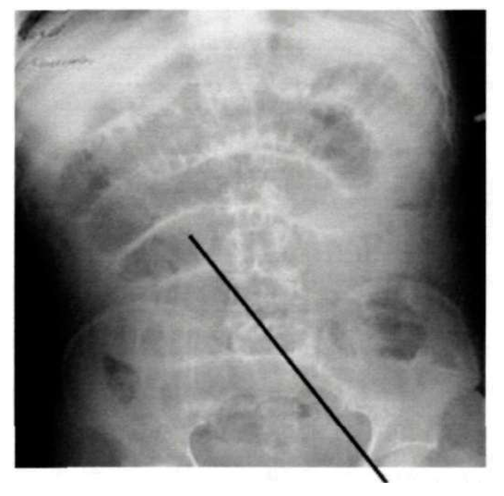
Most of the surgical patients in the older age group had serious comorbidities that affected the course and outcome of the disease. 82% of people in this age group had 2-3 comorbidities. According to the anamnesis, the duration of wearing a hernia before admission to the hospital varied from 1 to 20 years, with a total duration of 9.5 + 1.7 years.From the onset of strangulation, patients admitted to the emergency department of the Samarkand branch of the RRCEM had different periods. The hospitalization time in the main group ranged from 4 to 144 hours, with a total duration of 27.1 plus or minus 8.4 hours. Six patients (8.8%) were admitted within the first six hours; 46 (33.8%) were admitted between six and twelve hours; 38 (27.9%) were admitted between twelve and twenty-four hours; and 20 (29.4%) patients were admitted after strangulation after 24 hours.The hospitalization time in the control group ranged from 3 to 144 hours, with a mean stay of 22.6 plus or minus 6.8 hours. Six patients (11.3%) were admitted within the first six hours; 42 (39.6%) were admitted between six and twenty-two hours; 30 (28.3%) were admitted between twenty-two and twenty-four hours; and 22 (20.8%) were admitted after 24 hours from strangulation.238 (98.3%) patients reported that their previously freely reducible hernia could not be treated. They also reported that the hernia was becoming more painful and increasing in size. In 230 patients (95.1%), no "cough impulse" was observed during palpation. Nausea was observed in 136 (55%) patients, vomiting, which recurred at the prehospital stage and periodically recurred in 92 (37%) patients, delayed passage of stool and flatus in 64 (26%) patients, and increased peristalsis in 34 (14%) patients. 28 (11%) patients showed peritoneal symptoms, and 10 (4%) patients noted a change in skin color over the hernial protrusion.Radiographic examination was performed in 188 (75%) patients admitted to the hospital who had an incarcerated hernia of the anterior abdominal wall, which was complicated by intestinal obstruction. Abdominal radiographs showed that 53.1% of patients had evidence of low small bowel obstruction with multiple horizontal fluid levels in dilated small bowel loops. 26.6% of patients had evidence of high small bowel obstruction on radiographs.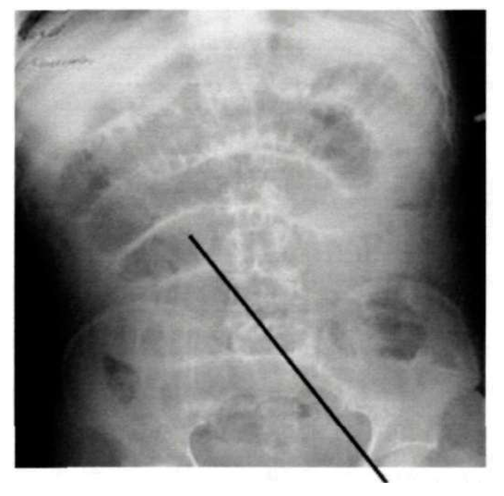 | Picture 1. Patient D., 51 years old. X-ray image of strangulated inguinal hernia with signs of small bowel obstruction (direct projection) |
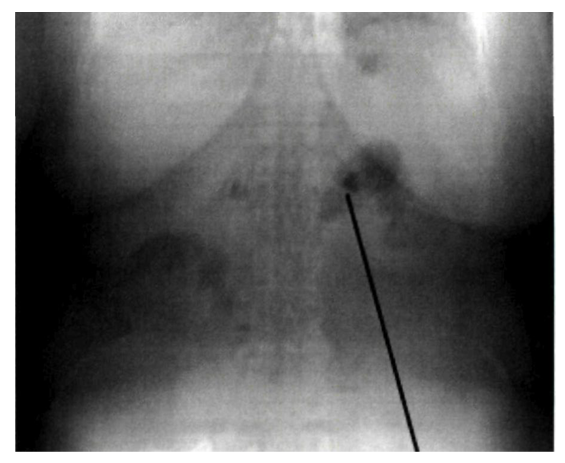
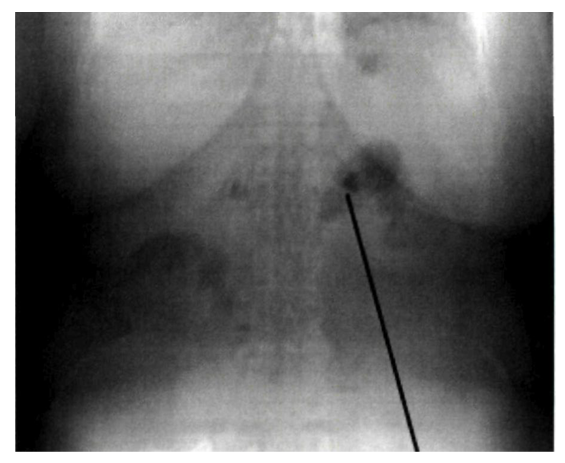 | Picture 2. Patient A., 63 years old. Postoperative ventral hernia with radiographic signs of intestinal obstruction (direct projection) |
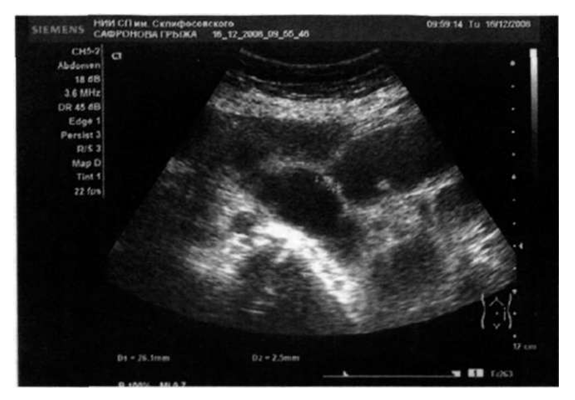
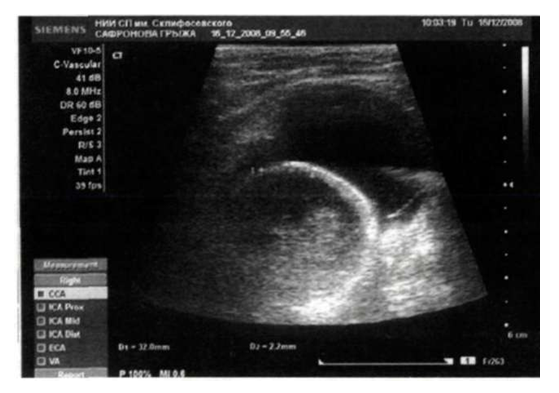
In the hospital, an ultrasound examination was performed in 166 patients with complicated strangulated hernias (68.8%). In 92 (92%) patients of the main group and 68 (94%) of the control group, an increase in the diameter of the afferent intestinal segment with thickening of the walls, as well as "pendulum-like" movements of the intestinal contents and collapsed intestinal loops of the efferent segment were detected. The appearance of signs of free fluid in the lateral channels and interloop spaces was accompanied by a number of complications. 52 (52%) patients of the main group and 42 (58%) patients of the control group showed ultrasound signs characteristic of strangulated hernias complicated by peritonitis and intestinal necrosis. In 48 (35.2%) cases of the main group and 42 (39.6%) cases of the control group, the contents of the hernial protrusion were detected as a strangulated intestinal loop (Picture 3, 4). In 36 (36%) and 30 (42%) cases, respectively. In 36 (36%) cases of the main group and 30 (42%) of the control group, small intestinal loops and omentum were detected. In 34 (34%) patients of the main group and 32 (44%) of the control group, a hernia was detected.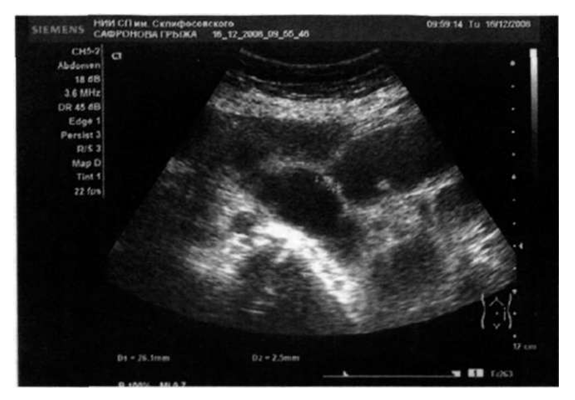 | Picture 3. Patient R., 52 years old. Ultrasound: strangulated ventral hernia: the hernial orifice is located, through which a fragment of the small intestine with liquid contents comes out, without peristalsis. Blood flow in the wall is not registered. Fluid in the hernial sac is located |
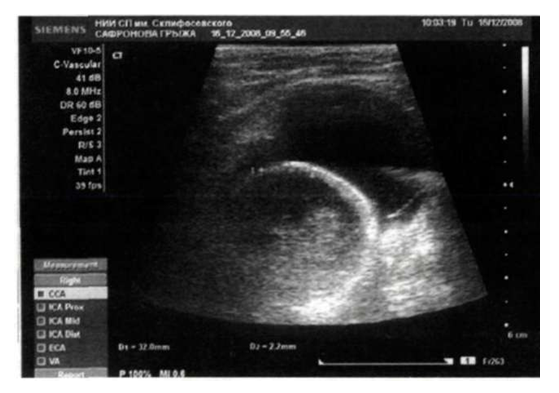 | Picture 4. Patient J., 71 years old. Ultrasound: Strangulated right-sided inguinal hernia: In the right inguinal region, a hernial orifice up to 1.5 cm is located, into which a fragment of the small intestine with a diameter of 3.2 cm emerges, the wall is 0.3-0.4 cm, blood flow in the wall and peristalsis are not recorded, the contents are liquid in nature. Heterogeneous hernial fluid is located |
In both groups of patients with strangulated hernias complicated by intestinal obstruction, 92 (36.3%) patients had serious systemic diseases that posed a significant risk for the anesthetic procedure. Multicomponent endotracheal anesthesia was used for the majority of operations (208, or 85.9%). The operation was performed under spinal anesthesia in 20 patients with strangulated inguinal hernias (8.2%). The operation was performed under local infiltration anesthesia using 0.5% Novocaine solution with intravenous potentiation in fourteen patients (5.6%) who were considered high risk according to the ASA classification. In the main group of patients with strangulated hernias, 62 patients (42%) had isolated strangulation of the small intestine, 46 (36%), strangulation of the small intestine with omentum in 18 (14%), and strangulation of the colon in 10 (8%). In the control group, strangulation of the small intestine was also frequently observed in 42 patients (45.3%), strangulation of the small intestine and omentum in 36 (29.3%), strangulation of the small intestine and colon in 18 (16.7%), and strangulation of the colon in 10 (9.4%) patients. In the main group, there were 18 cases of nonviable omentum and small intestine, 28 cases of necrotic portion of the small intestine, and 2 cases of the colon. In the control group, ten patients received resections of necrotic omentum and small bowel, twenty-six of them received small bowel resections, and two patients received colon resections. A total of 86 patients (35.5%) underwent bowel resection due to strangulation and necrosis. Eighty-two patients had small bowel resections, and four had colon resections.In the control group, traditional methods of plastic surgery for the surgical treatment of strangulated hernias were used without the use of synthetic implants. Treatment of strangulated inguinal hernias included the Bassini (12 cases) and Postemsky (18 cases) methods, as well as the Mayo (38 cases) and Sapezhko (62 cases) methods for the treatment of POVG and strangulated umbilical hernias. In six cases with giant ventral hernias, decompressive surgery was performed to eliminate the wound.Results and discussion. In the group of patients who underwent surgical treatment of strangulated hernias, various methods of "tension-free" plastic surgery of the anterior abdominal wall were mainly used. These methods have been well proven in previous operations for the treatment of hernias and have been well tested. A study examining the effect of intra-abdominal pressure levels was conducted in 60 patients who underwent surgery for strangulated postoperative ventral hernia complicated by intestinal obstruction. Of these, 32 patients were studied in the study group, where "tension-free" hernioplasty was performed, and 28 patients in the control group, where "tension" hernioplasty was performed. Of the 60 patients studied, 52 (86.7%) had grade II or III intra-abdominal pressure. In the study group, the initial levels of intra-abdominal pressure were 18.8±1.8 mm Hg, while in the control group they were slightly higher, amounting to 19.3±1.6 mm Hg (p>0.05). In patients of the main group, by the end of the operation, there was a clear decrease in the level of intra-abdominal pressure (p<0.05) as a result of decompression of the gastrointestinal tract and the use of "tension-free" plastic surgery. In the control group, the average intra-abdominal pressure was lower (17.1 ±1.3 mm Hg). In both groups of patients, an increase in intra-abdominal pressure was observed up to three days after the operation. On the first day after the operation, the intra-abdominal pressure in the main group was 15.6 ±1.5 mm Hg, and in the control group 17.8 ±1.1 mm Hg. On the second day after the operation, the average intra-abdominal pressure in the main group was 15.9 ±0.8 mm Hg, and in the control group 18.3 ±0.7 mm Hg. On the third day, the average intra-abdominal pressure in the main group was 16.2 ± 0.7 mm Hg, and in the control group 18.9 ± 0.7 mm Hg. On the fourth day, the level of intra-abdominal pressure in the main group decreased to 13.3 ± 0.8 mm Hg and to 16.9 ± 0.7 mm Hg in the control group.The Pearson correlation coefficient (r=0.85 at p<0.05) confirmed the positive correlation between the initial level of intra-abdominal pressure (IAP) and the volume of fluid removed through the external enteral tube (EET) during surgery. The reduction in the IAP level after surgery was possible due to the use of EET. With statistically significant differences, an increase in IAP was observed up to three days during the four days after surgery (p<0.05). In addition, by the third day, the volume of intestinal discharge through EET increased. However, the difference in the volume of fluid evacuated after surgery was not statistically significant. Thus, the use of EET reduces the level of IAP by removing intestinal contents. Results of early postoperative abdominal ultrasound examinations in 28 patients out of 250 patients undergoing surgery for strangulated hernias complicated by intestinal obstruction were analyzed to assess the reversal of small bowel obstruction in the postoperative period. Of the total 28 patients undergoing surgery, 24 ultrasound examinations were performed. Of the 20 examinations performed from the 2nd to the 5th day after surgery, 18 showed the use of nasoenteric intubation of the small bowel. Gas in small bowel loops was detected in all 28 patients within 2–10 days after surgery. Of the 28 patients analyzed on the second and third days after surgery, four had gas and fluid collections in the lumen of multiple small bowel loops. Changes such as dilation of the small bowel lumen to 4.0–5.0 cm, moderate thickening of the walls and folds, and the formation of multiple horizontal fluid levels and a small amount of gas in the right parts of the colon were observed. Patients with severe symptoms of intestinal obstruction before surgery had these changes and had a long period of obstruction (10–34). The next dynamic control showed that the amount of gas in the small bowel loops decreased, that the horizontal fluid levels decreased, that the edema of the walls and folds decreased, and that gas appeared in the colon overall. In 24 patients, changes in the small bowel included gas in individual loops (22 of 24 cases), which formed either isolated collections (8 cases) or single loops with gas with a diameter of 1.5 to 3 cm (14 cases). In five patients, there were no horizontal fluid levels, and in nine patients, there were unclear fluid levels in the lumen. Thickening of the mucosal folds in single loops of small bowel was detected on the fourth postoperative day in a patient with a bowel obstruction that had lasted more than four days and was the result of a ventral hernia. All patients had a moderate amount of gas in the colon throughout its length.Among eight patients who underwent surgery for strangulated hernias of the anterior abdominal wall complicated by intestinal obstruction, the overall mortality rate was 3.3%. The mortality rate after surgery in the control group was 5.7% (6 patients), while in the main group it was 1.5% (2 patients). In the control group, the cause of death was pulmonary embolism in two cases, and in the remaining four cases, the cause of death was acute cardiorespiratory failure caused by mechanical ventilation and bilateral pneumonia caused by increased intra-abdominal pressure. In the main group, both people died due to acute myocardial infarction. Five of the eight deaths occurred in patients over seventy years old with strangulation lasting more than one day.
4. Conclusions
1. In strangulated ventral hernias of any type and size, the use of tension-free methods of plastic surgery is indicated due to increased intra-abdominal pressure, which can lead to enteral and multiple organ failure. Intestinal failure syndrome can be prevented with endotracheal intubation.2. In the main study group, there was a significant tendency to decrease IAP (p<0.05) when using NEI and tension-free plastic surgery. In the comparison group, IAP dropped from the initial value of 19.3 ± 1.6 to 17.1 ± 1.3 mm Hg after surgery, while in the main group it dropped from 18.8 ± 1.8 to 14.5 ± 1.3 mm Hg with a similar trend over the next three days. Ultrasound examination of the abdominal cavity can effectively monitor the resolution of paresis and intestinal obstruction. 3. An algorithm for treating patients with strangulated hernias complicated by intestinal obstruction, taking into account the degree of enteral insufficiency, the level of IAP, the type and size of hernias, can reduce the incidence of abdominal complications from 20.7% to 4.4%, general postoperative complications from 28.3% to 11.3%, mortality from 5.2% to 1.5% and the incidence of wound complications from 28.3% to 8.8%.
References
| [1] | Sallinen, V., et al. (2022). "Management of incarcerated hernia and the impact on clinical outcomes." *BMC Surgery*. DOI: 10.1186/s12893-022-01321-3. |
| [2] | Henriksen, N.A., et al. (2021). "Incarcerated ventral hernia: Pathophysiology, diagnosis, and treatment." *British Journal of Surgery*, 107(3), 171-182. DOI: 10.1093/bjs/znaa104. |
| [3] | Skrovina, M., et al. (2020). "Clinical outcomes of ventral hernia repair in emergency settings." *World Journal of Emergency Surgery*, 15(1), 45. DOI: 10.1186/s13017-020-00320-9. |
| [4] | Velasco, N., et al. (2019). "Predictive factors for bowel necrosis in patients with incarcerated hernias." *BMC Medical Informatics and Decision Making*, 19(1), 158. DOI: 10.1186/s12911-019-0873-2. |
| [5] | Rios-Diaz, A.J., et al. (2023). "Umbilical hernia repair and risk of recurrence in complex cases." *BMC Surgery*. DOI: 10.1186/s12893-023-02001-0. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML