-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(8): 1977-1980
doi:10.5923/j.ajmms.20241408.06
Received: Jul. 10, 2024; Accepted: Aug. 2, 2024; Published: Aug. 6, 2024

Assessment of the Working Environment of a Specialized Hospital for the Treatment of COVID-19
Bakhriddin Nurmatov1, Bakhodir Rakhimov2, Sardor Fayziboev3
1Researcher, Assistant, Tashkent Medical Academy, Uzbekistan
2Dsc., Assistant Professor, Tashkent Medical Academy, Uzbekistan
3Master’s Student, Tashkent Medical Academy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of this study is to examine the working conditions of medical personnel responsible for treating and caring for COVID-19 patients and, subsequently, to propose measures to safeguard their health. The survey encompassed 75 hospital employees specializing in COVID-19 treatment, representing at least 15% of the total staff. Through this survey, the medical staff identified high-risk scenarios for contracting the disease and developed strategies to mitigate these risks and protect their health.
Keywords: COVID-19, Labor process, Working conditions, Workers’ health, Questionnaires
Cite this paper: Bakhriddin Nurmatov, Bakhodir Rakhimov, Sardor Fayziboev, Assessment of the Working Environment of a Specialized Hospital for the Treatment of COVID-19, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 1977-1980. doi: 10.5923/j.ajmms.20241408.06.
Article Outline
1. Introduction
- According to the guide “Guidance on Preparing Workplaces for COVID-19” [1,2,5] developed by the United States Occupational Safety and Health Administration (OSHA), the classification of the effects of SARS-CoV-2 on workers was developed and divided into very high, high, medium, and low levels. The highest level of this classification includes doctors, nurses, dentists, paramedics, emergency medicine doctors, laboratory workers, and specialists in pathological anatomy. According to scientific and research works, medical workers who worked during the pandemic were in the 3rd class of harmful and dangerous factors of the working environment, with a rating of not less than 3.3 [4]. Another study described the negative impact of the COVID-19 pandemic on the mental well-being of medical workers, resulting in depression, anxiety, and stress. It concluded that the COVID-19 pandemic significantly contributed to depression, anxiety, and stress among medical workers [2,3].
2. Research Objective
- The main aim of this research work is to study the working conditions of medical workers who treat and care for patients infected with COVID-19.
3. Object and Subject of the Research
- The research work was carried out at Zangiota No. 2 hospital, a medical institution specializing in the treatment of patients infected with COVID-19 in the city of Tashkent. The study involved a sanitary-hygienic assessment of treatment conditions within the hospital, focusing on key areas such as reception, wards, intensive care units, and sorting areas.
4. The Main Section
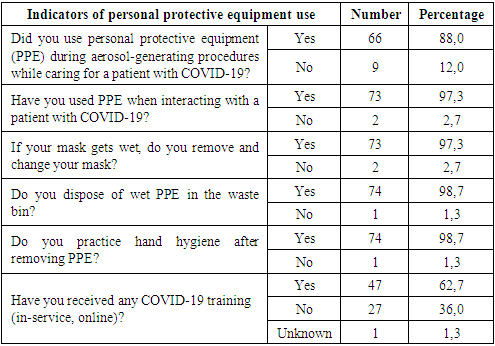
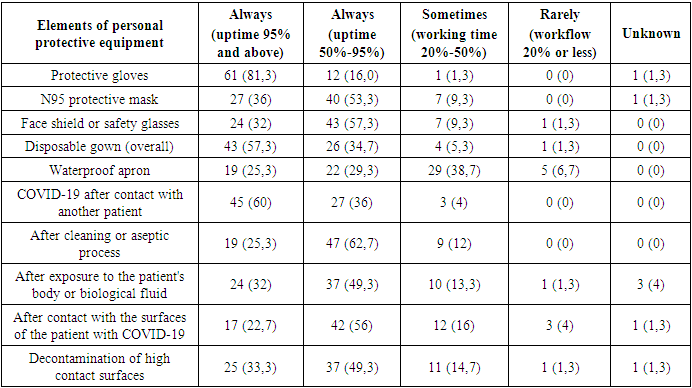
- Anonymous questionnaires were used to study and evaluate the health of employees during the investigation of indoor air and surface contamination in the hospital specializing in the treatment of COVID-19. These questionnaires also aimed to assess the hygienic factors of the hospital's indoor air. At least 15% of the total number of employees participated in the surveys, totaling 75 employees.According to questionnaire, 34 (43.5%) men and 41 (54.7%) women participated in the survey. In terms of age groups, 14 (18.7%) were aged 18-24, 37 (49.3%) were aged 25-34, 22 (29.3%) were aged 35-44, and 2 (2.7%) were aged 45-54. Regarding marital status, 14 (18.7%) were unmarried, 60 (80%) were married, and 1 (1.3%) was divorced. It was found that 39 (52%) of the respondents have a higher education and 36 (48%) have secondary education. In terms of length of service, 51 (68%) have 1-10 years of experience, 22 (29.3%) have 11-20 years, and 2 (2.7%) have 21 or more years. Regarding job types of medical workers, 37 (49.3%) are treating doctors, 12 (16%) are nurses, 3 (4%) are receptionists (support staff), 9 (12%) are laboratory workers, and 2 are other staff (including roles in activities such as X-ray/radiology and sanitation). 75 staff members surveyed, 25 (33.3%) worked in the outpatient department, 31 (41.3%) in the intensive care unit, 11 (14.7%) in reception, and 1 (1.3%) as sanitation workers. The next section of the questionnaire focused on assessing the impact of COVID-19 on the health of medical workers at Zangiota Hospital No. 2, specializing in the treatment of COVID-19 patients (Table 1). It was found that during the study period, 16 (21.3%) hospital employees contracted COVID-19, while 59 (78.7%) did not. Regarding exposure, 58 (77.3%) had direct contact (within 1 meter) with a COVID-19-infected patient, 6 (8%) did not have such contact, and 11 (14.7%) were unsure. Similarly, 58 (77.3%) reported direct contact with a surface contaminated with COVID-19, while 6 (8%) did not have contact within 1 meter, and 11 (14.7%) were unsure.
|
|
|
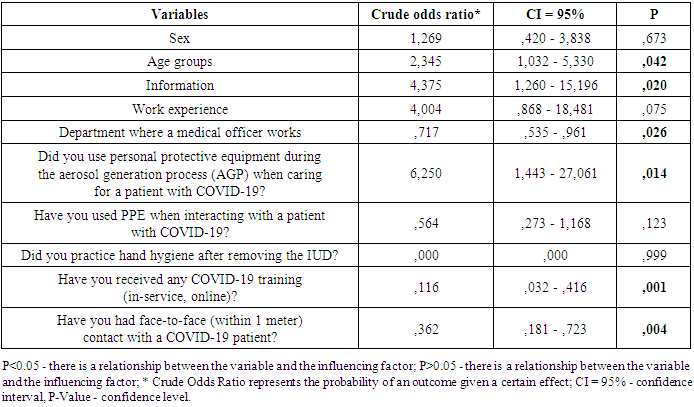
5. Conclusions
- Through questionnaires, hospital staff specializing in the treatment of COVID-19 patients identified high-risk conditions for contracting the disease. These include age groups of staff, education level, department where medical staff work, proximity to patients, adherence to PPE usage during medical procedures, completion of COVID-19 training, and face-to-face contact with patients within 1 meter. Addressing these factors is crucial for protecting employee health, reducing illness among staff, and preventing disabilities.
References
| [1] | Grebenkov, V., Batov, V. E., Kuznetsov, S. M. (2021). Assessment of working conditions for medical workers of military medical organizations during the pandemic of a new coronavirus infection. Medico-biological and socio-psychological problems of safety in emergency situations, No. 3, 35-40. |
| [2] | Alhouri. A., Abu Shokor. M., Marwa. K., Sharabi. A., Mohammad Nazir Arrouk. D., Al Houri. F. N., Al Houri. H. COVID-19 and Its Impact on Healthcare Workers: Understanding Stigma, Stress, and Quality of Life. Cureus, (2023). 15(4), e37846. https://doi.org/10.7759/cureus.37846. |
| [3] | Bielicki. Julia. A et al. “Monitoring approaches for health-care workers during the COVID-19 pandemic.” The Lancet. Infectious diseases vol. 20.10 (2020): e261-e267. doi:10.1016/S1473-3099(20)30458-8. |
| [4] | Ng.K., Poon.B., H., Kiat. Puar.H., Shan Quah. J. L., Loh. W. J., Wong, Y. J., Tan.T. Y., Raghuram. J. COVID-19 and the Risk to Health Care Workers: A Case Report. Annals of internal medicine, (2020) 172 (11), 766–767. https://doi.org/10.7326/L20-0175. |
| [5] | U.S. Department of Labor Occupational Safety and Health Administration OSHA 3990-03 2020 Guidance on Preparing Workplaces for COVID-19 (osha.gov). |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML