Khikmatullaeva Malika Rakhimjonovna
Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan
Correspondence to: Khikmatullaeva Malika Rakhimjonovna, Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Caesarean section is one of the most common surgical interventions in obstetrics. It is performed when vaginal birth poses a threat to the health of the mother or baby. As a complication of this operation, an isthmocele is formed - a defect in the uterus after surgery, which can affect the woman's health in the future.
Keywords:
Caesarean section, Scar on the uterus, Isthmocele, Suture, Lower segment of the uterus
Cite this paper: Khikmatullaeva Malika Rakhimjonovna, Isthmocele after Cesarean Section – A New Solution to the Problem, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 1974-1976. doi: 10.5923/j.ajmms.20241408.05.
1. Introduction
In recent decades, the topic of quality of suture repair on the uterus after cesarean section surgery, failure of which results in local thinning of the myometrium with the formation of the so-called isthmocele [4].An isthmocele is defined as a protrusion on the anterior wall of the isthmus of the uterus or cervical canal, located next to a cesarean section scar [10,12]. The prevalence of symptomatic isthmocele after cesarean section is still unknown [8,11]. Various studies have reported wide variations ranging from 19.4% to 88% [5,14]. Considering the literature data, complications identified in women with isthmocele are steadily increasing [7,8].Poor myometrial contractility around the isthmocele, caused by the presence of fibrous tissue, often leads to a lack of blood flow in this area. The accumulation of blood during the menstrual cycle at the level of the scar leads to subsequent spotting, usually during the first week of the cycle. This symptom is most often considered a symptom of AUB [8]. It is known that hormonal therapy symptomatically stops bleeding. Over the past few years, these complications have been treated with drug therapy, but this is not a radical treatment method [2,5,9].An integrated approach to the early diagnosis of isthmocele, timely correction of manifested complications, as well as preventing the manifestation of a defect after a surgical scar using optimized methods for restoring the integrity of the uterus during a cesarean section will greatly reduce the development of isthmocele.The purpose of the study is to evaluate the effectiveness of a new surgical suture to restore the integrity of the uterus during cesarean section and prevent the development of isthmocele.
2. Materials and Methods of the Research
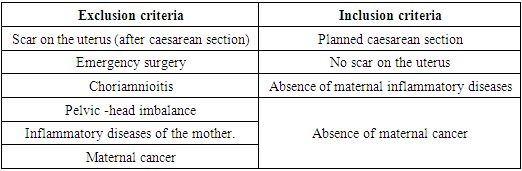
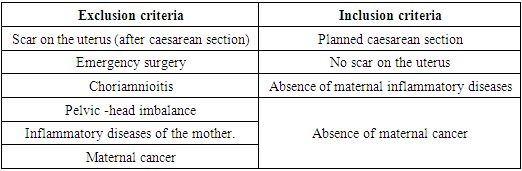
About examined 98 female patients who underwent operative delivery. All patients were divided into two groups: 48 postpartum women who A caesarean section was performed with a new surgical method of restoring the integrity of the uterus - the main group. To compare the effectiveness and the surgical suture technique we proposed, we examined 50 patients who had undergone surgical delivery using the traditional method. Considering the literature on the effectiveness of surgical sutures [4], inclusion and exclusion criteria for the study group were introduced [1,3,5,8]. (Table 1)Table 1. Inclusion and exclusion criteria for study groups
 |
| |
|
Progress of surgery differed only in the method of suturing the lower uterine segment. There were no other differences. During the operation, the following parameters were studied: time to extraction fetus, total duration of operation, average blood loss, the characteristics of the uterus were assessed, the need for additional hemostasis in during surgery, time spent on suturing the uterus, the need to use uterotonics. In the postoperative period, everyone in the first two days, postpartum women received infusion therapy, prevention of thromboembolic complications was carried out, and according to indications, uterotonics, to regulate contractile function uterus and antibiotics.According to the American Association of Obstetricians and Gynecologists (ACOG) [1,6], ultrasonography and Doppler examination of the pelvic organs can be used to detect isthmocele with a sensitivity of 82 and 96%, specificity of 85 and 90%, respectively [6,8]. All postpartum women underwent ultrasound examination on 2, 5, 7 days after surgical delivery and in the long-term period after cesarean section 1, 3, 6, 12 months after cesarean section.
3. Results and Discussions
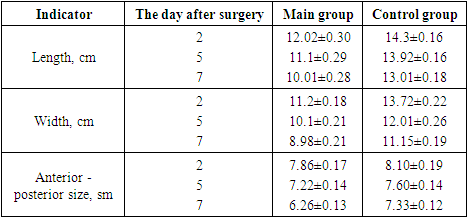
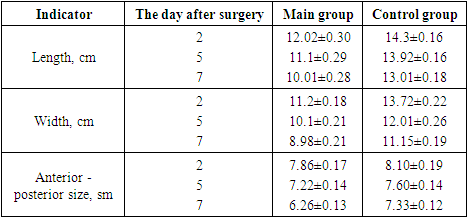
In the early postpartum period at 2, 5, 7 days. transabdominal biometry of the uterus was performed. This study allows timely diagnose subinvolution of the uterus, the presence of pathological inclusions in its cavity, and the condition of the suture.Table 2. Transabdominal biometry of the uterus
 |
| |
|
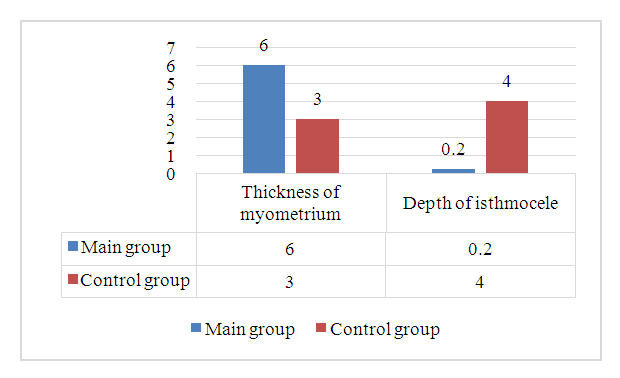
The results show that the rate of involution the uteruses are somewhat delayed in the control group, where the lower uterine segment was restored using the traditional method. Whereas in the main study group, where is the restoration of the lower segment of the uterus was carried out in a new way, the average values of these quantities approached normative for the postpartum period. It was found that patients in the control group had lochiometers more often (48%, n = 24) compared to the main study group.Besides control of involutive changes in the uterus, dynamic ultrasound examination of the formation of a scar on the uterus was carried out under the conditions of various application techniques seams on the bottom uterine segment. In the early stages after surgery, no obvious ultrasound signs of isthmocele were detected; the nature of the uterine scar was assessed. In the control group, the developing scar was significantly unevenly thickened (62%, n =31), in some areas asymmetrical, in the seam zone there are both point and linear inclusions and large ones of increased echogenicity (reflection of suture material), discontinuity of the scar line. In 73% (n =35) of patients in the main group, uniform, scar symmetrical in all parts, homogeneous structures. There were no significant inflammatory changes. Echostructure the scar almost corresponded in acoustic density to the wall of the uterus (p < 0.01). In the control group, heterogeneity of the myometrium (56%, n = 28), an area of increased echogenicity, still remained at discharge from the maternity hospital. The thickness of the uterine wall in the area of the scar has not changed, and sometimes even increased. And in the main group, the ultrasound picture looked more favorable - the postoperative line the suture was poorly visualized (87.5%, n = 42), there was a slight increase in echogenicity, corresponding encapsulated ligatures.In the long term after caesarean section, ultrasound the study was carried out on 90 patients: 45 women from each group. Ultrasound examination was carried out with a vaginal sensor, 1, 3, 6 and 12 months after surgery. Dilatation of the uterine cavity was not detected in any of the cases. Greatest During this study, attention was paid to identifying isthmocele and echographic assessment of the anterior wall of the uterus in the projection of the scar. In the main group there was a study where the lower segment of the uterus was restored using a new surgical method, suture was rarely visualized on the uterus. No uneven contours of the endometrium were detected. Sometimes visualized areas of high acoustic density in the scar area apparently encapsulated ligatures (8.8%). Whereas in the control group, using a traditional suture, heterogeneity of the endometrium was detected in 62.2% (28) of patients, zones of increased echogenicity along the suture line in 48.8% (22) of women. Also, in this group visualized myometrial defects in the form isthmocele in 42.2% (19) of cases. These patients had complaints indicating the presence of isthmocele in the postoperative period, namely, prolonged bleeding from the genital tract, painful menstruation, dysmenorrhea, hypermenorrhea (p < 0.01).It was found that the thickness of the myometrium in the area of the uterine scar was higher in the study group compared to the control group. The mean isthmocele depth was 4.6 mm (p < 0.05). Also, in the control group, no blood flow was detected in the area of the postoperative scar, whereas in the main group there was complete vascularization of this area. (Figure 1.)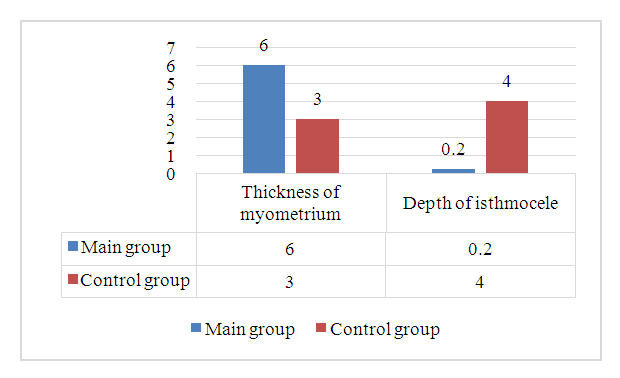 | Figure 1. Comparative analysis of myometrial thickness and isthmocele depth 12 months after cesarean section |
Thus, ultrasound examinations of early and remote periods of scar formation on the uterus are said to about the advantages of the new technique for restoration of the lower segment of the uterus and indicate the possibility of forming a full suture on the uterus. Also, our proposed method eliminates the disadvantages of previously proposed sutures for suturing the wound, which makes the method safer and more optimal for use.
4. Conclusions
1. The rate of uterine involution is delayed when restoration of the lower uterine segment using the traditional method. Whereas when a suture is applied to the uterus using the new ultrasound technique, the picture looks more favorable;2. Sewing wounds on the uterus during a caesarean section a new surgical method makes it possible to prevent the manifestation of isthmocele, as well as significantly increase the thickness of the myometrium (p < 0.05); 3. Using an optimized method for restoring the integrity of the uterus during a cesarean section, the development of isthmocele will be greatly reduced, as well as helps normalize the menstrual cycle, reduce severity of symptoms such as postmenstrual bleeding from the genital tract, dysmenorrhea, hypermenorrhea (p < 0.05).The above data confirm that the new method of reconstructing the lower segment of the uterus has sufficient advantages to be widely used in cesarean sections. The increase in operative births with the subsequent development of isthmocele and its complications dictates that this method should be considered key in the prevention of uterine scar failure after operative birth.
References
| [1] | Barba, M., Cola, A., Passoni, P., La Milia, L., De Vicari, D. and Frigerio, M. (2023), Transvaginal repair of isthmocele after cesarean scar pregnancy. Int J Gynecol Obstet, 162: 775-776. |
| [2] | Budny-Winska J, Pomorski M. Uterine niche after cesarean section: a review of diagnostic methods. Ginekol Pol 2021; 92: 726–730. |
| [3] | En'kova EV [Prediction of uterine scar failure by assessing the mast cell population] / EV En'kova, DA Atyakshin, VA Vukolova et al /[Scientific results of biomedical research]. – 2019. – V. 5. – No. 2. – P. 86–95. |
| [4] | Laganà, A. S., Garzon, S., Alkatout, I., Hortu, İ., Gitas, G., Vitale, S. G., & Gubbini, G. (2022). Isthmocele: When Surgery Is Both the Problem and the Solution. Journal of Investigative Surgery, 35(1), 231–232. |
| [5] | Martynov S.A., Adamyan L.V. Scar on the uterus after cesarean section: terminological aspects. Gynecology 2020; 22(5): 70-75. (Martynov SA, Adamyan LV Uterine scar after cesarean section: terminological aspects. Ginekologija 2020; 22 (5): 70-75). |
| [6] | Menacker F, Hamilton BE. Recent trends in cesarean delivery in the United States. NCHS Data Brief. 2023; 35: 1-8. |
| [7] | Moretti L, Stalfort J, Barker TH, Abebayehu D. The interplay of fibroblasts, the extracellular matrix, and inflammation in scar formation. J Biol Chem. 2022; 298(2): 101530. |
| [8] | Murji A, Sanders AP, Monteiro I, Munro MG et al. Cesarean scar defects and abnormal uterine bleeding: a systematic review and meta-analysis. Fertil Steril. 2022; 118(4): 758-766. |
| [9] | Rupa R, Kushvaha S, Venkatesh K. Uterine Isthmocele-A Frequently Overlooked Complication of Cesarean Sections. Indian J Radiol Imaging. 2021 Oct 26; 31(3): 601-604. doi: 10.1055/s-0041-1736393. PMID: 34790304; PMCID: PMC8590568. |
| [10] | R Basel Al-Ghotani, Nafiza Martini, Ebaa Alabdallah, Ieman Alawad, Khaled Hussien, A large post-caesarean Niche (Isthmocele) with amenorrhea, a symptom that was not reported in the medical literature: A rare case report, International Journal of Surgery Case Reports, Volume 109, 2023, 108528, ISSN 2210-2612. |
| [11] | Thaysa Guglieri Kremer, Isadora Bueloni Ghiorzi, Raquel Papandreus Dibi. [Isthmocele: an overview of diagnosis and treatment]. REV ASSOC MED BRAS 2021; 65(5): 714-721. |
| [12] | Vukolova VA, Yen'kova EV Effect of Different Suturing Methods on Uterus Postsurgical Cicatrix after Cesarean Section. Journal of experimental and clinical surgery 2017; 10: 3: 241-245. DOI: 10.18499/2070-478X-2017-10-3-241-245. |
| [13] | Vitale SG, Ludwin A, Vilos GA, Torok P et al. From hysteroscopy to laparoendoscopic surgery: what is the best surgical approach for symptomatic isthmocele? A systematic review and meta-analysis. Arch Gynecol Obstet. 2020; 301: 33 -52. |
| [14] | Yuldashev Sanjar Keldiyarovich and Khikmatullaeva Malika Rakhimjonovna (2023) “Istmocele and fertility. A modern solution to the problem (literature review)”, Journal of reproductive health and uro -nephrology research, 4(1), p. 30. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML