-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(8): 1971-1973
doi:10.5923/j.ajmms.20241408.04
Received: Jul. 20, 2024; Accepted: Aug. 3, 2024; Published: Aug. 6, 2024

Assessment of Cytokine Status with Endometrial Hyperplastic Processes in the Reproductive Period
Miraliev F. K.
Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan
Correspondence to: Miraliev F. K., Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The purpose of the study was to study the assessment of cytokine status with endometrial hyperplastic processes in the reproductive period. The data obtained indicate that immune changes during abnormal uterine bleeding in combination with non-atypical endometrial hyperplastic processes occur at the systemic level and indicate an ongoing inflammatory process at the time of examination. In this regard, determining the concentration of cytokines in peripheral blood is prognostically significant for diagnosis and monitoring the effectiveness of therapy in this cohort of patients.
Keywords: Endometrial hyperplasia, Cytokine status, IL-1β, TNFα, IL-2, IL-4, IL-6, IL-8
Cite this paper: Miraliev F. K., Assessment of Cytokine Status with Endometrial Hyperplastic Processes in the Reproductive Period, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 1971-1973. doi: 10.5923/j.ajmms.20241408.04.
Article Outline
1. Introduction
- Hyperplastic processes of the endometrium in the structure of gynecological pathology occupy from 15.0% to 50.0% in women of reproductive age. Women's health and gender pathology remain priority areas of prognostic, preventive and personalized medicine [1,2,6,9]. The relevance of the study of endometrial hyperplasia (EH) is primarily due to the high risk of malignant transformation and problems associated with menstrual irregularities, dysfunctional uterine bleeding, and anemia in women. Endometrial hyperplasia occupies a significant place in the structure of gynecological morbidity in women of reproductive age and is one of the most common reasons for hospitalization in a gynecological hospital (from 10% to 18%) [5,7,10].With a high recurrence rate of endometrial hyperplasia, the risks of malignancy require further improvement and the search for new approaches to the diagnosis and treatment of this disease [3,4,8]. More studies on histological features and immunological profiles are needed to find an association between endometrioid and high-grade endometrial carcinoma and endometrial pathology.Most scientific research in recent years has been devoted to the study of both systemic immunity and local immunity of the endometrium in endometriosis, uterine fibroids, chronic endometritis and recurrent miscarriage. At the same time, data on the state of immunity during endometrial hyperplastic processes (EHP) in patients with abnormal uterine bleeding (AUB) are extremely contradictory [3].Purpose of the study is to study the assessment of cytokine status with endometrial hyperplastic processes in the reproductive period.
2. Materials and Methods of the Research
- The work was an open, prospective, comparative study in parallel groups. The criteria for inclusion of patients in the study were: 1) the age of the patients from 18 to 35 years; 2) the presence of AUB in combination with non-atypical forms of endometrial hyperplasia (simple endometrial hyperplasia (SHE) without atypia; 3) the presence of AUB in combination with non-atypical forms of endometrial hyperplasia (complex endometrial hyperplasia (CHE) without atypia The exclusion criteria were: 1) endometrial polyps; 3) atypical hyperplasia and endometrial cancer; 4) large uterine fibroids; submucosal localization of myomatous nodes; 5) external genital and extragenital endometriosis, grade I–III adenomyosis; 6) acute inflammatory diseases of the pelvic organs; 7) the presence of allergic reactions. All patients upon admission to the hospital underwent hysteroscopy with separate diagnostic curettage and subsequent histological examination of scrapings of the mucous membrane of the uterine cavity and cervical canal.Based on histological examination of endometrial tissue, all patients were divided into two groups: group I consisted of 63 women with AUB in combination with PGE without atypia; Group II - 63 patients with AUB in combination with CGE without atypia. The control group consisted of 25 apparently healthy women with endometrium in the proliferation phase.To study the levels of proinflammatory cytokines - tumor necrosis factor-α (TNF-α), interleukins (IL) - IL-1β, -2, -6, and interferon-γ (IFN-γ) - in peripheral blood plasma, the enzyme-linked immunosorbent assay method was used. analysis using the sandwich method using reagent kits for enzyme immunoassay “Vector BEST” (Russia).Immunological data were processed according to the principle of normal distribution using the Student's t test, the arithmetic mean and its standard error were calculated.
3. Results and Discussions
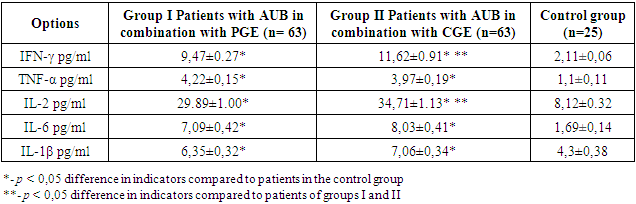
- Analysis of the data we obtained on the concentration of cytokines in peripheral blood serum indicates an ongoing inflammatory process at the time of examination and has signs of a systemic inflammatory reaction.As shown by the results of the study of cytokine status, patients with abnormal uterine bleeding with PGE without atypia had changes in the content of proinflammatory cytokines (Table 1).
|
4. Conclusions
- Thus, the data obtained indicate that immune changes during abnormal uterine bleeding in combination with non-atypical endometrial hyperplastic processes occur at the systemic level and indicate an ongoing inflammatory process at the time of examination. Thus, the data is obtained to indicate that immune changes during abnormal uterine bleeding in combination with non-atypical endometrial hyperplastic processes occur at the systemic level and indicate an ongoing inflammatory process at the time of examination. The identified disorders may also indicate a local inflammatory process in the uterine mucosa if there are hyperplastic changes in it.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML