-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(8): 1962-1965
doi:10.5923/j.ajmms.20241408.02
Received: Jul. 15, 2024; Accepted: Jul. 31, 2024; Published: Aug. 2, 2024

Retrospective Analysis of Women with Pelvic Organ Prolapse
Buribaeva Asal I.
Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan
Correspondence to: Buribaeva Asal I., Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, Tashkent, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents data from a retrospective analysis of the history of women operated on with pelvic organ prolapse after hysterectomy at the Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health. The frequency of occurrence, features of the course of the disease and the frequency of the form of genital prolapse were studied.
Keywords: Hysterectomy, Pelvic organ prolapse, Uterine fibroids
Cite this paper: Buribaeva Asal I., Retrospective Analysis of Women with Pelvic Organ Prolapse, American Journal of Medicine and Medical Sciences, Vol. 14 No. 8, 2024, pp. 1962-1965. doi: 10.5923/j.ajmms.20241408.02.
Article Outline
1. Relevance
- According to various statistical studies, the incidence of pelvic organ prolapse in postmenopausal women reaches 50%, which is especially important in the presence of comorbid pathology, affecting not only the effectiveness of surgical correction, but also the quality of life of patients [1,2,4]. Pelvic organ prolapse (POP) is one of the most common problems among the female population [2,3,6,8]. Vaginal surgery for genital prolapse using your own tissue is associated with an increased risk of recurrence and failure [5,6,7]. Correction of POP using synthetic mesh via vaginal access is associated with an increased risk of vaginal erosions, implant extrusions, and repeat surgery [9]. The use of laparoscopic sacrocolpopexy may be accompanied by the development of complications as a result of the location of a number of important anatomical landmarks in the promontorium area, especially in the presence of risk factors such as obesity and adhesions [12]. Damage to the hypogastric nerve contributes to the development of constipation, and injury to the intestinal wall or bladder during dissection occurs with a frequency of up to 10%, especially in conditions of increased body mass index [11]. Despite the variety of surgical methods for correcting genital prolapse and stress urinary incontinence, the available data are contradictory. The issue of surgical treatment of genital prolapse requires further study, taking into account an individual approach for each patient.Purpose of the study: To study clinical and anamnestic data in women with pelvic organ prolapse after total hysterectomy.
2. Materials and Methods of the Study
- A retrospective analysis was carried out at the Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health for the period 2020-2023. The object of the study was women with genital prolapse who underwent hysterectomy using laparotomy (abdominal), vaginal and laparoscopic approaches due to uterine fibroids. All operations were performed for the purpose of surgical treatment of uterine fibroids. All women underwent a comprehensive clinical and laboratory examination and preparation for planned surgical treatment for uterine fibroids larger than 12 weeks. Patients with uterine fibroids underwent examination and training at the scientific advisory clinic “Family and Marriage” of the Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health, after which they were hospitalized for surgical treatment in the department of operative gynecology of the Republican Specialized Scientific and Practical Medical Center for Maternal and Child Health. Gynecological status was determined based on examination of the external genitalia, examination of the vagina and cervix using speculum, bimanual vaginal examination, and, if indicated, rectal-vaginal examination. During a bimanual examination, the position, mobility, size, consistency, shape of the uterus, localization and size of myomatous nodes, and their pain on palpation were determined. The condition of the uterine appendages, pelvic tissue, the condition of the vaginal vaults and uterosacral ligaments was determined.The data obtained during the study were subjected to statistical processing on a Pentium-IV personal computer using the Microsoft Office Excel-2003 software package, including the use of built-in statistical processing functions. Methods of variational parametric and nonparametric statistics were used with the calculation of the arithmetic mean of the studied indicator (M), standard deviation (σ), standard error of the mean (m), relative values (frequency, %), the statistical significance of the obtained measurements when comparing average values was determined by the criterion Student's t test (t).
3. Results of the Study
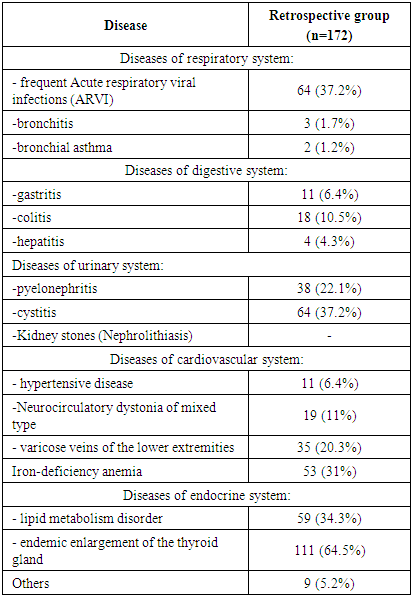
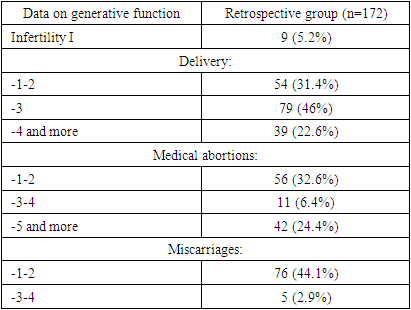
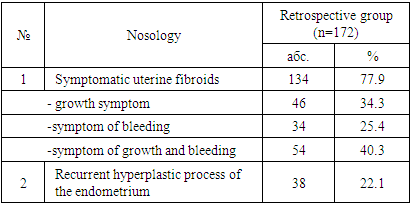
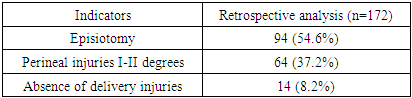
- The surgical histories of 172 women who underwent total hysterectomy were studied. The age of the women was from 45 to 52 years; the average age was 49.4±1.78 years.The results of studying the somatic status of those examined are presented in Table 1. As can be seen from Table 1, many patients suffered from various diseases in the past. Most often, the patients indicated diseases of the urinary system.
|
|
|
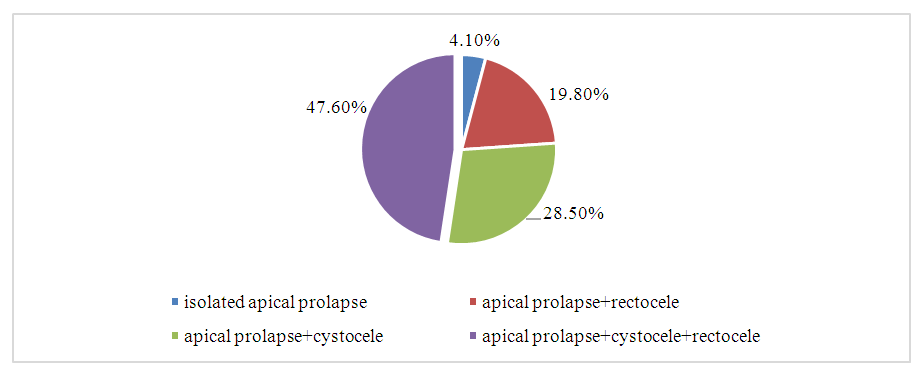 | Figure 1. Structure of forms of pelvic organ prolapse, (%) |
|
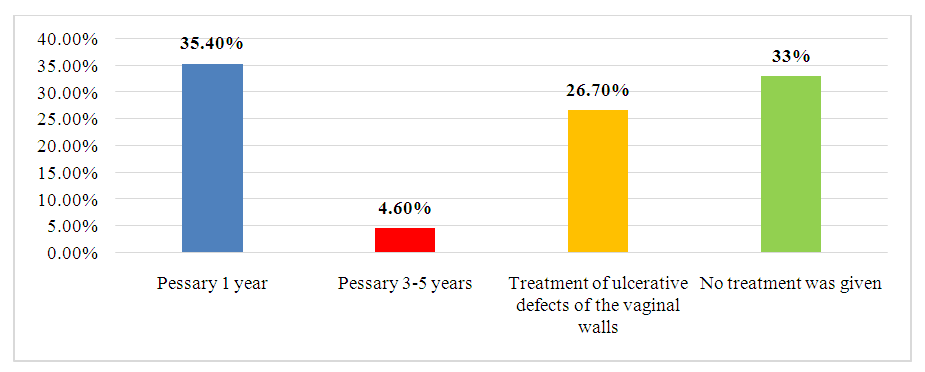 | Figure 2. Conservative treatment of pelvic organ prolapse in the anamnesis (medical history of the patients) |
4. Conclusions
- Thus, the results of examination of the patients before surgical treatment confirmed the multifactorial nature of the causes of pelvic organ prolapse and the accompanying disorders by adjacent organs. Summarizing the assessment of the general condition of hospitalized patients, when considering all the factors combined, we can conclude that pelvic organ prolapse needed to be surgically treated. Indications for surgery were determined by the diagnosis made on the basis of a comprehensive clinical and laboratory examination. The decision on the extent of surgical treatment was made individually.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML