-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1931-1933
doi:10.5923/j.ajmms.20241407.42
Received: Jul. 3, 2024; Accepted: Jul. 25, 2024; Published: Jul. 26, 2024

Features of Metabolic Changes in the Liver in Patients with Pancreatic Steatosis
D. Kh. Jabborova1, G. R. Yuldasheva2, L. T. Daminova1
1Tashkent State Dental Institute, Tashkent, Uzbekistan
2Center for Development of Professional Qualifications of Medical Workers Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study involved 69 people. ALT, AST, total and direct bilirubin, ALP, GGT, and fecal elastase were studied. In addition, serum total protein, albumin, cholesterol, triglycerides, LDL, VLDL, glucose, insulin, and leptin concentrations were taken into account. The results showed that patients with pancreatic steatosis combined with MS have disturbances in glucose-insulin homeostasis, caused not only by hormonal disorders, but also by changes in cellular metabolism due to the main substrate - free fatty acids.
Keywords: Pancreatic steatosis, Metabolic disorders in the liver, Metabolic syndrome, Insulin, Glucose, Leptin
Cite this paper: D. Kh. Jabborova, G. R. Yuldasheva, L. T. Daminova, Features of Metabolic Changes in the Liver in Patients with Pancreatic Steatosis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1931-1933. doi: 10.5923/j.ajmms.20241407.42.
Article Outline
1. Introduction
- Pancreatic steatosis (PS) is one of the leading pathologies of the digestive system. The significant prevalence of the disease is determined by the central role of the pancreas in the organization of cavity digestion. Lesions in CP exocrine pancreas invariably involve the endocrine part in the pathological process, PS, insulin resistance and diabetes mellitus occur, which are invariable companions of metabolic syndrome (MS) [2,3]. The main components of the cascade of metabolic disorders or metabolic syndrome are closely related to the functional state of the digestive organs. Eating disorders, imbalance of hormones in the digestive tract, functional state of the liver and pancreas are key pathogenetic factors in the development of MS. As a result of the listed disorders, metabolic changes sometimes develop in many organs and systems at the cellular level [1,2]. Meanwhile, pancreatic lesions in patients with MS were more common in women and a relationship was found between pancreatic and liver lesions, which is one of the causes of metabolic disorders [4,5]. Despite the large number of publications on the problem of metabolic syndrome and long-term life expectancy, the available literature lacks clear criteria for determining the severity of metabolic disorders in the liver, which may lead to adjustments in patient management tactics.The aim of the study: to study some features of metabolic disorders in the liver in patients with pancreatic steatosis in combination with metabolic syndrome.
2. Material and Research Methods
- The study involved 69 people, including 14 men and 55 women, average age 52.2±2.6 years. All patients were referred for inpatient treatment with a diagnosis of chronic pancreatitis (CP), presenting or increasing pain 30-40 minutes after eating, the control group consisted of 14 people without manifestations of PS and MS (conditionally healthy).The diagnosis of CP was made on the basis of clinical, laboratory and instrumental studies and was based on the decision of the European Association of Pancreatologists. However, according to ultrasound data, CP was detected. The activity of the inflammatory process was assessed based on the indicators of a clinical blood test, amylase activity in the blood serum and urine, C-reactive protein alanine and aspartate transaminases (ALT and AST), as well as the activity of fecal elastase. To determine possible cholestasis, the indicators of total and direct bilirubin, alkaline phosphatase (ALP), gamma-glutamyl transpeptidase (GGT) were studied. When studying the trophic status of patients, serum total protein, albumin, cholesterol, triglycerides, low-density and very low-density lipoproteins were taken into account from laboratory indicators, the absolute number of lymphocytes was calculated.To assess changes in the exocrine function of the pancreas, all patients underwent a coprogram study. To optimize the study and identify hidden steatorrhea, three days before the study, patients were prescribed a diet with a fat content of 70-80 g / day and enzyme preparations were canceled. In addition, transabdominal ultrasound was performed using the Philips-SD-360 device. During the ultrasound, the sizes and acoustic structure of the pancreas, liver, gallbladder, spleen, the condition of the vessels of the portal system, and mesenteric vessels were assessed. The condition of the pancreatic and bile ducts was carefully studied.The combined form of LD with MS was diagnosed according to the criteria proposed by experts of the US National Cholesterol Education Program (2009). The criteria for MS were waist circumference greater than 102 cm in men and greater than 88 cm in women; blood pressure of 130/85 mm Hg and above, serum triglyceride content of 1.7 mmol/l and above, HDL-C less than 1 mmol/l, fasting plasma glucose level of 6.1 mmol/l and above.Patients were informed about the details of the study and signed an agreement to participate in the scientific work.The concentration of glucose in the blood plasma was studied by the glucose oxidase method, using kits from the company “HUMAN”. The level of insulin was studied by the enzyme immunoassay, using kits from the company “DBG – Diagnostics”. The insulin resistance index was calculated using the HOMA-IR formula [Matthews. D., 2005]. A value greater than 2.27 was considered to indicate insulin resistance [Unger R.H., 2018]. The blood leptin level was studied by the enzyme immunoassay method, using kits from the company “DVS” supplied by the company “BioKhimMak” (Russia). The content of free fatty acids in the blood serum was determined using the NEFA FS test system from the company “DiaSis” (Germany). The following were determined as marker enzymes of cytoplasmic localization: the activity of fructose-1-phosphotaldolase, fructose-1,6 diphosphatase (V.I. Tovarishchsky’s method modified by Ya. Broginsky), the total activity of lactate dehydrogenase and gamma-glutamyl transpeptidase; the activity of malate dehydrogenase (Warburg optical method) was studied using kits from the company “HUMAN” as marker enzymes for mitochondria. The research used a biochemical analyzer from the companies “HOSPITAX” and “HUMAN”.Statistical processing of the study results was performed using the Statisticа-6.1 software package. The statistical significance of differences between the means in samples with a normal distribution was assessed using Student’s t-test (at p<0.05).
3. Results and Discussion
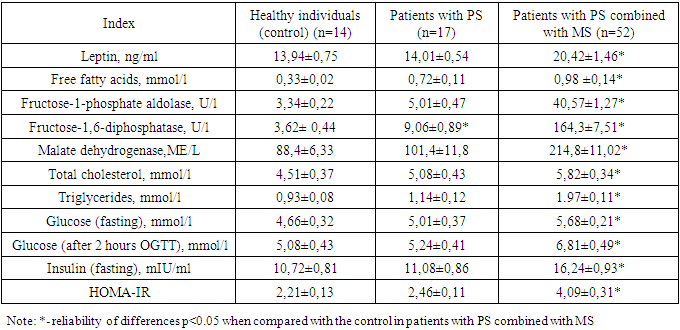
- The presented results of the study (Table 1) showed the presence of reliable changes in the studied blood parameters in patients with PS combined with MS. As indicated above, the state of dyslipidemia, manifested in most patients with a combined form of pathology, indicated the formation of a state of insulin resistance. The identified changes in the lipid spectrum of the blood were accompanied by an increase in the level of non-esterified fatty acids by an average of 3 times and indicated a violation of its transfer by the blood and absorption by cells. An increase in the level of free fatty acids in the blood is accompanied by a state of hyperinsulinemia an increase in the level of free fatty acids in the blood contributes to a violation of the function of insulin receptors and the absorption of glucose by cells. In this situation, the effect of lipotoxicity is accompanied by hyperinsulinemia and hyperglycemia, and is reflected in the dynamics of increasing leptin levels in the blood. According to many authors, leptin stimulates the proliferation of ß-cells of the islets of Langerhans by phosphorylating mitogen-activated protein kinase, just like insulin, and correlates with body mass index. In patients with PS, when compared with a group of healthy individuals, no significant changes were observed in the studied biochemical parameters.
|
4. Conclusions
- 1. Conditions of hypertriglyceridemia, hyperglycemia, hyperinsulinemia and hyperleptinemia against the background of high levels of free fatty acids activate the process of gluconeogenesis while inhibiting glycolysis. 2. Patients experience disturbances in glucose-insulin homeostasis caused by hormonal disturbances and changes in cellular metabolism due to free fatty acids.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML