-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1907-1913
doi:10.5923/j.ajmms.20241407.38
Received: Jun. 28, 2024; Accepted: Jul. 19, 2024; Published: Jul. 25, 2024

Preclinical Trials of Collagen and Hyaluronic Acid Based Gels for Use in Dental Surgery
Usmanova D. R.1, Mukimov O. A.1, Rajabov O. I.2, Shomurodov K. E.1
1Tashkent State Dental Institute, Uzbekistan
2Academy of Sciences of Uzbekistan Institute of Bioorganic Chemistry, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Regenerative medicine is aimed at expanding the possibilities of doctors to stimulate internal regenerative processes and provide artificial materials for tissue and organ repair. The article is devoted to the research of the effectiveness of collagen and hyaluronic acid based gels for application in surgical dentistry. The results of the experiment showed that the introduction of vitreous body and calcium gluconate in combination with collagen increased the regenerative activity of soft gingival tissues. The best results were observed with the combined administration of the preparations, which was characterised by the development of delicate collagen fibres and regenerative process at the injection site. Thus, the results of the study indicate the potential effectiveness of collagen and hyaluronic acid based gels in surgical dentistry to improve the regeneration processes of soft tissues.
Keywords: Collagen, Hyaluronic acid, Vitreous body, Standardisation and determination of gel stability, Surgical dentistry
Cite this paper: Usmanova D. R., Mukimov O. A., Rajabov O. I., Shomurodov K. E., Preclinical Trials of Collagen and Hyaluronic Acid Based Gels for Use in Dental Surgery, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1907-1913. doi: 10.5923/j.ajmms.20241407.38.
Article Outline
1. Relevance
- There are a large number of collagen-containing membranes on the market today. Most of them effectively fulfil barrier functions, but their insufficient thickness does not allow to achieve a significant increase in the volume of soft tissues. In contrast, a collagen matrix with a combined structure helps to fill soft tissue defects during a single operation, even in soft tissue deficiency, but the possibilities of its clinical application are still insufficiently studied. Due to the wide spread of such diseases as gingival recession, periodontitis, erosive and ulcerative lesions of the oral mucosa, alveolitis, the choice of optimal treatment tactics remains a serious problem. Gels allow to provide a large concentration of drugs directly in the focus of lesions, have optimal rheological properties, provide the most complete and rapid release of the main active substances. The most promising excipients are collagen and hyaluronic acid, which are characterised by prolonged action, high regenerative properties and indifference, and are widely used in the pharmaceutical industry, in particular for the creation of soft dosage forms [2,8]. There are different types of collagen, depending on location and function. To date, more than 20 types have been classified. Type I-IV collagens are the most abundant in the human body. Type I collagen is the main component of several commercially available collagen membranes (CMs), developed as an evolution of barrier membranes first introduced in the mid-1980s. The principle of so-called directed tissue regeneration was based on the membrane's ability to exclude epithelial and connective cells to enhance the ability of damaged periodontal tissue to regenerate to form new bone, periodontal ligament and cementum. The mould-forming ability of collagen is multifaceted. In the form of solutions it can be the basis of ointments, liniments, prolonger of liquid dosage forms (drops, injection solutions), thickener, etc. When solutions are air-dried, transparent films are formed, which are used as an independent dosage form. After freezing and lyophilic drying of solutions, highly porous structures (sponges) are obtained, the density of which depends on the initial concentration of collagen and other ingredients [6,7]. Spray drying of solutions or dispersion of dry films, sponges and other products yields powders that can be used as independent dosage forms and as excipients in the manufacture of other drugs. The vitreous body is composed of 90% hyaluronic acid and 10% water. The vitreous body (stroma vitreum) is formed by a thin network of interwoven fibres of different forms of collagen protein (vitreous-specific forms of collagens are also called vitrosins). The spaces between the fibres are filled with fluid (humor vitreus). This structure of the vitreous body gives it the character of a gelatinous mass [3]. Hyalocyte cells are present in the vitreous body, mainly located at its borders. These cells are involved in the secretion of hyaluronic acid, collagens and soluble proteins of the vitreous body, and also form hemidesmosomes, which provide attachment of the vitreous body to the retinal lining membrane. By origin, most hyalocytes are macrophages [4,5].Hyaluronic acid is also widely used in the pharmaceutical and cosmetic industries. Hyaluronic acid has a transport function - the polymeric network that hyaluronic acid forms on the surface of the skin allows the bioactive substances in various preparations to linger longer on it, increasing the likelihood that they will penetrate into the tissues. Hyaluronic acid has a high water-holding capacity - one hyaluronic acid molecule binds up to 5000 water molecules. The absorbed water is retained inside in the form of a gel and does not evaporate even when the humidity of the surrounding air decreases. We have developed several gel models using different excipients [1,2]. In this connection, the urgent task is to further study the properties of materials allowing to obtain a sufficient volume of attached keratinised gingiva, as well as to develop techniques contributing to the reduction of traumatism and the volume of surgical interventions. The aim of the research: Studying the influence of collagens of domestic production on the soft tissues repair by experimental way on animals.
2. Materials and Methods of Research
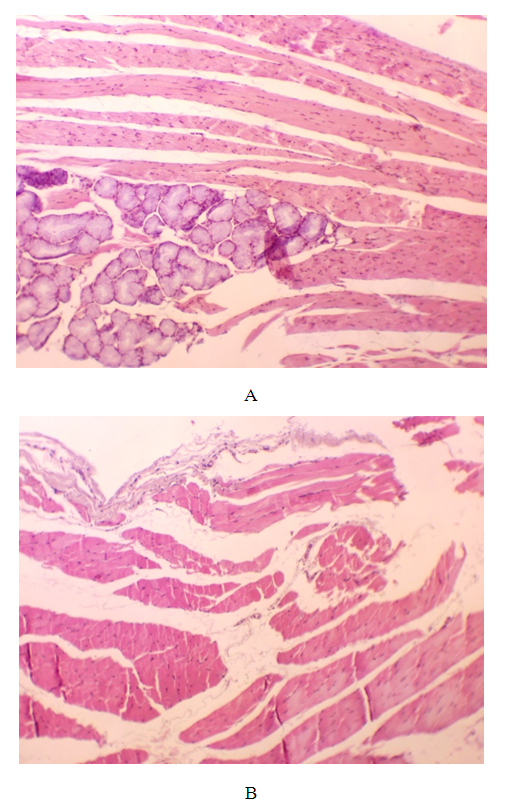
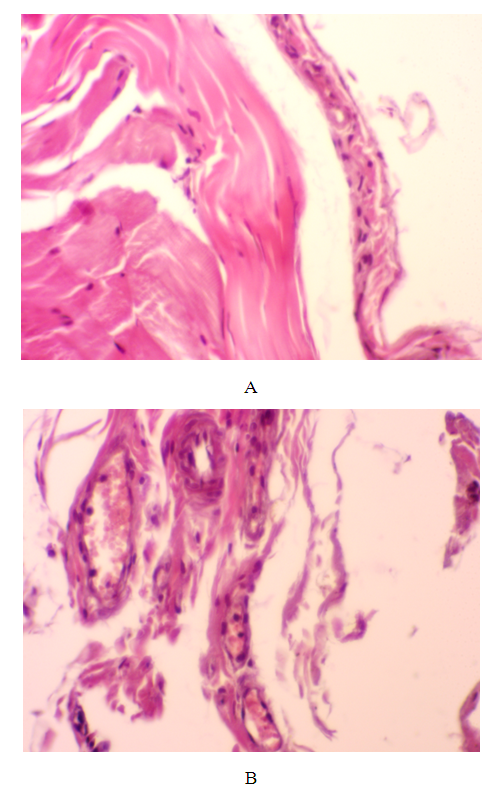
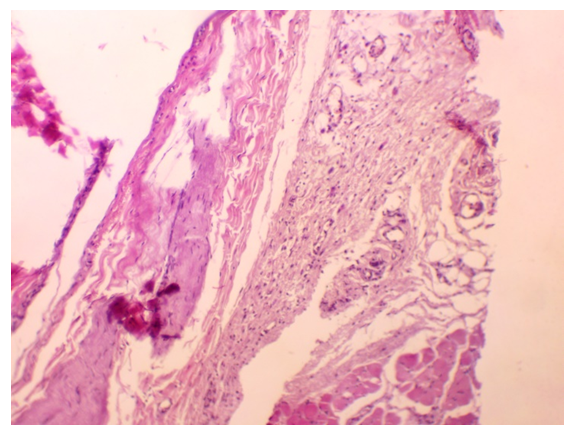
- The collagen "Bioplant" developed in the Institute of Biochemistry named after academician A.S.Sadikov was used to achieve the set goal. Vitreous body (90% hyaluronic acid and 10% water) and calcium gluconate solution (10% 10 ml) were used as a solvent. 5%, 10% and 15% solutions for injection with collagen were prepared. The technological process of gel preparation consisted of several stages: The first stage involved the preparation of drug substances and materials.The result of the first stage is the obtained mushy base (Fig. 1), which was obtained by dissolving the preparation "Bioplant" in the vitreous body in the volume of 0.5 ml, 1 ml and 2 ml. The solution was then placed in a 35°C water bath for 5 minutes. The obtained gel was a homogeneous mass of white colour with a weak characteristic odour (Fig. 2).
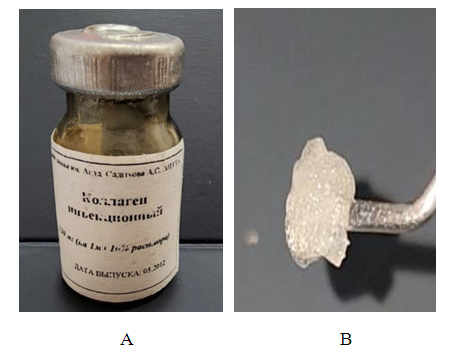 | Figure 1. A. Primary state of collagen. B. Collagen mixed with vitreous (in mushy form) |
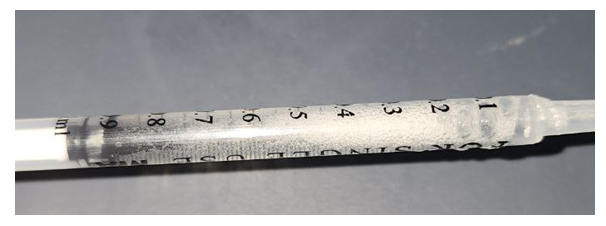 | Figure 2. Collagen dissolved in the vitreous and placed in a 35-degree bath |
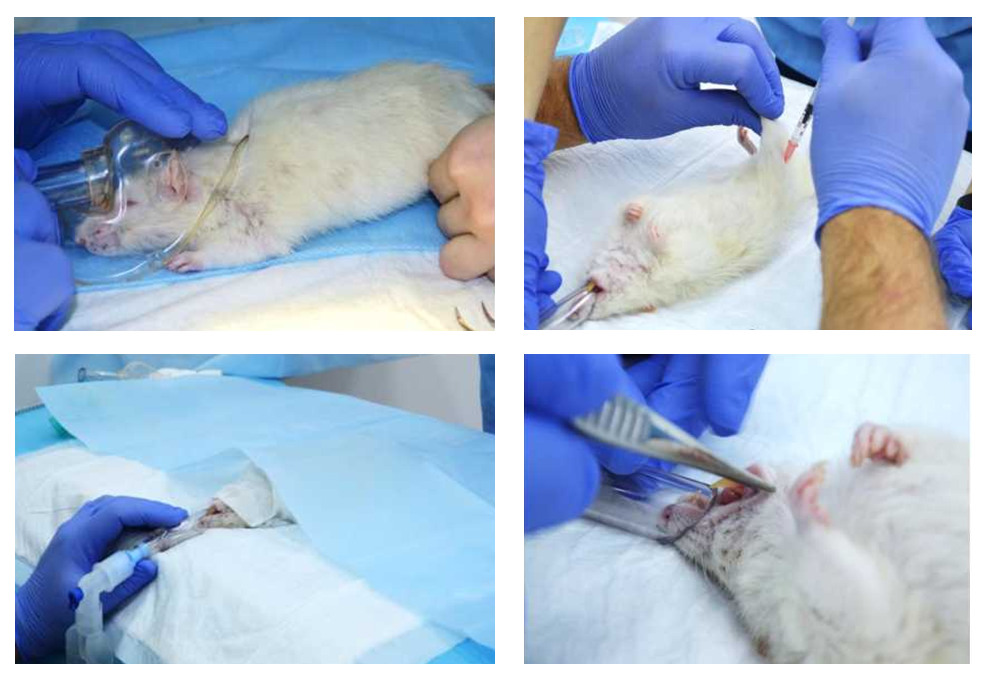 | Figure 3. Experiments were performed on male rats under aseptic conditions |
3. Results and Discussion
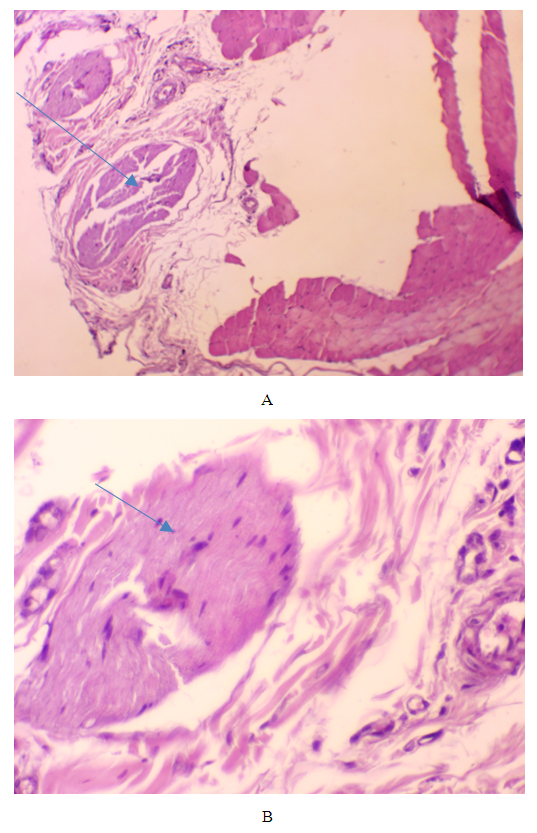
- I. Day 7 of the experiment.1). Intact group.The results of histological examination of soft tissues on the 7th day of the experiment in the intact control group showed the absence of signs of focal changes and other pathological processes. In fragments of muscle tissue transverse striation and nuclei were preserved, only in intermuscular layers swelling was determined. Fragments of the mucous membrane and salivary gland were also without visible changes (Fig. 4 A and B).
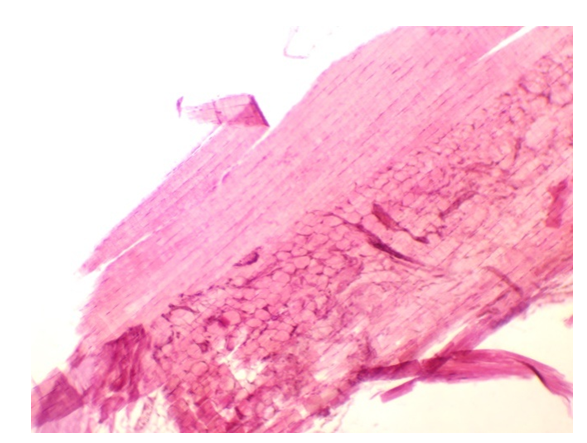
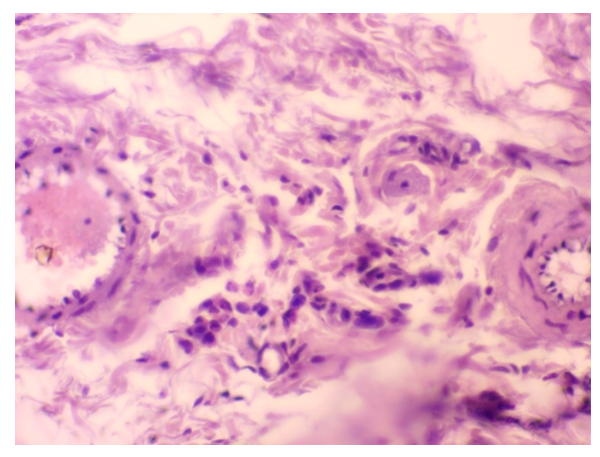
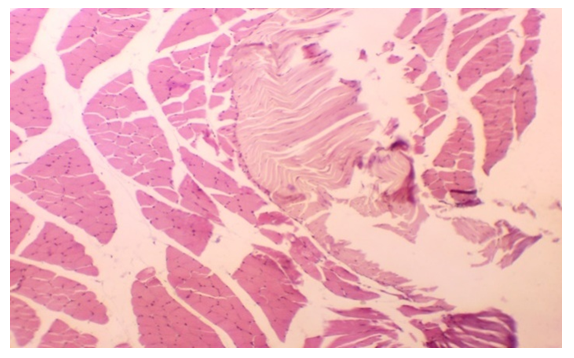 | Figure 5. 0.1 ml of vitreous with collagen. An area of thin fibrous collagen structure among the muscle tissue. Eq. vol. 10x10. Staining: haematoxylin and eosin |
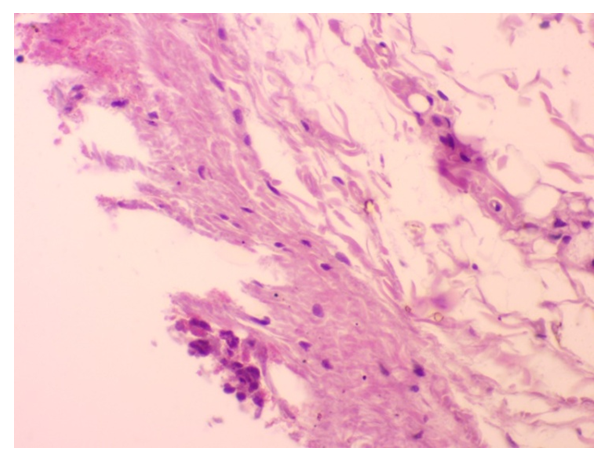
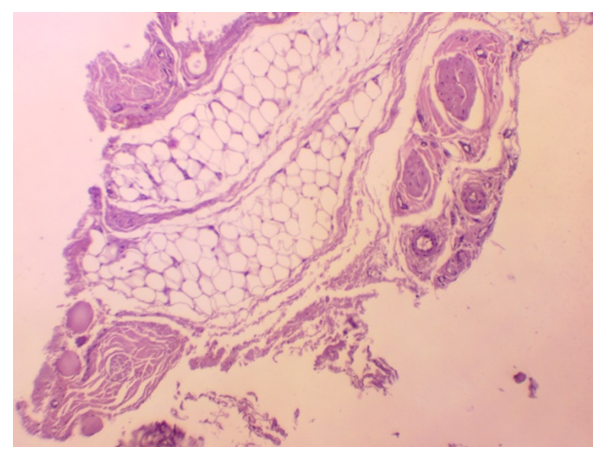
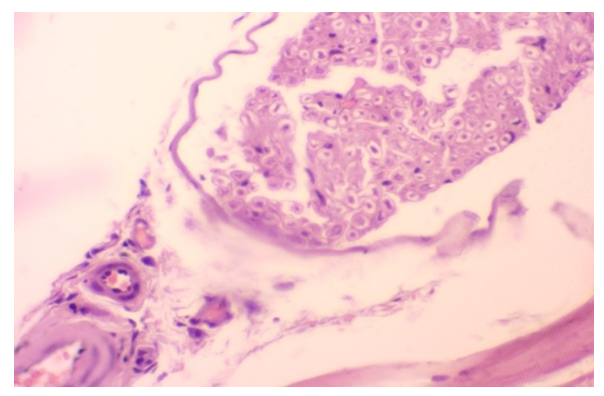 | Figure 10. 0.1 ml of vitreous with collagen. A section of soft tissue separated by a fibrous capsule included in the vitreous cavity. Haematoxylin and eosin staining. Eq. 10х10 |
 | Figure 11. 0.1 ml of vitreous with collagen. Areas of partial dissolution of the substance and its replacement by fibrous connective tissue. Haematoxylin and eosin staining. Eq. 10х10 |
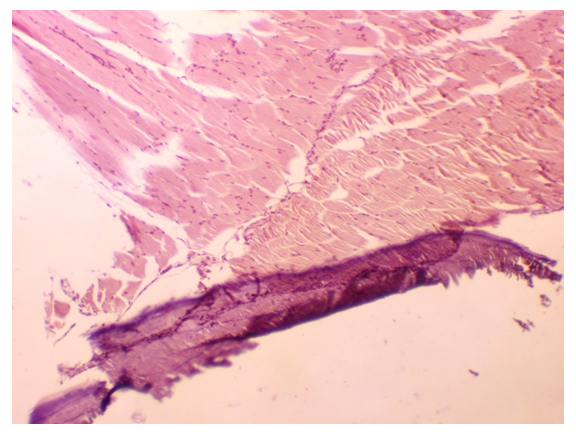
 | Figure 13. 0.1 ml calcium gluconate solution with collagen. Muscle, fibrofibrous tissue fragments and fatty fibre without visible changes. Haematoxylin and eosin staining. ob. 10x10. |
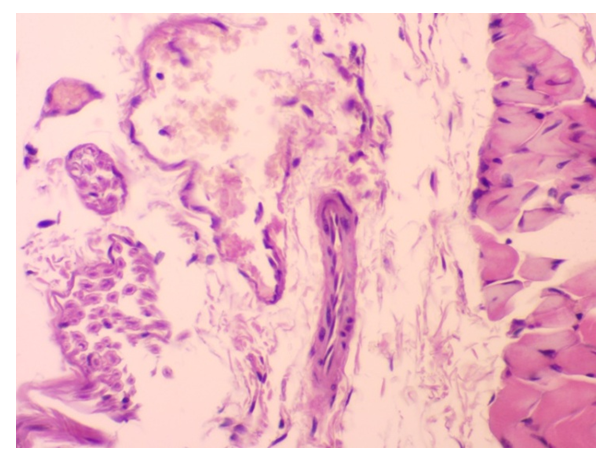 | Figure 14. 0.2 ml calcium gluconate solution with collagen. A section of formed collagen structures on a cross section. Haematoxylin and eosin staining. 10x10 |
4. Conclusions
- The obtained results of the experimental study of the soft tissues of the gingiva, after the introduction of various wound-healing substances in the form of collagen together with vitreous body and calcium gluconate testified to the enhancement of regenerative activity especially on days 7, 14. Soft tissue in this case was characterised by resorption of collagen and calcium gluconate replaced by scar tissue. Residual structures with basophilia in the form of clumps were also revealed. At collagen injection the regeneration processes were characterised by moderate organisation, and at vitreous body injection signs of encapsulation. Thus, the most optimal results of the experiment were observed in animals that were injected with collagen in vitreous body solution and were characterised by the development of delicate collagen fibres, which indicated the regenerative process at the site of drug injection.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML