-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1892-1896
doi:10.5923/j.ajmms.20241407.35
Received: Jul. 3, 2024; Accepted: Jul. 22, 2024; Published: Jul. 23, 2024

Tactics of Managing Women with Habitatal Loss of Pregnancy
Matrizaeva Gulnara Djumaniyazovna1, Ikhtiyarova Gulchekhra Akmalovna2
1Urgench Branch of Tashkent Medical Academy, Uzbekistan
2Bukhara State Medical Institute, Uzbekistan
Correspondence to: Matrizaeva Gulnara Djumaniyazovna, Urgench Branch of Tashkent Medical Academy, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Miscarriage is defined as spontaneous loss of pregnancy before 22 weeks of pregnancy. About 15-25% of pregnancies end in miscarriage, although miscarriage statistics vary greatly depending on the country and the timeliness of pregnancy diagnosis [1]. Pregnancy losses before 12 weeks of gestation (miscarriage, spontaneous abortion) account for 80% of all early reproductive losses. Miscarriages occurring before the thirteenth week of pregnancy are considered early miscarriage and from the fourteenth week onwards there is a decreasing risk of miscarriage. The probability of miscarriage between the third and sixth weeks is about 75%. By definition, habitual pregnancy loss is defined as the loss of two or more pregnancies [2]. Pregnancy loss is a common complication in early pregnancy. Data from a Scottish registry show that the prevalence of miscarriage is 5%. Other studies have shown a higher prevalence of pregnancy loss - from 10 to 15%. According to a population registry, 13.5% of pregnancies that were planned to be carried to term ended in fetal loss. Recurrent pregnancy loss is less common. Recurrent pregnancy loss is estimated to affect approximately 1% to 2% of women, defined as three consecutive pregnancy losses within 20 weeks of the last menstrual period [3].
Keywords: Gestation, Pregnancy, First trimester, Endometrium, Antibiotics
Cite this paper: Matrizaeva Gulnara Djumaniyazovna, Ikhtiyarova Gulchekhra Akmalovna, Tactics of Managing Women with Habitatal Loss of Pregnancy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1892-1896. doi: 10.5923/j.ajmms.20241407.35.
Article Outline
1. Introduction
- Recurrent pregnancy loss has a significant emotional impact on women and their partners. Pregnancy loss is a major negative life event, and the recurrent nature of recurrent pregnancy losses may increase the grief experienced. Genetic, endocrine, infectious, and anatomical factors are involved in the etiology, as well as autoantibodies, abnormal prothrombotic state, and other aspects. Endometrial receptivity can also be explained as the state of the endometrium that ensures adhesion, invasion, and implantation of the embryo. Endometrial and subendometrium hypoxia caused by inadequate blood flow induces slow receptivity, which reduces embryo implantation and increases the likelihood of spontaneous abortion. The woman's age is a risk factor and the likelihood of spontaneous abortion is high. About 7% of miscarriages occur among the ages of 25-29 and about 43% among the ages of 40-44. In those who have had three or more pregnancy losses, the risk of miscarriage is 20-70%, especially in the first trimester. In addition to age, a woman's environment may increase the risk of miscarriage. When a woman or her partner smokes, the risk of miscarriage is higher compared to a non-smoker. Chronic endometritis is characterized by plasma cell infiltration in the endometrium associated with a variety of pathogens. Several studies have suggested a prevalence of chronic endometritis in women with PPB of 7-58%. Antibiotics have been found to reduce the manifestations of endometritis and apparently improve live birth rates. However, this concept has not been tested in randomized controlled trials [4-10].Decidualization refers to the differentiation of resident stromal cells into specialized decidual cells that transform the endometrial mucosa into a tough, immunologically tolerant matrix necessary for trophoblast invasion and placement. Decidualization results in the appearance of not only progesterone-dependent, anti-inflammatory decidual cells, but also progesterone-independent senescent decidual cells. Senescent decidual cells, which secrete large amounts of inflammatory mediators and extracellular matrix proteases, participate in endometrial remodeling and its preparation for embryo implantation. They are subsequently cleared by activated uterine natural killer cells, a process that appears to be fundamental to the prevention of chronic sterile inflammation and the destruction of the developing maternal-fetal interface during pregnancy [11-16]. Endometrial receptivity is defined in the literature as the period of endometrial maturation during which the blastocyst trophectoderm can adhere to endometrial epithelial cells and subsequently invade the endometrial stroma and vasculature. Endometrial maturation is achieved in part by exposure to steroid hormones such as estrogen in the follicular phase and progesterone in the luteal phase. In the follicular phase, estrogen signals induce proliferation of the endometrial mucosa, leading to increased expression of progesterone receptors. Following ovulation, progesterone further alters the endometrium, creating an environment receptive to implantation and ultimately maintaining early pregnancy [3,1]. In addition to hormones, many molecular pathways including adhesion molecules, cytokines, and growth factors work in sync to create the implantation window. This implantation window is a short period of optimal endometrial receptivity and typically occurs between days twenty and twenty-four of a normal 28-day menstrual cycle. Not only are estrogen and progesterone levels important for implantation; their receptors also appear to play an important role in the process. Estrogen receptors exist in two forms: ERα and ERβ. Both are expressed in the endometrium, but they have different functions. Women with ERα have endometrial hypoplasia and are infertile. Thus, ERα appears to be essential for implantation. In contrast, women with ERβ have a normal endometrium and are fertile, suggesting that ERβ is involved in other aspects of endometrial function. During the proliferative phase, estrogen causes the progesterone receptor in endometrial cells to induce a response to progesterone during the luteal phase. As a negative feedback, progesterone inhibits ERα expression for proper endometrial function. The effects of progesterone in endometrial cells are mediated by the progesterone receptor. The effects of progesterone mediated by PR-A appear to be responsible for proper implantation, pregnancy, and parturition [2,17].Thus, for successful implantation, estrogen levels increase during follicular growth and are responsible for endometrial proliferation, myometrial thickness, and increased blood supply. Normal estradiol levels in early pregnancy may reflect the quality of the dominant follicle, corpus luteum function, and thereby help maintain the corpus luteum. In addition, estradiol appears to be an important factor in maintaining early pregnancy. A positive correlation was found between serum estradiol levels and gestational age in the fourth to eighth week of pregnancy. Serum estradiol levels are significantly lower in pregnant women with a history of abortion than in women with normal pregnancies. Progesterone deficiency and a shortened luteal phase may result in suboptimal endometrial development. On the other hand, it has been argued that progesterone deficiency is rather a manifestation of a previously insufficient follicular phase, which should be optimized in advance. While the effect of progesterone via endometrial thickness plays an important role in implantation and maintenance of pregnancy, progesterone supplementation in patients with sporadic miscarriage does not appear to improve pregnancy outcome. Progesterone therapy did not significantly increase live birth rates in women with threatened miscarriage overall, but women with early pregnancy loss and a history of previous miscarriages had higher live birth rates [18,7]. In view of this, estrogen plays a critical role in endometrial receptivity by initiating paracrine or autocrine signaling. Higher or lower estrogen levels in the periconceptional period result in lower pregnancy rates. Leukocytes are an important constituent of the human endometrium, accounting for 10% of stromal cells in the proliferative phase. Immediately before implantation, 20% of endometrial cells in the secretory phase are leukocytes, and in early pregnancy, leukocytes constitute 30% of decidual cells. The leukocyte population in the endometrium consists of T cells, macrophages, and large granular lymphocytes. T cells constitute 45% of leukocytes in the proliferative phase of the cycle. Their number remains constant throughout the menstrual cycle, although it decreases proportionally in relation to other types of leukocytes by the secretory phase of the cycle. Macrophages constitute a significant proportion of the leukocyte population of the human endometrium throughout the menstrual cycle [16,19].Given the above circumstances, women with habitual pregnancy loss should undergo a comprehensive study of the endometrium, biochemical and hormonal blood profile.
2. Research Objective
- To develop a pathogenetically substantiated algorithm for the comprehensive treatment of miscarriage based on the study of immunohistochemical markers of inflammation and endometrial receptivity.
3. Research Material and Methods
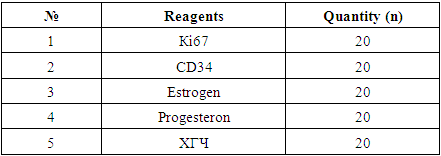
- To achieve this goal, a retrospective analysis of 382 case histories of patients observed in the gynecological departments of the Regional Perinatal Center of the Khorezm Region and the Urgench City Maternity Hospital from 2019 to 2022 was carried out. The diagnosis was made according to the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10). The study was conducted in women with miscarriage up to 13 weeks. The age of the patients ranged from 20 to 40 years, the average age was 23 years, all women were married, and the average age at marriage was 21.9 ± 0.28. Retrospectively, the medical history was carefully studied and the following data were found: history of somatic, gynecological and obstetric pathologies. A prospective observational comparative controlled study was performed in 258 women with habitual miscarriage. The first group included 198 women with habitual miscarriage. The control group consisted of 60 healthy fertile women with no history of miscarriage, with a full-term birth through the birth canal in the history, without deviation from the physiological course of pregnancy and the act of birth, as a result of which healthy children were born. For the second stage of the study, the main group was divided into two subgroups: Group 1 (n = 100): formed from patients who subsequently received a personalized, comprehensive examination and preconception preparation, Group II (n = 98) - from patients who subsequently received a generally accepted volume of diagnostics and treatment. Inclusion criteria: Reproductive age from 18 to 45 years; 2 or more miscarriages in the anamnesis; miscarriage associated with inflammatory diseases of the pelvic organs, hormonal disorders, immunological and hemostatic disorders; history of normal pregnancy and childbirth; pregnancy at the time of participation in the study; history of miscarriage, non-viable pregnancy, and, if there has been childbirth, a physiological term birth with the birth of heavy or stillborn children; history of infertility; no history of miscarriage, non-viable pregnancy, and, if there has been childbirth, a physiological term birth with the birth of healthy children; absence of chronic gynecological and somatic pathology in the acute stage; informed voluntary consent to participate in the study. Exclusion criteria: woman's age under 18 and over 45 years; male factor; alloimmune miscarriage (healthy husband and wife); uterine anomalies, intrauterine pathology (Asherman syndrome); multiple and symptomatic uterine fibroids of large sizes, external genital endometriosis and adenomyosis; concomitant gynecological and somatic pathologies in patients requiring medication at the time of participation in the study; the presence of chromosomal pathologies; an increase in the body mass index (BMI) of 34.5 or more; chronic gynecological and somatic pathologies in the acute stage; presence of oncological pathologies in the anamnesis; lack of informed voluntary consent to participate in the study or refusal at any stage of the work (for patients of all groups).The diagnosis of early miscarriage was made by vaginal ultrasound during the first trimester examination or after abdominal symptoms or vaginal bleeding. On imaging, the absence of motor activity and heartbeat, as well as the discrepancy between the embryo size and the estimated gestational age according to the last menstrual date, were the criteria for the diagnosis of non-viable pregnancy. Patients with miscarriage up to 12 weeks were included in the study. In accordance with the management policy at our institution, each patient was fully informed and counseled about the two options for miscarriage management: medical treatment (misoprostol) and dilation and curettage, after which a specific consent form was provided and signed, which selected the medical or surgical approach according to individual preference. Patients who had complications with miscarriage, including heavy uterine bleeding (resulting in the need for blood transfusion), uterine perforation, fever, and the need for surgical hysteroscopy to remove retained products of conception, were excluded.Immunohistochemistry was performed at the RIO and RIATM Pathomorphology Department. Uterine scrapings were collected at the Perinatal Center of the Khorezm Region in the Gynecology Department from women with miscarriage after miscarriage in the period 2021-2023.Among the examined women, the frequency of NB in the anamnesis ranged from 1 to 8 cases, the average number was 2.1±0.02 cases.Directly, scrapings from the uterine cavity (n=40), including decidual tissue of the endometrium, served as the material for the morphological study. The comparison group consisted of a biological substrate obtained from women who decided to terminate an uncomplicated pregnancy at 5-12 weeks by artificial abortion (n=20). The main group included scrapings from patients suffering from habitual miscarriage in the early stages of various etiologies (main group, n=40).The gestational age was determined by the first day of the last menstruation.The results of the morphological examination are currently recognized as the gold standard worldwide. All patients who received histological cassettes taken from the incision were processed for immunohistochemical examination. The radio transmission of the Bond Leica Australia immune processor (Australia) was used for the study; Ki67, CD34, estrogen and progesterone receptors, and XGCH monoclonal antibody were determined.
|
4. Results of the Study
- Based on the full analysis of the patient's medical history, it was found that the patients with miscarriage were mainly urban residents who accounted for 232 (61%) women and 150 (39%) rural residents.The social status of the patients depending on the activity of women was distributed as follows: the main part was housewives 251 (65.7%), civil servants accounted for 105 (27.5%) women, and insignificant percentages were students, entrepreneurs and workers who respectively accounted for 1.6%; 1%; 2.1%.In our retrospective analysis, when patients came to the hospital, all women had their blood group and Rh factor, and it was especially noteworthy that 157 (41%) women had the first blood group, 82 (21.5%) had the second blood group, 101 (26.4%) had the third blood group, and 42 (11%) had the fourth blood group. The Rh factor was positive in 362 (94.8%) and negative in 20 (5.2%) women, and all women with Rh negative blood were given anti-Rhesus D immunoglobulin after a miscarriage.When studying the somatic pathology of patients with early miscarriage, endocrine pathology was more often observed. Among the endocrine diseases, thyroid pathology prevailed in the form of hypothyroidism, which amounted to 217 (56.8%), hyperthyroidism in 17 (4.5%), autoimmune thyroiditis 83 (21.7%), metabolic syndromes such as insulin resistance 89 (23.3%), obesity 78 (20.4%), prediabetes 16 (4.2%), as well as hyperandrogenism, hyperprolactinemia 12 (3.1%). An analysis of extragenital diseases was also performed, where the presence of cardiovascular disease was assessed such as: arterial hypertension was observed in 33 (8.6%) women, varicose veins in 104 (27.2%) women; diseases of the urinary tract and kidneys: the most common among patients was chronic pyelonephritis in 94 (24.6%) and chronic cystitis in 27 (7.06%); respiratory organs (chronic tonsillitis) in 63 (16.5%) and diseases of the gastrointestinal tract. Also, when analyzing extragenital pathology, systemic diseases were identified in 53 (13.87%) cases. Taking this into account, we can say about the timely detection of pathology, taking into account regular visits to a general practitioner, timely detection and treatment of this pathology. And for women with further pregnancy planning, also conduct pre-gravid preparation taking into account the anamnesis, hereditary diseases and extragenital pathology. In addition, patients with miscarriage were characterized by a high level of gynecological morbidity and a complicated obstetric history. Inflammatory diseases of the uterus and appendages were noted in 231 (60.5%) women, abnormal uterine bleeding in 18 (4.7%) women, uterine fibroids up to 15 mm in size according to ultrasound in 22 (5.7%) women, adenomyosis in 62 (16.2%) women, missed abortions in 12 (25.0%), spontaneous abortions in 7 (14.5%), abortions in 13 (27.0%), and premature births in 6 (12.5%). Complications and consequences of abortions lead to reproductive health disorders, increased levels of reproductive losses and in 25% of cases to infertility. It should be noted that the level of gynecological pathology was high, especially in those who had 3 or more miscarriages, and the main percentage was inflammatory diseases of the pelvic organs, which indicates the importance of preventing abortions and infections. Thus, according to the data we obtained, it was found that the level of somatic pathology in patients with miscarriage more than 3 times was 1.5 times higher. The frequency of gynecological morbidity: diseases of the uterus and appendages by 2.1 times, uterine fibroids by 3.0 times, endometriosis by 4.6 times, frozen pregnancies by 3.8 times, spontaneous abortions by 2.2 times, abortions by 2.7 times, in these women it is 2.3 times more than in women with miscarriage by 2 times, which, of course, indicates the influence of extragenital pathology and gynecological morbidity on the formation of infertility and the importance of preventing abortions, inflammatory diseases starting from adolescence. Prevention of the impact of extragenital pathology and gynecological diseases on fertility consists of early diagnosis of possible chronic diseases and adequate treatment long before planning pregnancy.
5. Conclusions
- The identified changes require further study of the problem by pathologists, obstetricians-gynecologists, immunologists to determine the pathomorphological mechanisms of the development of non-developing pregnancy in each couple. This will allow obstetricians-gynecologists to be guided in a detailed examination of the couple and to carry out comprehensive prevention of miscarriage.The results of the studies made it possible to establish new links in the pathogenesis of miscarriage in case of intrauterine infection.Immunohistochemistry allows for more accurate diagnosis and monitoring of the effectiveness of hormonal treatment, provides an individual approach to the patient and, therefore, allows optimizing hormonal therapy regimens.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML