Askarova Zebo Zafarjonovna1, Kurbaniyazova Madina Zafarjanovna2
1Associate Professor of the Department of Obstetrics and Gynecology No. 1 Samarkand State Medical University, Uzbekistan
2Senior Lecturer of the Department of Obstetrics and Gynecology Urgench Branch of Tashkent Medical Academy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
In recent years, attention has been drawn to the increasing incidence of Benign Breast Dysplasia (BBD) in patients with gynecological pathology [1,4]. In this case, hyperplastic processes of the internal genital organs (uterine myoma, endometrial hyperplasia, endometriosis) are most often detected in patients with breast pathology [5,8]. The frequent combination of hyperplastic diseases of the uterus and mammary glands is due to the presence of identical risk factors for these diseases, increased proliferative activity of cells, intense expression of growth factors, decreased apoptosis, and activation of the neoangiogenesis process [7,12].
Keywords:
Hyperplastic processes, Gynecology, Respiratory movements, Ultrasound systems, Tissue compression, Myometrial hyperplasia
Cite this paper: Askarova Zebo Zafarjonovna, Kurbaniyazova Madina Zafarjanovna, The Importance of Ultrasound Diagnostics and Elastography in the Diagnosis and Management of Women with Hyperplastic Processes of the Endo- and/or Myometrium in Combination with Diseases of the Mammary Glands, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1885-1891. doi: 10.5923/j.ajmms.20241407.34.
1. Introduction
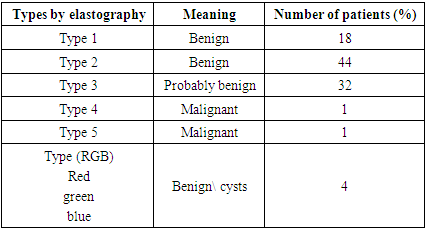
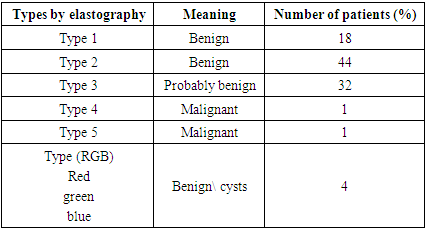
The combination of pathological processes in the endo-myometrium and mammary glands was detected in 76-97.8%. In general, data on the total frequency of hyperplastic diseases remain debatable, as does the question of the priority of pathological changes in these target organs [13]. According to some authors [5], the most severe forms of DDMZ are formed in women with uterine myoma, adenomyosis, hyperplastic processes of the uterus. Other researchers suggest considering the priority of damage to the mammary glands as a marker of developing uniform disorders in the reproductive system [7].Ultrasound examination (US) of the pelvic organs and mammary glands is the most common of all instrumental methods of examination in gynecology. Like any additional stage in the diagnostic algorithm, echography should be performed after collecting anamnesis and clinical gynecological examination [12].Elastography of the mammary gland can significantly improve the capabilities of the ultrasound scanner and differentiate benign and malignant tumors of the mammary gland - thereby reducing the number of biopsies. Elastography helps to assess the rigidity of tissues and the density of the neoplasm of the affected area by comparing the stress in tissue elements subject to external compression.Elastography has several technological options. In our work we used two main technical methods: compression elastography (SE) and shear wave elastography (SWE), the latter including elastography of the ultrasound force impulse (acoustic radiation force impulse, ARFI) and supersonic shear-wave imaging, SSI, which is considered one of the methods of (ARFI) technology.The compression method (SE) is based on the use of the method of compression of breast tissue and measurement of the deforming effect, calculating the values of local damage by stiffness in comparison with the surrounding tissues. Small compression / decompression by hand is applied using a conventional sensor or deformation can be obtained using respiratory movements."The technique allows to obtain only qualitative and semi-quantitative assessments of the damage, since the force of manual compression is unknown, which allows only the calculation of the deformation ratio, and not the absolute elasticity of the tissues" [9]. The shear wave elastography (SWE) method is possible because shear waves are ubiquitous and occur frequently in human soft tissue. Shear waves are transverse, they attenuate rapidly, travel much more slowly (1 to 10 m/s) and are not supported by low viscosity fluid. Shear waves are produced by any mechanical action and occur naturally in muscle movements, as well as being induced in ultrasound systems used to measure tissue elasticity. The SWE method has the advantage that the system "moves" the tissue itself and does not require tissue compression, providing quantitative information. Elastography can add important details to the examination, to identify lesions in epithelial and connective tissue, to determine their stiffness and elasticity. Localized benign disease usually appears as hypoechoic or anechoic structures, often regular in shape and with clear borders. These nodules are usually round or oval in shape, located parallel to the chest wall."The structure of the lesion is often homogeneous, with a large variability in echogenicity. Vascularity is variable and depends on the nodule histology. Generally, benign lesions are firmer than normal breast tissue, but softer than malignant tumors. Exceptions may be in cases of benign lesions such as hyalinized fibroadenomas and fat necrosis, which may be difficult to palpate and may lead to false elastography results [1,6]. Benign lesions are marked in ultrasound elastography in a light color in the color map, quantitatively 1-2 points, while the best point for differentiating benign and malignant tumors is 3-4 points at the border in the color map according to the Ueno-Itoh classification. Cysts often appear as solid and low deformable lesions, usually presented as a pattern on the blue color map and with a high degree of deformation due to their low compressibility.Success in obtaining maximum information from ultrasound depends on knowledge of the anatomy and physiology of the female body, since the size and structure of the uterus and ovaries depend on age, day of the menstrual cycle or duration of the postmenopausal period. Without taking these factors into account, it is impossible to solve the first task facing the ultrasound diagnostics doctor [3,4,8].
2. The Purpose of Our Study
To study the diagnostic value of ultrasound diagnostics in the management of women with hyperplastic processes of the uterus and mammary glands.
3. Materials and Methods of Research
Taking into account the set goal, we examined 220 perimenopausal patients with hyperplastic processes of the endo and / or myometrium, who were treated in the gynecological department of the multidisciplinary clinic of the Samara State Medical University for the period from 2022 to 2024.The examined women were divided into three groups: Group 1 - 120 patients with a verified diagnosis of endometrial and/or myometrial hyperplasia during perimenopause, who underwent a thorough examination of the mammary glands, during which no pathology was detected. Group 2 - 100 patients in the perimenopause period who were diagnosed with endo- and/or myometrial hyperplasia and benign diseases of the mammary gland. Group 3 - 90 women in the perimenopause period without gynecological diseases.The age of the examined ranged from 43 to 51 years, on average, was 46.9 ± 1.6 years.
4. Results
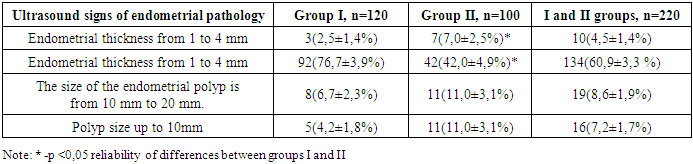
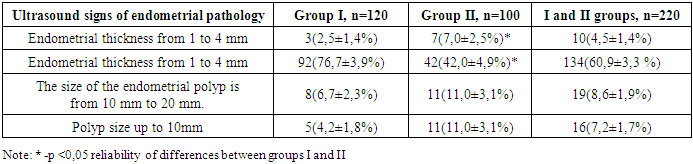
Patients with hyperplastic processes of the endo- and/or myometrium applied to the gynecological department of the 1st clinic of the Samarkand Medical University. When analyzing the complaints of patients in both main groups, it was found that upon admission to the clinic, bloody discharge of varying intensity was noted by the majority of those examined - 78 (65 ± 4.3%) patients in Group I and 70 (70 ± 4.6%) in Group II. The average duration of bloody discharge before admission to the hospital was 22.6 ± 3.6 days in Group I and 35.1 ± 3.6 days in Group II. An important stage of the examination was transvaginal scanning of the pelvic organs both before diagnostic hysteroscopy (HSC) and curettage of the uterine cavity, and after the operation during treatment and dynamic observation.During the ultrasound examination, the size of the uterus, structural features of the myometrium, endometrium, ovaries were assessed, special attention was paid to the structure, echogenicity and size of the median uterine echo (P50 P25 P75).Given the impossibility of performing ultrasound examination (US) for all patients according to standards in the 1st phase of the cycle, the ultrasound was performed against the background of a delay in menstruation, against the background of bleeding and immediately after bleeding.When analyzing the cycle irregularities, it was revealed that upon admission to the clinic, bleeding lasting from 26 to 45 days was observed in 90 (60.8±4.0%) patients of the main group (Table 1).Table 1. Number of patients with ultrasound signs of endometrial pathology, M±m
 |
| |
|
A delay of menstruation from 30 to 65 days was noted in 44 (61.1 ± 5.7%).All patients underwent ultrasound to assess the state of the endo- and myometrium.M-echo in patients with bleeding varied from 1 to 15 mm, on average in Group I it was 10.96 ± 5.6 mm, in Group II - 11.7 ± 4.5 mm.In 90 (60.8 ± 4.0%) of 148 with bleeding, M-echo varied from 7 to 20 mm, in 17 (11.4 ± 2.6%) endometrial polyp was diagnosed. M-echo in 44 (61.1±5.7%) patients with a delay in menstruation ranged from 10 to 20 mm, averaging 16.0±3.7 mm, in 18 (23.0±4.9%), an endometrial polyp was detected on ultrasound, and in the remaining 10 (13.9±4.0%), endometrial atrophy ranged from 1 to 4 mm.When examining the ultrasound signs of endometrial pathology (Table 2) by groups, the following was revealed: endometrial thickness from 1 to 4 mm was 3 times more common in the group with GGPM and DDMZ compared to its frequency in group I, (p < 0.05). Only 3 (2.5 ± 1.4%) patients in the main group had a thin endometrium. There were significant differences between groups I and II in the number of patients with endometrial thickness from 7 to 20 mm - 92 (76.7 ± 3.9%) and 42 (42.0 ± 4.9%), respectively, (p < 0.05).Table 2. Ultrasound signs of endometrial pathology, M±m
 |
| |
|
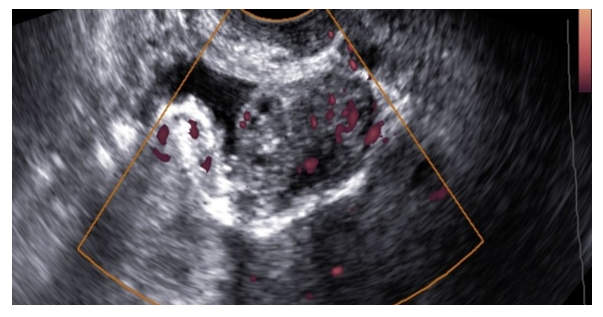
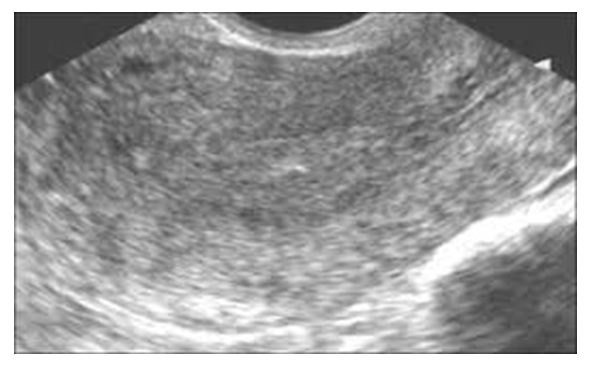
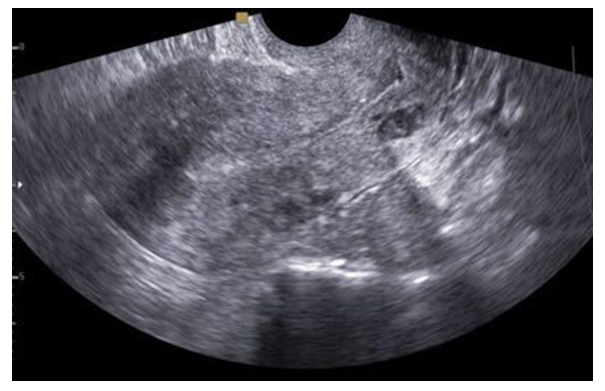
Endometrial polyps in groups I and II were observed in 13 (10.8 ± 2.8%) and 22 (22.0 ± 4.1%) patients, which was significantly more common in group II compared to group I. | Picture 1. Ultrasound image of glandular cystic hyperplasia of the endometrium |
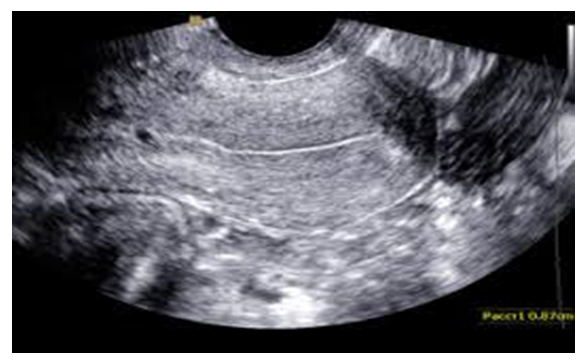
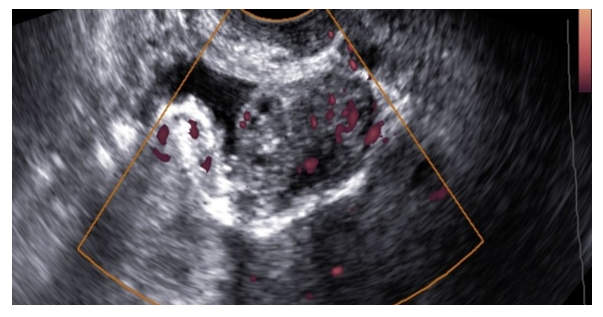
 | Picture 2. Ultrasound image of endometrial hyperplasia |
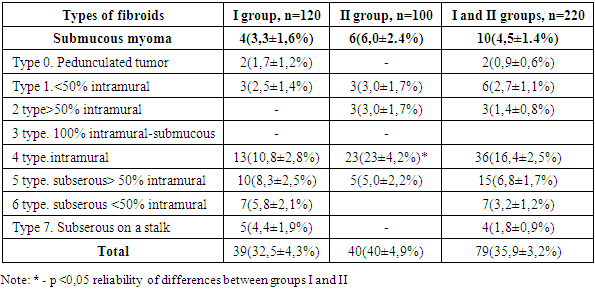
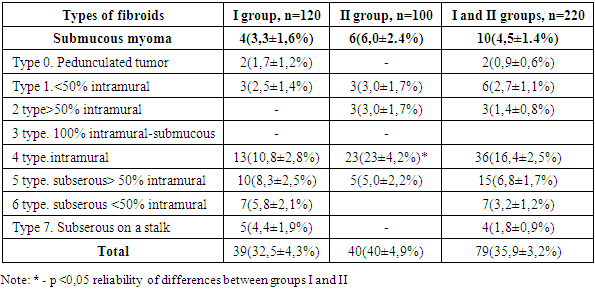
Among patients with GPPM, every third patient - 39 (32.5±4.3%) - had various types of uterine myoma detected by ultrasound. The detected types of uterine myoma were distributed according to the FIGO classification (Table 3). The frequency of myomas did not differ by group, except that the intramural type of myoma was significantly more often diagnosed by ultrasound in patients of group II - 13 (10.8±2.8%) versus 23 (23±4.2%) in group I, p<0.05.Table 3. Distribution of patients with myomas according to FIGO classification, M±m
 |
| |
|
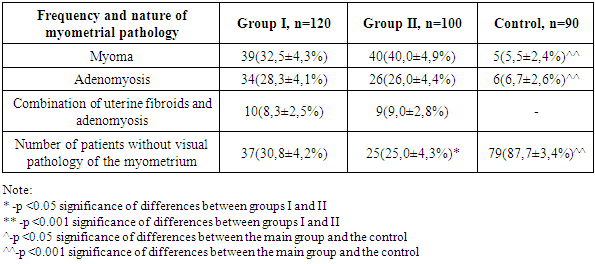
In this case, the size of the largest node was 31 mm in diameter, the average size of the myomatous node in both groups was 17.0 (12.0-20.0) mm. The features of the ultrasound picture of the myometrium were also studied (Table 4).Table 4. Frequency of echographic signs of myometrial pathology, M±m
 |
| |
|
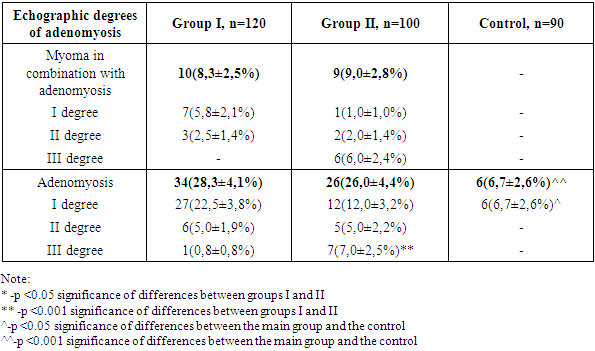
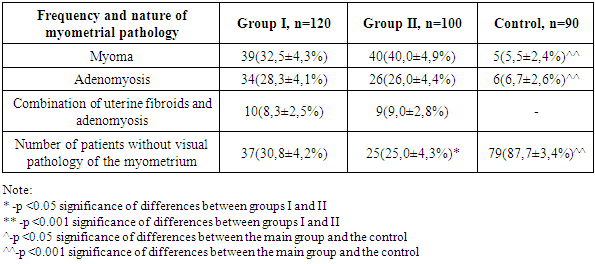
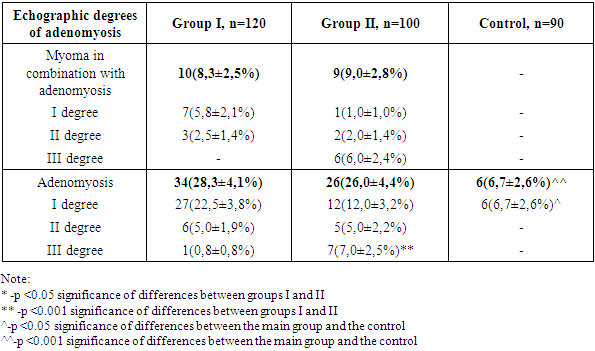
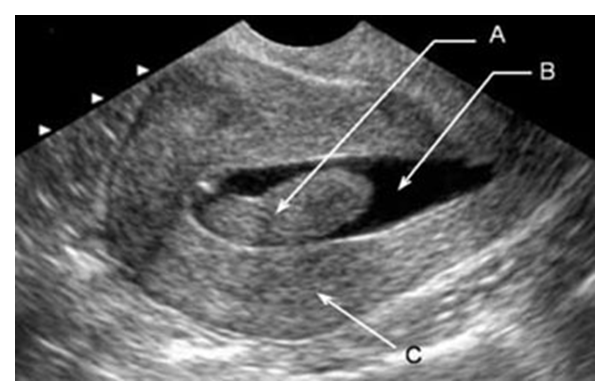
The structure of myometrial pathology according to ultrasound data is presented in Table 4. As can be seen from the table, the most frequent myometrial pathology was uterine myoma 39 (32.5±4.3%) and 40 (40.0±4.9%) among patients in groups I and II versus 5 (5.5±2.4%) in the control, p<0.001. The second most frequent pathology was adenomyosis - 34 (28.3±4.1%) and 26 (26.0±4.4%) among patients in groups I and II versus 6 (6.7±2.6%) in the control, p<0.001. A combination of uterine myoma and adenomyosis was observed in 19 patients. In addition, it should be noted that only every third patient with GPPM and every fourth patient with GPPM and DDMZ in perimenopause were not diagnosed with myometrial pathology - 37 (30.8±4.2%) and 25 (25.0±4.3%), while in the control group there were an overwhelming majority of such - 79 (87.7±3.4%), p<0.001.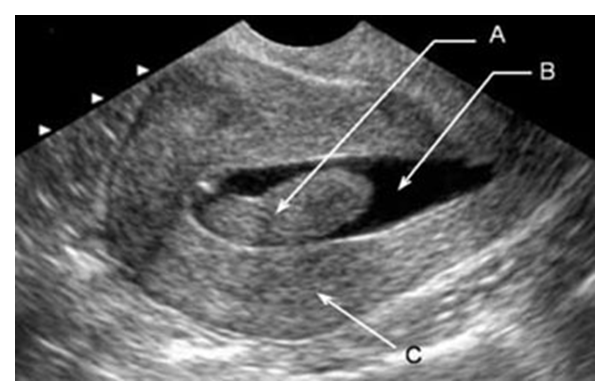 | Picture 3. Ultrasound image of endometrial polyp |
 | Picture 4. Ultrasound image of a submucous myomatous node |
Table 5. Echographic degrees of adenomyosis, M±m
 |
| |
|
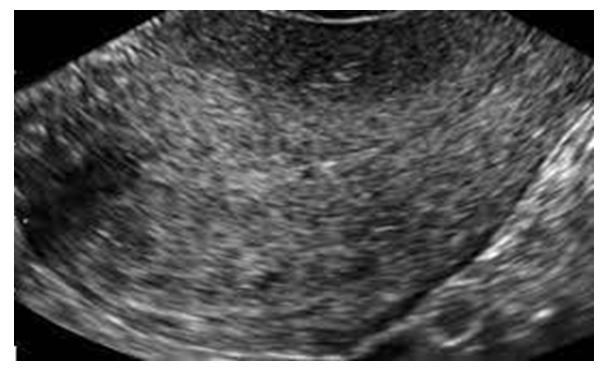
Adenomyosis in combination with uterine myoma was echographically detected in 10 (8.3±2.5%) patients of group I and in 9 (9.0±2.8%) patients of group II. Adenomyosis was detected in 34 (28.3±4.1%) patients of group I and in 26 (26.0±4.4%) patients of group II. It should be noted that the degree of adenomyosis was significantly more common in patients with GPPM and DDMZ - 7 (7.0±2.5%), p<0.001.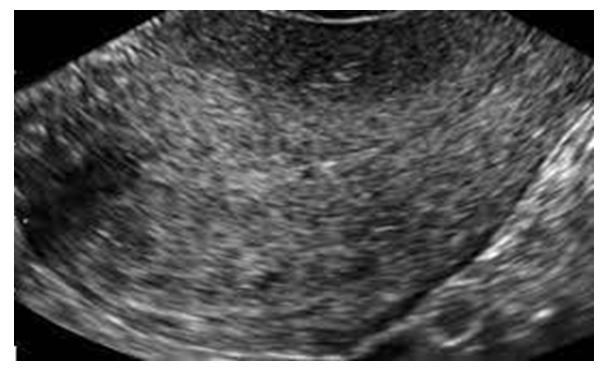 | Picture 5. Echo picture of stage I adenomyosis |
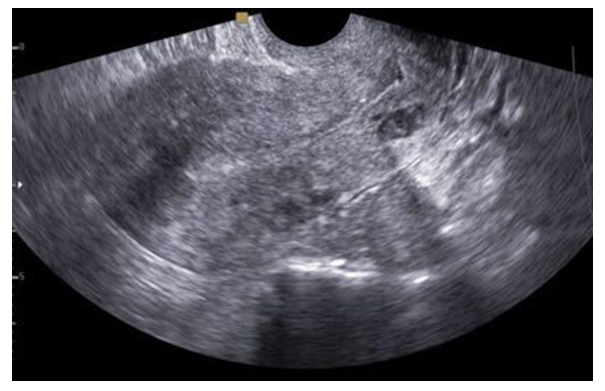 | Picture 6. Echo picture of stage II adenomyosis |
 | Picture 7. Echo picture of stage III adenomyosis |
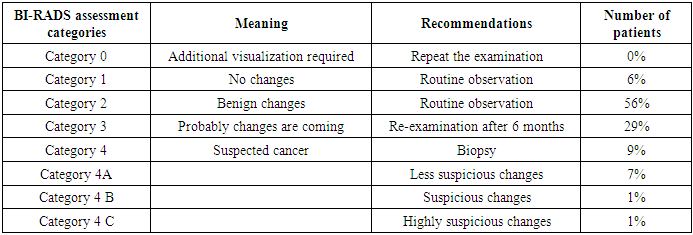
Ultrasound assessment of the condition of the mammary glands was performed using the Aplio 500 ultrasound machine (Toshiba) with a linear sensor, with a frequency of 7.5 MHz. The structure of the tissues of the mammary glands was assessed echographically - the ratio of fat, glandular and fibrous components. Thickening and unevenness of the walls, pocket-like expansion of the lumen of the ducts, echogenicity of the parenchyma were recorded. The presence of echographically changed areas, their size, echogenicity, boundaries, localization were determined. If volumetric formations were detected, the structure of the contents, wall thickness and the presence of parietal formations were assessed. The examination was completed by studying the regional zones of lymph outflow in the axillary, subclavian, parasternal regions, the size, structure and localization of the lymph nodes were assessed. Table 6. Mammographic findings were assessed according to the BI-RADS assessment category BI-RADS assessment categories of mammographic findings
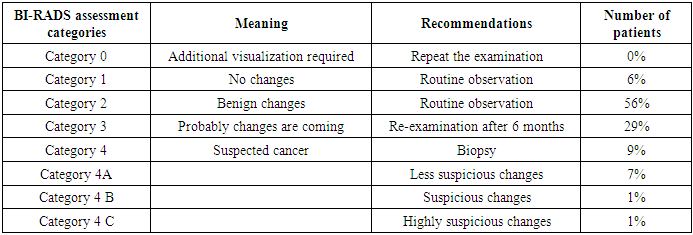 |
| |
|
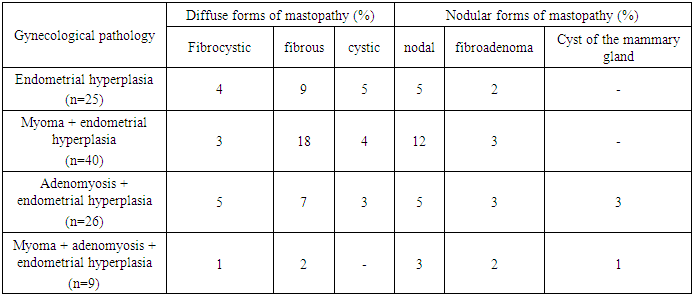
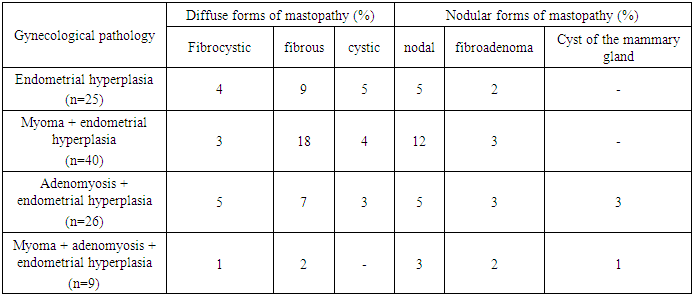
During the echography of patients with hyperplastic processes of the uterus and mammary glands according to the BI-RADS category, it was revealed that the echographic criteria corresponded to category 2 in 56% of patients. In 29% of patients, the echo picture corresponded to category 3 and 9% corresponded to category 4. Patients who corresponded to category 4 according to the BI-RADS category were referred to an oncologist for further examination.The correlation dependence of mammological pathology depending on the types of hyperplastic processes of the endo- and/or myometrium was studied (Table 7).Table 7. Distribution of patients with hyperplastic processes of the endo- and/or myometrium in accordance with the identified mammological pathology
 |
| |
|
In endometrial hyperplasia without myometrial pathology, diffuse fibrous mastopathy was mainly detected - 9%. In patients with uterine myoma combined with endometrial hyperplasia, diffuse fibrous mastopathy was also often detected - 18%. Patients with adenomyosis and GPE were also often detected fibrous mastopathy, but unlike other patients, they often had a breast cyst - 3%. In patients without adenomyosis, breast cysts were not observed.Table 8. Elastography of the mammary glands
 |
| |
|
Thus, when comparing the ultrasound results in the two groups, there is a statistically significant difference in the structure of the myometrium, endometrium, and mammary glands.The analysis of complaints of patients with hyperplastic processes of the uterus and DDM, gynecological status, ultrasound data, showed that the selected groups are comparable in the following indicators:• almost half of the patients with GPPM complained of heavy and prolonged uterine bleeding and eight times more often indicated pain in the lower abdomen compared to the control group;• during an ultrasound examination of the endometrial thickness in patients with GPPM, a thin endometrium was significantly more often observed in the group with GPPM in combination with DDM;• in every third patient with GPPM, uterine fibroids were detected during an ultrasound examination. The intramural type of fibroids was significantly more common in patients with a combination of DDM; • During echography of patients with hyperplastic processes of the uterus and mammary glands according to the BI-RADS category, it was revealed that the echographic criteria mainly corresponded to category 2 - 56%. In 29% of patients, the echo picture corresponded to category 3 and 9% corresponded to category 4. Patients who corresponded to category 4 according to the BI-RADS category were referred to an oncologist for further examination.• Unlike other patients, patients with adenomyosis often had a breast cyst - 3%. In patients without adenomyosis, breast cysts were not observed.Thus, ultrasound diagnostics of hyperplastic processes of the endo- and / or myometrium and benign dysplasia of the mammary glands is the most effective examination method, which gives us the opportunity to make a correct diagnosis, determine the degree of damage to the organ and the body, which makes it possible to choose the right tactics for managing the disease and prevent relapses and malignancy.
References
| [1] | Alieva, A.S. Endometrial ablation in hyperplastic processes in perimenopausal women: diss. ... candidate of medical sciences / A.S. Alieva. - M., 2018. -121 pages. |
| [2] | Askarova Z. Z., Aliyeva D. A., Kurbaniyazova M. Z. BREAST CONDITION IN WOMEN WITH ENDOMETRIAL HYPERPLASIA DURING THE PERIMENOPAUSE // Studies. – Т. 6. – С. 12. |
| [3] | Askarova Z. Z., Alieva D. A., Kurbaniyazova M. Z. IMPROVING EXAMINATION METHODS FOR PATIENTS WITH ABNORMAL UTERINE BLEEDING IN PERIMENOPAUSAL WOMEN //Euro-Asia Conferences. – 2021. – Т. 1. – №. 1. – С. 148-151. |
| [4] | ASKAROVA Z. Z., KURBANIYAZOVA M. Z. The Value of Genetic Research of Women with Abnormal Perimenopausal Bleeding. – 2020. |
| [5] | Курбаниязова М. З. и др. БЕРЕМЕННОСТЬ И ЗАБОЛЕВАНИЯ ШЕЙКИ МАТКИ: ЧАСТОТА, ОСЛОЖНЕНИЯ ГЕСТАЦИИ // МИНИСТЕРСТВО ЗДРАВООХРАНЕНИЯ РЕСПУБЛИКИ УЗБЕКИСТАН РЕСПУБЛИКАНСКИЙ СПЕЦИАЛИЗИРОВАННЫЙ НАУЧНО-ПРАКТИЧЕСКИЙ МЕДИЦИНСКИЙ ЦЕНТР АКУШЕРСТВА И ГИНЕКОЛОГИИ АССОЦИАЦИЯ ВРАЧЕЙ ЧАСТНОЙ ПРАКТИКИ УЗБЕКИСТАНА КЛИНИКА «MAHLIYO-SHIFO» & V «MAHLIYO-SHIFO» & V. – С. 55. |
| [6] | Askarova, Z.Z., Saparbayeva, N.R., Kurbaniyazova, M.Z. and Aliyeva, D.A., 2021. VALUE OF HYSTEROSCOPY AND GENETIC RESEARCH OF WOMEN WITH ABNORMAL UTERINE BLEEDING IN PERIMENOPAUSE. Eur J Mol Clin Med, 8(1), pp.409-416. |
| [7] | Bershtein L.M., Ievleva A.G., Mukhina M.S. The relationship between hormone-associated properties and plasticity of omental fat with clinical and morphological features of endometrial cancer in patients with different obesity phenotypes // Issues of oncology. - 2016. - N 1. - P. 79-84. |
| [8] | Benign breast dysplasia: clinical guidelines / Russian Society of Obstetricians and Gynecologists, All-Russian Public Organization "Russian Society of Oncomammologists", Russian Association of Mammologists LLC, All-Russian Public Organization "Russian Society of Specialists in the Prevention and Treatment of Tumors of the Reproductive System". 2020. |
| [9] | Eseneeva F.M., Shalaev O.N., Orazmuradov A.A., Radzinsky V.E., Kiselev V.I., Salimova L.Ya. The influence of epigenetic processes on the expression of steroid receptor genes in uterine fibroids. // Difficult patient No. 1-2. Vol. 15. 2017. P. 23-26. |
| [10] | Trubnikova L.I., Voznesenskaya N.V., Tadzhieva V.D., Kornilova T.Yu., Albutova M.L., Tikhonova N.Yu. // Current issues of gynecology. Tutorial. Ulyanovsk - 2019. 266 p. |
| [11] | Todzhieva N.I., Khudoyarova D.R., Bazarova Z.Z. Improving methods for treating endometrial hyperplastic processes in premenopause - Professional of the Year. 2018. 81-84 p. |
| [12] | Grady D. Clinical practice management of menopausal symptoms. N Engl J Med. 2018; 355: 2338-2347. |
| [13] | Goldstein SR, Lumsden M.A. Abnormal uterine bleeding in perimenopause. Climacteric. 2017; 414-420. 9. Rivard A. B., Galarza-Paez L., Peterson D. C. Anatomy, Thorax, Breast / StatPearls. 2022. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML