-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1880-1884
doi:10.5923/j.ajmms.20241407.33
Received: Jun. 29, 2024; Accepted: Jul. 20, 2024; Published: Jul. 22, 2024

Efficiency of Telemedicine in Assessing the Detection of Primary Open-Angle Glaucoma
Djamolova Shirin1, Asadov Diyor2
1Doctor of Medical Sciences, Associate Professor, Republican Specialized Scientific and Practical Medical Center of Eye Microsurgery, Tashkent, Uzbekistan
2Independent PhD Researcher, Republican Specialized Scientific and Practical Medical Center of Eye Microsurgery, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

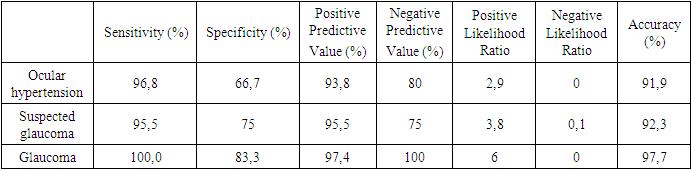
Objective: To evaluate the effectiveness of telemedicine in the primary detection of primary open-angle glaucoma (POAG). Methods: The study aimed to assess the effectiveness of telemedicine in diagnosing and treating POAG. The research design was based on comparing the results of teleconsultations and in-person ophthalmological examinations in the same sample of patients with suspected or confirmed POAG. The comparison of both types of examinations was conducted, and specific statistical indicators were calculated. Results: In detecting confirmed cases of POAG, sensitivity was 100%, specificity was 83.3%, positive predictive value was 97.4%, negative predictive value was 100%, positive likelihood ratio was 6, negative likelihood ratio was 0, and accuracy was 97.7%. Conclusion: The high sensitivity and specificity of remote consultations allow for the effective identification of patients with this disease and taking appropriate measures for further treatment and monitoring.
Keywords: Glaucoma, Primary open-angle glaucoma, Telemedicine
Cite this paper: Djamolova Shirin, Asadov Diyor, Efficiency of Telemedicine in Assessing the Detection of Primary Open-Angle Glaucoma, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1880-1884. doi: 10.5923/j.ajmms.20241407.33.
1. Introduction
- Glaucoma requires early detection, careful monitoring of intraocular pressure, assessment of the optic nerve condition and visual fields, and control and correction of medication therapy [1,4,5]. One of the key obstacles for patients with glaucoma can be the lack or remoteness of specialized ophthalmological facilities and qualified specialists [2,3,7]. Telemedicine for glaucoma screening offers many potential benefits. In developed countries, where the number of patients is high and there is a shortage of qualified glaucoma specialists, telemedicine can significantly reduce the number of unnecessary doctor visits [1,6,8,9]. Studies evaluating the effectiveness of remote interactions between local optometrists and ophthalmologists based on remote visualization of the optic nerve disc and assessment of visual fields confirm that screening patients at risk for glaucoma can reduce the rate of false referrals to specialists [2,10,11]. Thus, telemedicine is an effective solution to this problem.Objective. To study the effectiveness of telemedicine in the primary detection of primary open-angle glaucoma (POAG).
2. Materials and Methods
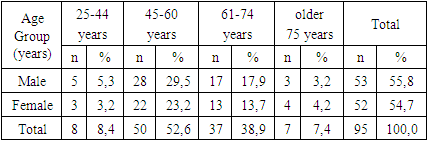
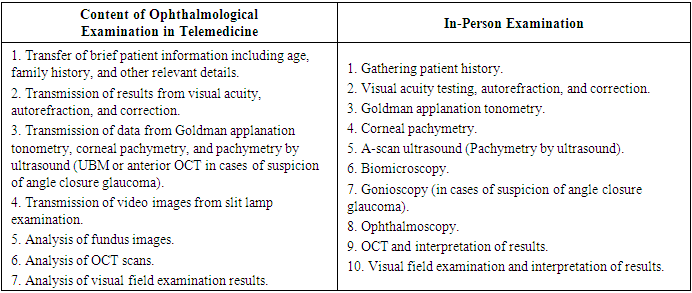
- The study was conducted from 2021 to 2023 at the Republican Specialized Scientific and Practical Medical Center of Eye Microsurgery and its regional branches. To achieve the study's objective, it was necessary to assess the effectiveness of using telemedicine in diagnosing and treating POAG. The main study design was based on comparing the results of teleconsultations and in-person ophthalmological examinations in the same sample of patients with suspected or confirmed POAG. The comparison involved evaluating the results of both types of examinations and calculating specific statistical indicators.The study included two main stages: the stage of assessing the effectiveness of telemedicine in POAG screening and the stage of assessing the effectiveness of telemedicine in POAG monitoring. In the first stage, a study of suspected glaucoma cases was conducted, where patients with initially detected signs of increased intraocular pressure and glaucomatous changes in the optic nerve head underwent two types of ophthalmological examinations: teleconsultation and in-person examination. In the second stage, the effectiveness of the two examination methods in monitoring glaucoma was compared, assessing POAG progression, criteria for changing medication therapy, indications for laser treatment, indications for surgery, and the effectiveness of surgery.The study included clinical cases of suspected POAG, involving individuals over 40 years old with increased intraocular pressure and/or glaucomatous changes in the optic nerve head. Another inclusion criterion was the patient's informed consent to participate in the study. Age and gender distribution of patients in the first and second stages of the study are presented in Table 1.
|
3. Results
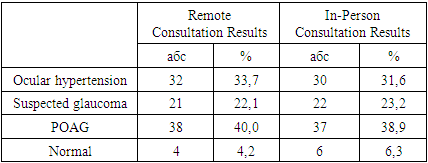
- The results of assessing suspected glaucoma cases using remote and in-person consultations are presented as absolute values and percentages (Table 2). Remote consultation identified 32 cases (33.7%) of ocular hypertension, compared to 30 cases (31.6%) identified during in-person consultation. Suspected POAG was identified in 21 cases (22.1%) through remote consultation, while 22 cases (23.2%) were identified in in-person consultations. Confirmed POAG cases were found in 38 cases (40.0%) through remote consultation, compared to 37 cases (38.9%) in in-person consultations. Normal findings were confirmed in 4 cases (4.2%) through remote consultation, whereas 6 cases (6.3%) were confirmed during in-person consultations. These data indicate that remote and in-person consultations generally show comparable results in identifying suspected glaucoma cases. The majority of suspected glaucoma cases were confirmed as POAG in both remote and in-person consultations.
|
|
|
4. Discussion
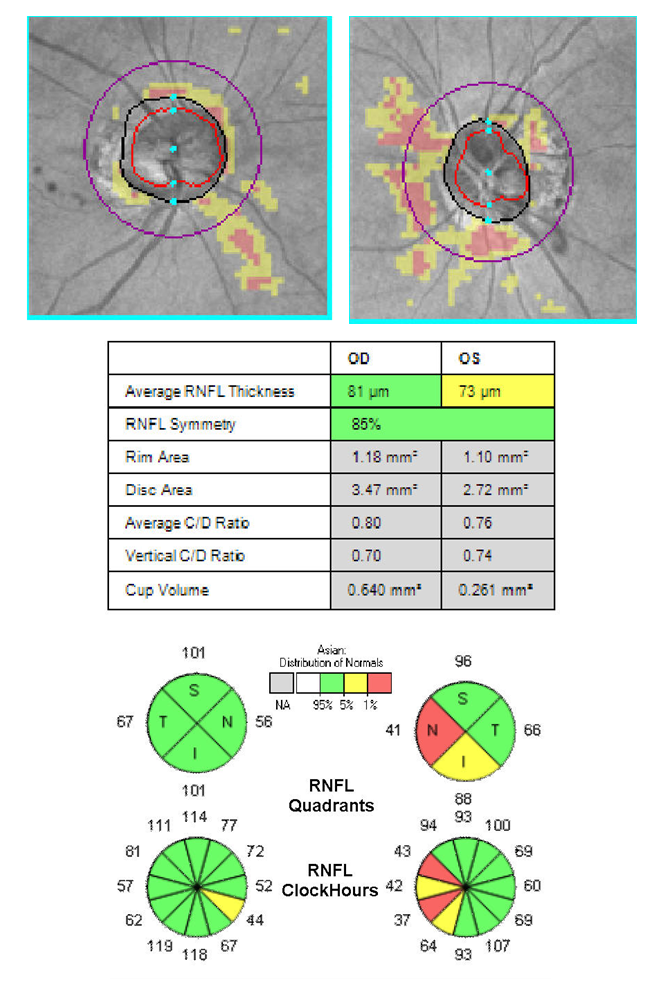
- Digitization of Diagnosis Allows for Rapid Transmission of Completed Examination Results to Specialists at the Central Branch of the Center. Moreover, Thanks to the Capability of Receiving High-Quality Fundus Images, There are No Difficulties Associated with Evaluating the State of the Optic Disc. Furthermore, the Analysis of Color Fundus Photographs in Assessing Glaucoma Patients Abroad is Currently Considered More Effective Than Ophthalmoscopy, as the Monitor Screen Enables Simultaneous Visualization of Fundus Photos and Corresponding OCT Images, Which is Extremely Important in Suspected Glaucoma Cases. Observations Have Shown That Difficulties Were Only Noted in Evaluating the Anterior Segment, as Despite the Presence of Sufficiently High-Quality Equipment for Online Slit Lamp Transmission, Some Aspects Were Still Difficult to Assess Remotely. Specifically, the Resolution and Image Quality Did Not Always Allow for Accurate Determination of Anterior Chamber Depth, Leading to Incorrect Conclusions About Its Depth Reduction and the Need for Gonioscopy, UBM, or Anterior OCT. There Were Also Cases of False Positive Diagnoses of Pseudoexfoliation Syndrome in Patients, Which the In-Person Consultation Excluded. Finally, it was Found That Image Transmission Was Currently Unable to Provide the Capability to Assess the Angle of the Anterior Chamber When Using a Gonioscopy Lens Due to Low Image Detail. Otherwise, the Technical Capabilities of Teleconsultation Did Not Inferior to Those of In-Person Examination. Below is a Clinical Example of Examination Using Teleconsultation in the Form of Fundus Images, OCT Results, and Computer Perimetry of a Patient Suspected of Glaucoma. The Patient, 62 Years Old, IOP OD/OS=23/21 mmHg (Fig. 1-3).
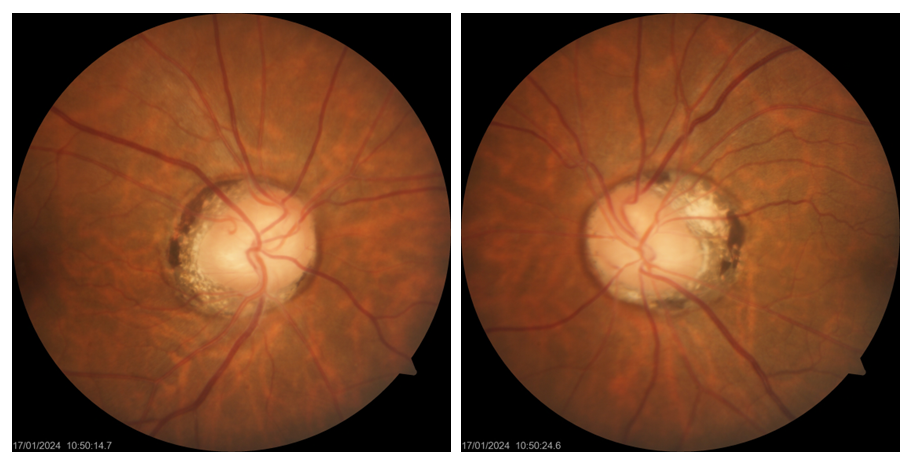 | Figure 1. Fundus images of patient. OU: Optic disc: CDR=0.4-0.5; presence of b-zone parapapillary atrophy; no pronounced defects in RNFL are noted |
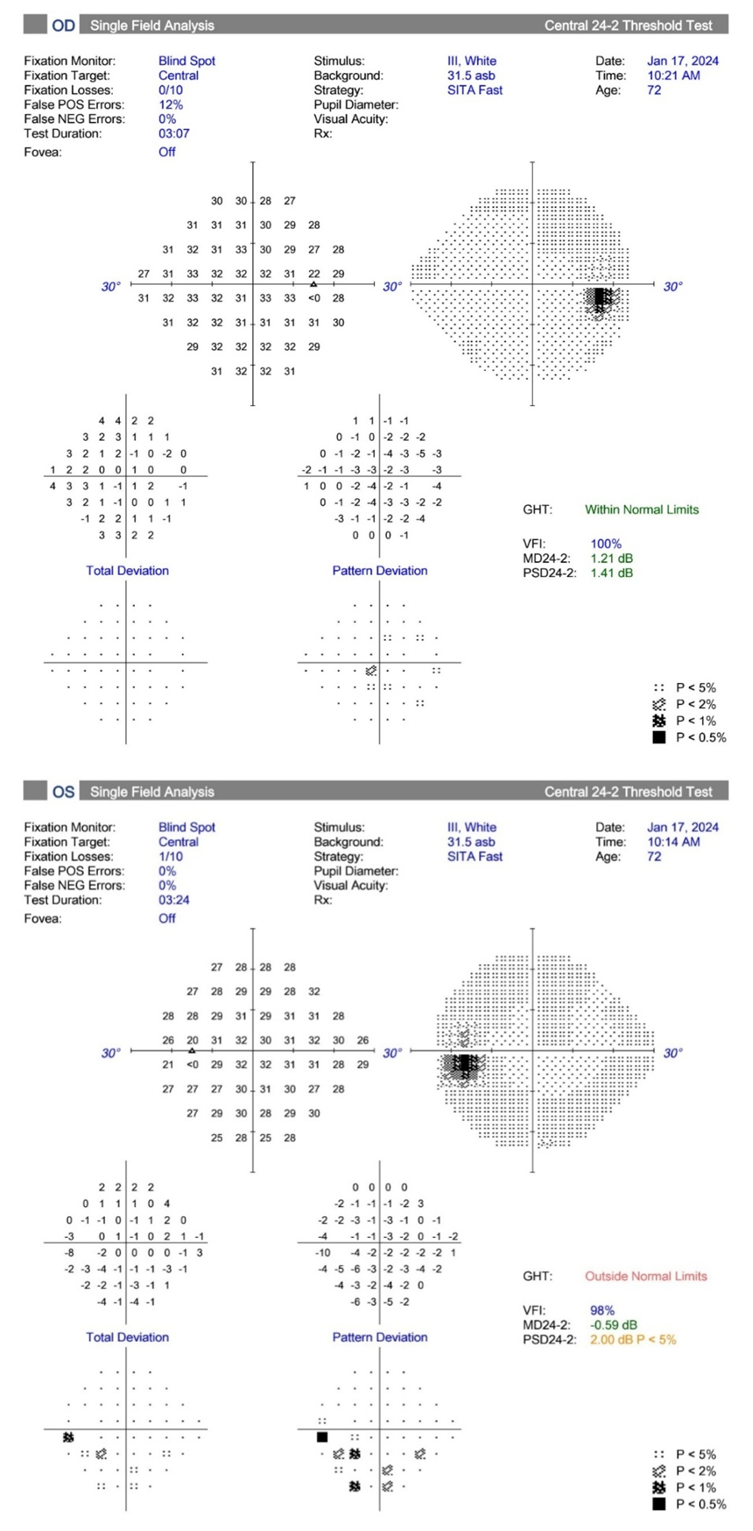 | Figure 3. Results of Humphrey visual field test. OD: Within normal limits. OS: Field defects in the lower nasal and lower temporal quadrants with decreased VFI. PSD at the lower limit of normal |
5. Conclusions
- These results indicate the high diagnostic efficiency of remote telemedicine consultations in detecting ocular hypertension, suspected primary open-angle glaucoma (POAG), and confirmed POAG. The sensitivity and specificity of the remote consultation tests are high, enabling effective identification of patients with these conditions and appropriate measures for further treatment and monitoring.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML