-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1848-1851
doi:10.5923/j.ajmms.20241407.26
Received: Jun. 16, 2024; Accepted: Jul. 12, 2024; Published: Jul. 20, 2024

Cognitive Disorders Degree in Children with Post-COVID Syndrome
Rakhimbaeva G. S., Ishankhodzhaeva G. T., Asomova N. I.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article describes a research study on neuropsychological cognitive functioning in children after COVID-19. A clinical observation was made of 50 children aged 3 to 12 years who applied with catarrhal manifestations, accompanied by signs of damage to both the upper respiratory tract and lower respiratory tract, as well as children with neurological manifestations, from families where adults diagnosed with COVID-19 received outpatient or inpatient treatment.
Keywords: COVID-19, Children, Cognitive function, Neurological disorder, Reflex
Cite this paper: Rakhimbaeva G. S., Ishankhodzhaeva G. T., Asomova N. I., Cognitive Disorders Degree in Children with Post-COVID Syndrome, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1848-1851. doi: 10.5923/j.ajmms.20241407.26.
1. Introduction
- As knowledge about coronavirus disease (COVID-19) has grown, it has become clear that COVID-19 presents with various extrapulmonary manifestations involving multiple organs. Although lung involvement is typical, non-pulmonary multi-organ signs or atypical manifestations are not uncommon [8]. During the COVID-19 pandemic, children and adolescents were at risk of infection in families by being in contact with infected adults. In most cases, children tolerate COVID-19 more easily than adults. However, they were diagnosed with varying severity neurological syndromes - from cranial mononeuropathies to acute Guillain-Barré inflammatory polyneuropathy, and severe brain and spinal cord lesions in the brain and spinal cord, the form of acute hemorrhagic necrotizing encephalopathy and myelopathy [5,6]. Various studies demonstrate encephalopathy as one of the frequent neurological complications of COVID-19. Encephalopathy is a diffuse dysfunction of the brain, manifested by headaches, cognitive impairment, distraction, confusion or oppression of consciousness, sleep disturbances, and convulsive syndrome [2]. According to various studies, the incidence of encephalopathy in adult patients with severe COVID-19 ranges from 9 to 32%, and in extremely severe cases of the disease, it can reach 69% [4,7,10]. It is explained by the high neurotropism and neuroinvasiveness of various representatives of the coronavirus family, which are not so rare and have been proven by many researchers [3]. According to some authors, COVID-19-associated encephalopathy develops due to brain hypoxia and its toxic damage against the background of metabolic changes caused by respiratory failure and systemic inflammatory response, i.e., it has the character of toxic-metabolic encephalopathy [2,4,7]. Involvement of the central nervous system (CNS) occurs by transsynaptic spread or transmission across the blood-brain barrier [8,9,11]. Pathogenetically neurological disorders in COVID-19 may be due to the “cytokine storm”, hypoxemia, homeostasis disorders, neurotropism and neurovirulence of SARS-CoV-2, as well as the combined effect of these factors [5]. Hypoxia, immune-mediated injury, and vascular injury are potential mechanisms for CNS manifestations. Several mechanisms may underlie CNS damage in SARS-CoV-2 infection, such as synaptic transport from infected neurons, penetration through the olfactory nerve, transport through the vascular endothelium, or penetration of leukocytes across the blood-brain barrier. Multiple mechanisms of neurological injury have been postulated, predominantly including hypoxic brain injury, immune-mediated injury, and cerebrovascular injury [2,8]. It should be noted that coronaviruses can activate processes leading to the demyelination of various structures in the peripheral and central nervous systems [3]. Involvement of the central and peripheral nervous system is very common with COVID-19, and in children, the disease may present with only neurological symptoms. Neurological manifestations in children may precede, coincide with, or after respiratory lesions in COVID-19, manifesting with varying degrees of damage to the central and peripheral nervous system. Therefore, further research should focus on short-term and long-term CNS complications and their consequences in patients with COVID-19 [8].It should be noted that in addition to the fact that the condition of a child with signs of post-COVID encephalopathy requires special care. The quarantine regime with restriction of free movement also affects the child's psyche, aggravating the clinic of post-COVID encephalopathy. The primary psychological disorders are not associated with the impact of the infection itself on the central nervous system but with the child's reaction to the situation with the quarantine regime. According to the research results, frequent manifestations of psychological disorders were: behavioural and emotional disorders in the form of increased excitability, frequent disobedience and conflict behaviour with parents and peers, enclosure or isolation, frequent causeless crying, depressed mood, and anxiety, phobias, sleep disturbances. Psychosomatic disorders were also often (respiratory neurosis, increased urge to urinate, enuresis, changes in stool frequency, panic attacks, etc.) [1].Available publications and systematized information have shown that lesions of the peripheral and central nervous systems in children with COVID-19 manifest in various clinical forms. Frequent manifestations are post-COVID encephalopathy, with signs of cognitive dysfunction, which require timely diagnosis and drug adjustment to improve the social adaptation of children in everyday life and educational institutions.Purpose of the study. Neuropsychological study of cognitive activity in children after COVID-19.
2. Methods of Research
- A clinical observation was made of 50 children aged 3 to 12 years who applied with catarrhal manifestations, accompanied by signs of damage to both the upper respiratory tract and lower respiratory tract, as well as children with neurological manifestations, from families where adults diagnosed with COVID-19 received outpatient or inpatient treatment. The control group consisted of 20 neurologically healthy children of the same age. The study included children of the appropriate age category with an established etiological diagnosis and the presence of clinical signs of CNS dysfunction. Children whose neurological disorders could be associated with other causes (inflammatory diseases of the brain, cerebrovascular accidents, traumatic brain injury) or preceded the disease with COVID-19 were not included or withdrawn from the study. Children were diagnosed with COVID-19 based on clinical signs characteristic of ARVI, examination, and data from specific laboratory tests. When examining swab samples from the upper respiratory tract by PCR, 30 (60%) children identified the Covid-19 virus (SARS-CoV-2). At a later blood examination by ELISA, SARS-CoV-2IgG antibodies were detected in 16 (32%) children and SARS-CoV-2-IgM antibodies in only 4 (8%) children. In addition to routine tests, determination of oxygen saturation in the blood, children with neurological manifestations underwent a blood test for CRP, X-ray examination of the lungs, and, EEG and MRI of the brain. A neuropsychological study was performed using the Wechsler test for children. The quality of life of the examined children was assessed by the Russian version of the PedsQL 4.0 Generic Core Scales questionnaire to assess the quality of life of children aged 8–12 years. Statistical processing of the obtained data was performed using the statistical data analysis package "Statistica", 6.0.
3. Results
- 14 (28%) children of preschool age (3-7 years) and 36 (72%) children of primary school age (7-13 years) children with COVID-19 having neurological manifestations were observed. In examined children neurological signs were noted in the form of headaches in 40 (80%), dizziness - 10 (20%), emotional lability - 30 (60%), absent-mindedness - 31 (62%), sleep disturbances - 34 (68%) and memory disorders - 41 (82%). Clinical signs of neurological disorders were manifested mainly in the form of revival of tendon reflexes in 21 (42%) children, increased muscle tone in 11 (22%) children, a slight decrease in muscle tone in 18 (36%) children, and signs of intracranial hypertension in 11 (22%) children.The Wechsler test was considered, as a psychological load on the brain, to determine the degree of disorders in the intellectual-mnestic sphere of children. A comparative analysis of the data showed significant differences between the indicators of the examined groups. Significant differences (Р<0.001) in the intellectual level of patients compared with healthy children were revealed in both groups for all subtests of Wechsler.Clinically, this was expressed in the poverty of the vocabulary, an inadequate behavioural response, and low orientation of children in the environment, reflecting the degree of impairment of verbal and non-verbal thinking due to the coronavirus infection. During the clinical and psychological examination of children with post-COVID encephalopathy, several emotional and behavioural disorders, such as rapid mental fatigue, nervousness, aggressiveness, refusal to contact a doctor, decreased concentration of attention and poverty of other psychomotor reactions were also revealed. In a fragmentary analysis of the subtests of the Wechsler test, significant differences were determined in verbal and non-verbal subtests, which indicates a predominant violation in children of the ability to establish logical connections, a decrease in active attention and working memory. Thus, the verbal subtests "Intelligence", "Similarity", "Arithmetic", and "Repetition of numbers" demonstrated significant differences between the indicators of the examined groups of children. Low scores in the "Arithmetic" and "Similarity" subtests indicate a decrease in the rate of verbal-logical thinking, which is an indicator of memory and attention. Low scores in the "Arithmetic" and "Repetition of Numbers" subtests indicate a low concentration of voluntary attention and operative memory in children with post-COVID encephalopathy.
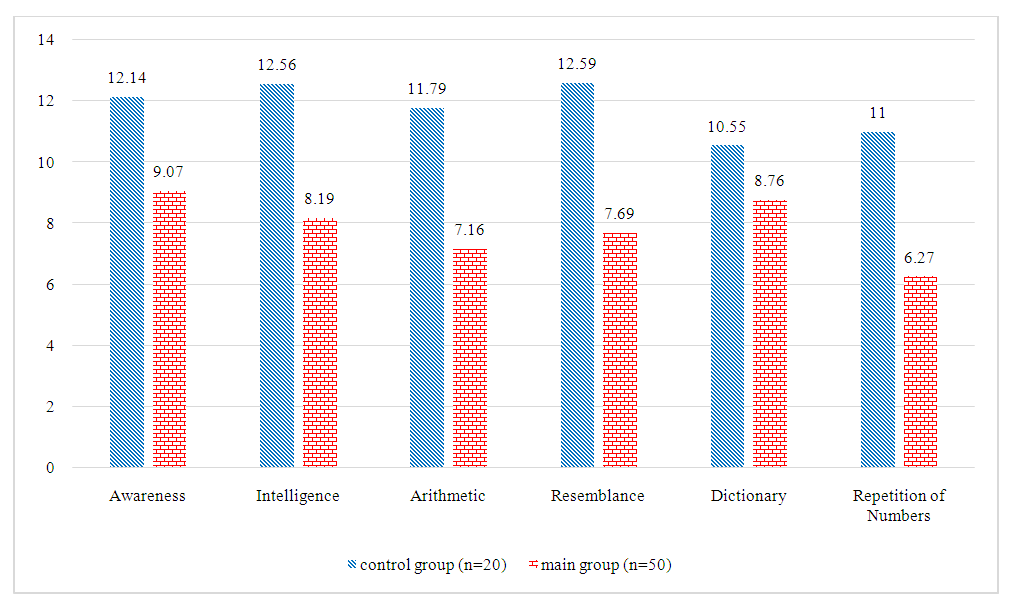 | Figure 1. Comparative analysis of indicators of verbal subtests in the surveyed groups |
 | Figure 2. Comparative analysis of indicators of non-verbal subtests in the surveyed groups |
4. Conclusions
- Thus, studying the cognitive activity of children with the consequences of coronavirus infection using the Wechsler methodology revealed an uneven decrease in intellectual level indicators. Mental disorders of varying severity accompanied post-COVID encephalopathy, and the use of the Wechsler technique makes it possible to identify a number of features of intellectual level disorders, making it possible to improve the methods of differentiated psycho correction of identified neuropsychological disorders. The study's results can find their practical application in the development of medical and social programs for the early rehabilitation of children with post-COVID encephalopathy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML