-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1844-1847
doi:10.5923/j.ajmms.20241407.25
Received: May 10, 2024; Accepted: Jun. 6, 2024; Published: Jun. 15, 2024

Depressive Syndrome After Recurrent Ischemic Stroke
Yo‘lchiyev Elmurod O‘ktamovich
Senior Lecturer, Fergana Medical Institute of Public Health, Fergana, Uzbekistan
Correspondence to: Yo‘lchiyev Elmurod O‘ktamovich, Senior Lecturer, Fergana Medical Institute of Public Health, Fergana, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Health is an incomparable wealth for people all over the world. Today, various types of diseases are increasing day by day due to climate changes in different districts, gases and wastes coming out of modern technologies. Finding effective treatment measures for such diseases is one of the urgent problems of today. Ischemic stroke is one of these diseases, and various methods of its treatment have been found to date. Depressive syndrome that occurs after ischemic stroke is one of the serious complications that arise as a result of this disease. In this article, various methods of its treatment, which method is used in which place, and how to achieve positive results faster, are given. Also, the views of different sciences for the treatment of depression are studied, and the application of the Hamilton scale and its results are explained.
Keywords: Stroke, Recurrent stroke, Human health, Medical institutions, Medical services
Cite this paper: Yo‘lchiyev Elmurod O‘ktamovich, Depressive Syndrome After Recurrent Ischemic Stroke, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1844-1847. doi: 10.5923/j.ajmms.20241407.25.
Article Outline
1. Introduction
- Health is a great blessing that cannot be measured or evaluated by anything for every person and our entire population. Because we all understand well that a healthy person and a healthy people are capable of unprecedented things. As our Honorable President Shavkat Mirziyoyev stated: "Creating high-quality and professional medicine for everyone is an important direction of our strategy". Therefore, the head of our country has been paying special attention to this issue and has been consistently developing the sector. In the following years, historical works were carried out in the way of building a new state and society in our country, and the scope of efforts in this regard is expanding more and more. In particular, the healthcare sector has undergone tremendous changes. Attention and attitude to the industry have changed radically. Especially in the last seven years, consistent reforms have been implemented in our country in order to strengthen human health, radically improve the quality of medical services provided to the population, improve the resource capacity of medical institutions, free and prosperous living and happy life of our people.In our country, extensive work is being carried out aimed at the fundamental improvement of the quality of medical services provided to the population and the development of the health care system. In addition to these activities, attention is paid to the study of the causes of the disease, risk factors, pathogenetic mechanisms of the occurrence of the disease against the background of the coronavirus infection, in the development of secondary prevention and treatment of ischemic stroke, including secondary prevention and treatment of ischemic stroke. Important tasks aimed at "... prevention and diagnosis of diseases, wide introduction of modern technologies, provision of high-quality and high-quality medical care" have been defined. In order to implement the stated tasks, to prevent the redevelopment of cerebrovascular diseases among the population, especially among the population belonging to the "risk group", taking into account the impact of the coronavirus infection, to develop optimal treatment and rehabilitation measures aimed at reducing the complications of them, patients reducing mortality rates and increasing the quality of life is one of the current scientific directions.
2. Materials and Methods
- The dominant risk factors of ischemic strokes, the treatment of cerebrovascular diseases and the organization of rehabilitation measures against the background of the coronavirus infection pandemic are being studied by both foreign and domestic scientists. Risk factors for both primary and recurrent ischemic stroke in patients depending on age and gender (Makarov A.O., 2017; Tibekina L.M., 2018; Nikitenkova V.E, 2020; O'Donnell M. J. et al., 2016) was determined. It has been proven that atherothrombotic, cardioembolic and lacunar types predominate among the pathogenetic types of primary and recurrent stroke. (Rakhmanova Sh.P., 2011; Gafurov B.G., 2019; Geraskina L.A, 2020; Salomova N.K., 2021; Stamm, B.; Huang, D., 2022), ischemic stroke and COVID- A convincing pathogenetic relationship between 19 has not been proven (Beirouti R, Adams Me, Benjamin L, et al. 2020). The endothelium of large arteries in the development of ischemic stroke against the background of COVID-19 inflammation and coagulopathy (Shirokov E.A., 2020; Vozniuk I.A., 2020, C. de Roquetaillade, 2021). Clinical course and consequences of ischemic stroke associated with COVID-19 (Perry R.J., Smith C.J., 2020; Zabolotnaya S.V., 2021; Nadezhdina M.V., 2021; Kabaeva E.N., 2023), cognitive and depressive changes (Parfenov V.A., 2019; Rasulova X.A., Rasulova M.A., 2021), risk of ischemic stroke in concomitant diseases (Pilipovich A.A., 2019; Bogolepova A.N., 2021; Ostroumova O.D., 2022) and effective methods for its prevention (Rakhmatullina E.F., 2022; Rakhimbaeva G.S., Gazieva Sh.R., 2023) have been proven. In ischemic stroke, it has been proven that hypercoagulation and tendency to thrombosis are observed in the hemostasis system (Makarov A.O., 2018; Joly B. S., Siguret V., Veyradier A., 2020; Zhang S. et al., 2021; Nekrasova L.A., 2022; Tang X., Zheng F., 2022). At present, more than 300 risk factors of ischemic stroke have been identified, and there is little information on the risk factors that dominate the occurrence of repeated ischemic stroke against the background of coronavirus infection, the clinical course of the disease, while the changes in the pathogenicity and virulence characteristics of the virus over time make their corrections to the obtained data.
3. Results and Discussion
- Stroke is the second leading cause of death in the world after heart disease. The age-standardized rate of death from stroke in Russia for 2001 was 282 men and 205 women per 100,000 population. The death rate in the acute period of stroke reaches 35%, and by the end of the year it increases to 12-15% [1]. Combined with high mortality rates, stroke is the leading cause of disability in the elderly population, causing up to 80% partial and 10% total disability, and one in two patients die annually. 1 million in Russia people who have had a stroke live, one-third of them are working-age population, and only one in five of them return to work [1]. In Uzbekistan, strokes occur in 35 thousand people a year, and more than 7,000 of them die. The death rate from stroke in Uzbekistan reaches 21% and increases to 12-15% at the end of the first year of illness [2,3]. In patients who survive after a stroke, the probability of recurrence of blood circulation in the brain is 30%. After a stroke, the overall risk of revascularization in the brain is 4-14% in the first two years, 2-3% of patients who survive ischemic stroke in the first month, 10-16% during the first year, and 5% every year after that. recurrence is observed in the rest of the patients. A standardized definition of recurrent stroke was developed to compare data from different studies and conduct an appropriate meta-analysis [2]. Recurrent or recurrent stroke is focal neurologic symptoms lasting more than 24 hours that occur after a primary stroke (a specific acute worsening of a nonprogressive deficit) that is not associated with cerebral edema and dislocation, hemorrhagic transformation, intercurrent disease, hypoxia, or drug intoxication. is any new acute neurological event.Arterial hypertension (AG) is the most common risk factor for ischemic stroke, and according to some researchers, it is now not a risk factor, but an etiology of ischemic stroke. Currently, AG is considered the most widespread non-infectious pandemic in human history, affecting half of the world's population. Damage to the central nervous system as a result of AG can be observed in its various stages, especially in its II and III stages. Among patients with AG, the risk of developing ischemic stroke is 40% higher in people with normal blood pressure [9].Recurrence of stroke is also associated with diabetes, with an incidence of 8% in the general population and 15–33% among stroke patients [5]. Ryglewicz D. et al. (1997) denied the correlation between ischemic stroke and diabetes [10], Omori T. et al. (2015) showed a convincing causal relationship between diabetes and recurrent cardioembolic stroke [3]. Cardiovascular diseases are the cause of 20% of ischemic strokes [4]. A convincing relationship between recurrent ischemic stroke and swinging arrhythmia [7], angina pectoris [10], ischemic heart disease, cardiomyopathy [8] has been established. If the patient does not take anticoagulant and antiplatelet drugs in fluttering arrhythmia, the risk of ischemic stroke is 4.5% [6].There are several neuroimaging predictors of acute II that can be used to predict the risk of early recurrence of stroke. These include multiple acute infarcts, acute II occurring simultaneously in both hemispheres or in both anterior and vertebrobasilar basins, II of different periods (acute and subacute), and location of the infarction in a separate cerebral cortex [8]. The fifth predictor of stroke development is leukoaraiosis, because in the FLAIR mode it is a relatively stable and easy-to-determine parameter, while in the DWI mode, the signs of infarction have the characteristic of rapid changes in dynamics.Thus, the risk factors that play an important role in the recurrence of ischemic stroke have been identified. But the SARS-CoV-2 pandemic has made its corrections to the accumulated knowledge. Observational data suggest that neurologic symptoms may also occur in patients with COVID-19, and cerebrovascular disease is considered the most common comorbid condition. Different authors show different numbers about the frequency of primary stroke in COVID-19, for example, the frequency of type II in Wuhan was 2.34% [9], while in New York City it was 0.9%.Studies have shown that acute bacterial and viral infections, especially infections associated with respiratory diseases, are a temporary, i.e. transient, immediate risk factor for stroke development [10]. The association between acute infection and stroke stems from the systemic inflammatory response to infection, which can lead to endothelial dysfunction and induce procoagulant states [10]. It is difficult to differentiate between symptoms of asthenia and apathy in stroke patients as a result of depression or "organic" post-stroke depression. Indifference to depression causes worsening of the patient's condition - decreases the patient's physical activity and quality of life, increases the risk of suicide. Depression reduces patient motivation for treatment, increases disability, increases the risk of re-stroke and ultimately death. Determining depression in a patient has a negative prognostic value.Diagnosing depression in stroke patients is more difficult, in many cases aphasia prevents communication with the patient, changes in facial expressions can be caused by prosoparesis, crying can be caused by pseudobulbar syndrome, apathy can be caused by damage to the right hemisphere. Diagnostic criteria for post-stroke depression include the presence of 3 or more of the following symptoms during the past week and not previously observed:- The patient does not communicate most of the day, every day or most of the week; - Fatigue every day or most of the week;- Depressed mood most of the day, every day or most of the week (often cries, sad);- Insomnia, early awakening or hypersomnia every day or most of the week;- A feeling of helplessness and worthlessness most of the day, every day or most of the week;- Periodic thoughts about death, attempts to commit suicide;- Feeling hopeless most of the day, every day, or most of the week;- Unreasonable nervousness every day or most of the week;
4. Hamilton Depression Rating Scale (HDRS)
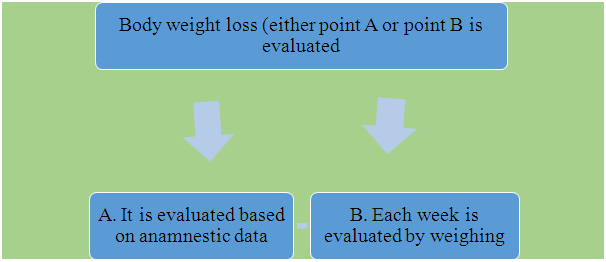
- The Hamilton Depression Rating Scale is one of the most widely used depression scales. This scale consists of 23 items, 2 of which (items 16 and 18) consist of two parts and are filled in alternately. 1. Low mood (sadness, despair, weakness and low value);2. Guilt – feelings and thoughts of guilt or thoughts of past mistakes (sins), thoughts of punishment for them, incriminating verbal or visual hallucinations.3. Suicidal thoughts - feelings of low worth can lead to suicide. 4. Early insomnia (difficulty falling asleep). 5. Moderate insomnia.6. Late insomnia (early awakenings).7. Ability to work and activity.8. Inhibition (slowing down of thinking and speech, loss of concentration, slowing down of motor activity). 9. Agitation (excitement).10. Mental anxiety.11. Somatic anxiety (physiological symptoms of anxiety: gastrointestinal - dry mouth, stomach pain, flatulence, diarrhea, dyspepsia, spasms, belching; cardiovascular - rapid heartbeat, headache pain; breath - hyperventilation, holding breath, panting; frequent urination; profuse sweating).12. Somatic symptoms of gastrointestinal changes.13. General somatic symptoms. 14. Changes in the sexual sphere (genital symptoms) (loss of libido, menstrual changes).15. Hypochondriac changes.16.
 17. Attitude towards one's illness (criticism towards one's illness).18. Daily fluctuations of the patient's condition.A. In what part of the day is the patient's condition worse - morning or evening.B. If diurnal fluctuations are observed, their significance is evaluated.19. Depersonalization and derealization.20. Obsessive changes (paranoid symptoms).21. Obsessive and compulsive changes.Scores 18-21 do not reflect the degree of depressive symptomatology in the outcome assessment. When assessed by the first 17 points, the levels of depression are distributed as follows (G.P. Panteleeva, 1998), and itis adapted to the ICT-10:
17. Attitude towards one's illness (criticism towards one's illness).18. Daily fluctuations of the patient's condition.A. In what part of the day is the patient's condition worse - morning or evening.B. If diurnal fluctuations are observed, their significance is evaluated.19. Depersonalization and derealization.20. Obsessive changes (paranoid symptoms).21. Obsessive and compulsive changes.Scores 18-21 do not reflect the degree of depressive symptomatology in the outcome assessment. When assessed by the first 17 points, the levels of depression are distributed as follows (G.P. Panteleeva, 1998), and itis adapted to the ICT-10: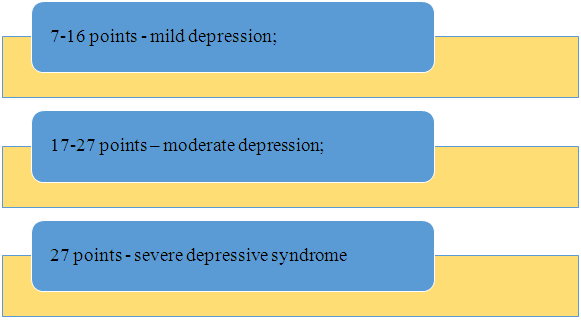 In order to prevent depressive syndrome, it is necessary to regularly engage in the following activities. Regular rest in the sun, creating a positive environment at home and at work, a healthy lifestyle: proper nutrition and regular exercise, giving up bad habits, alternating between work and rest, enough sleep, meditation and practicing yoga.
In order to prevent depressive syndrome, it is necessary to regularly engage in the following activities. Regular rest in the sun, creating a positive environment at home and at work, a healthy lifestyle: proper nutrition and regular exercise, giving up bad habits, alternating between work and rest, enough sleep, meditation and practicing yoga.5. Conclusions
- 1. It is important to identify all the causes and factors that lead to depression in a timely manner. The initial conditions for the development of depression can be different, and doctors can correctly identify it. In order not to get this disease, first of all, every person should avoid severe or light head injuries, chronic inflammatory processes in the body, constant stress, emotional overstrain and overload, constant insomnia, brain strain, avitaminosis, previous diseases. due to general fatigue, poisoning or intoxication, excessive consumption of nicotine, alcohol, drugs should be avoided. 2. Modern lifestyle often leads to depression. The desire to achieve all the benefits of humanity, unreasonable expectations, excessive demands on oneself and others, fear of loss, inability to digest a large flow of information also lead to this disease. For this reason, a person should always know his own standards in these actions. It is very important to recognize the syndrome in time and prevent its progression. The person himself rarely diagnoses this disease and puts it aside until the end. All foods consumed should contain the most antioxidants, which will allow a person to quickly get out of a state of depression.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML