-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1822-1828
doi:10.5923/j.ajmms.20241407.21
Received: Apr. 23, 2024; Accepted: May 16, 2024; Published: Jul. 18, 2024

Prevalence and Prevention of Headaches Caused by Sleep Disorders
Bozorov Shakhobjon Ismatovich1, Tolibov Dilshod Sirojovich2
1Department of Neurology, Bukhara State Medical Institute, Uzbekistan
2Department of Neurology and Medical Psychology, Tashkent Medical Academy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article deals with the prevalence of various types of headaches caused by sleep disorders and measures for their early prevention.
Keywords: Headache, Sleep disturbance, Apnea, External environmental factors, Prevention, Spread
Cite this paper: Bozorov Shakhobjon Ismatovich, Tolibov Dilshod Sirojovich, Prevalence and Prevention of Headaches Caused by Sleep Disorders, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1822-1828. doi: 10.5923/j.ajmms.20241407.21.
1. Relevance
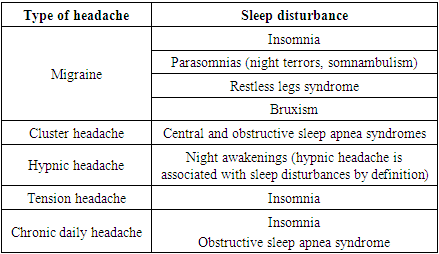
- Sleep is an integral part of life and one of the basic human needs, and sleep disorders are a significant clinical problem. Almost 50% of the population suffers from some kind of disorder sleep. Sleep disorders are closely associated with both diseases of the nervous system and mental disorders, but patients suffering from such diseases prefer to seek help from neurologists. Sleep disorders affect more than 45% of the world's population and have become a global health problem in recent decades. And from this point of view, headaches included in number of the most common complaints: according to the World Health Organization, they affect 50–75% of the adult population. That's why headache, and sleep disorders have become global health problem. In everyday clinical practice, the most common syndrome is characterized by insomnia, various sleep disorders and subsequent daytime awakenings and resulting headaches. Primary headaches include migraines, tension headaches, cluster headaches, and other less common variants. The connection between headaches and sleep disorders is multifaceted. On the one hand, headaches can be a consequence of sleep disturbances; a typical example is hypnotic headache. On the other hand, lack of sleep can lead to headaches. The first large-scale epidemiological study was conducted in Denmark to assess the incidence of comorbidity between headache and sleep disorders. 68,518 people took part in the survey, most of them under the age of 55 (80% responded offline, 20% online). 18.1% of people had headache and insomnia at the same time (the high frequency of comorbidity of these diseases is associated with common pathophysiological mechanisms). Another 16.3% suffered only from headaches, and 21.1% only had trouble sleeping. Comorbid pathology was more often observed in women and middle-aged people. Other risk factors include low socioeconomic status, unhealthy lifestyle (overweight/obesity), high stress levels, anxiety and depression. Sleep disturbances can be acute (transient), short-term (up to 6 months) and chronic (more than 6 months). Acute sleep disturbances can occur in any person under the influence of stress or overexcitation due to time zone change. Chronic insomnia develops in people prone to it. Typically, this condition affects elderly patients, women, people who, for one reason or another, sleep no more than 5 hours a day, as well as people who have not worked for a long time, divorcees, those with psychological and mental trauma, and patients. chronic diseases. The most common complaint of patients is difficulty falling asleep. A person experiences the desire to sleep before going to bed, but disappears when a person goes to bed under the influence of various factors. These may be unpleasant thoughts and memories, discomfort in the legs, pain or itching, or the inability to find a comfortable position due to extraneous sounds. Light drowsiness is disturbed by even the slightest noise, and sometimes a falling asleep person feels as if he “didn’t sleep for a minute.”There can be many reasons for difficulty falling asleep, including lack of fatigue, staying in bed for long periods of time during the day, irregular bedtimes, and medical conditions that cause swelling, itching, or pain. The researchers concluded that patients with headaches and sleep disorders should be actively identify in clinical practice. Lifestyle changes, stress reduction, and screening for depression and anxiety can go a long way in treating and preventing the combination of headaches and sleep disorders.
 | Figure 1 |
|
2. Materials and Research Methods
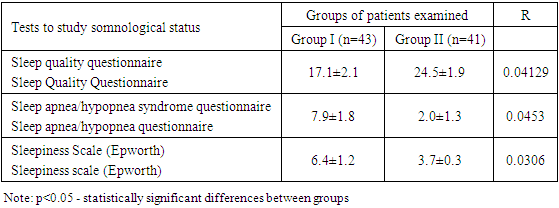
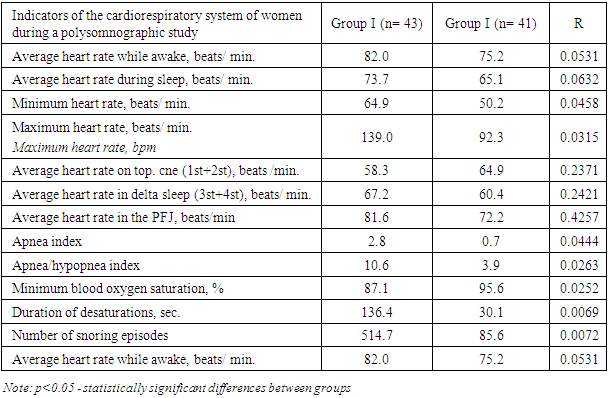
- Using modern examinations and neuropsychological tests that identify sleep disorders, diagnostic examinations and neuropsychological tests were carried out to determine sleep disorders in 133 groups of patients of both sexes aged 18-59 years with a diagnosis of “Primary headaches” and “Vegetative-vascular dystonia”., asthenia, based on examinations, Primary headaches. To determine the comparative level of sleep disturbances in patients suffering from pain and vegetative-vascular dystonia, asthenic diagnostics and EEG studies of higher nervous activity are used. At the stage of studying the characteristics of the somnological status, patients with excess body weight (BMI 25–29) and a diagnosis of “metabolic syndrome” were selected based on one main and two additional criteria (HOMA-IR resistance index ≥2.77, glucose level in fasting blood plasma ≥5.1 mmol/l). Additional criteria were high-density lipoprotein level <1.2 mmol/l, low-density lipoprotein level >3.0 mmol/l, triglycerides ≥1.7 mmol/l, urinary albumin excretion level >20 mcg/min., blood pressure 140 /90 mmHg Art., ratio of waist circumference to hip circumference >0.85. Two clinical groups were formed: I - main (77 patients with excess body weight, BMI 25-29, ambi-LPPA) and II - control (71 patients with normal weight, BMI 18-24, ambi-LPPA-A). To study the somnological status, the “Questionnaire for scoring subjective characteristics of sleep” (modification of the Spiegel questionnaire) was used (with a score of <19 points, sleep disorders were diagnosed). Sleep-disordered breathing was identified using the Sleep Apnea Screening Questionnaire (a score of 4 points indicated breathing disturbances). The level of daytime sleepiness was determined using the Epworth Sleepiness Scale (1990) (5–9 points indicated severe daytime sleepiness). Somnographic examination of patients was carried out using the software and hardware complex “Encephalan-EEGR-19/26” at night. An electroencephalogram (EEG), electrocardiogram (ECG), electrooculogram (EOG), electromyogram (EMG) of the hypoglossal muscle, respiratory rate (RR), pulse oximetry, and actigraphy were recorded. The EEG was recorded monopolarly using the 10/20 system in symmetrical frontal, temporal, central, parietal and occipital leads with a time constant of 0.3 sec. EEG analysis was carried out on epochs lasting 20 s while determining frequency-amplitude and spectral characteristics using the fast Fourier transform method and determining sleep events using the cluster method. The index of severity of EEG frequency ranges was calculated: delta activity (0.5–2 Hz), delta 2 activity (2–4 Hz), theta activity (4–8 Hz), alpha activity (8–12 Hz), sigma activity (12–18 Hz), beta activity (18–36 Hz), as well as localization of the maximum amplitude of EEG rhythms for each stage of sleep. EEG characteristics were studied while awake with eyes closed before sleep, in all phases of sleep and after awakening. The structure of sleep (phases, cycles, stages, hypnograms) was assessed using EEG, EMG, ECG and RR indicators. Sleep efficiency (SE) was determined in minutes using the formula: ES = (DS+DD)/(LS+SB), where: DS - total sleep duration, DD - delta sleep duration, LPS - latent value of sleep onset, SV - time wakefulness inside the night. The lower the ES value, the more productive the sleep was considered. At the same time, segmental sleep indicators were assessed by calculating the number of segments (areas of homogeneous sleep depth) in sleep stages. The proportion of segments in each stage was determined with a total stage duration of 100%. In addition, the number and duration of different types of intersegmental episodes in sleep stages were determined.SPIEGEL SLEEP subjective scale questionnaire:SPIEGEL SLEEP SUBJECTIVE RATING SCALE
|
|
3. Results of the Study
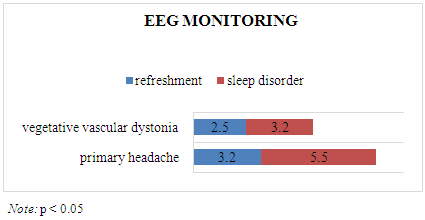
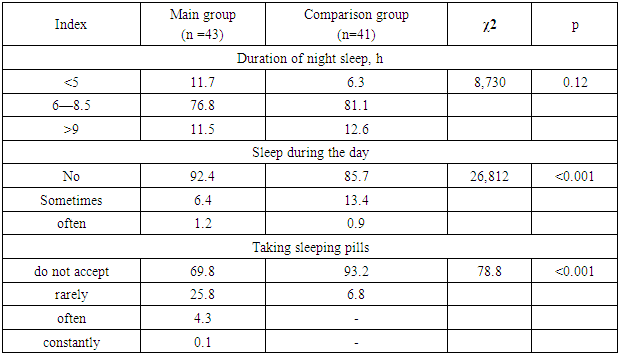
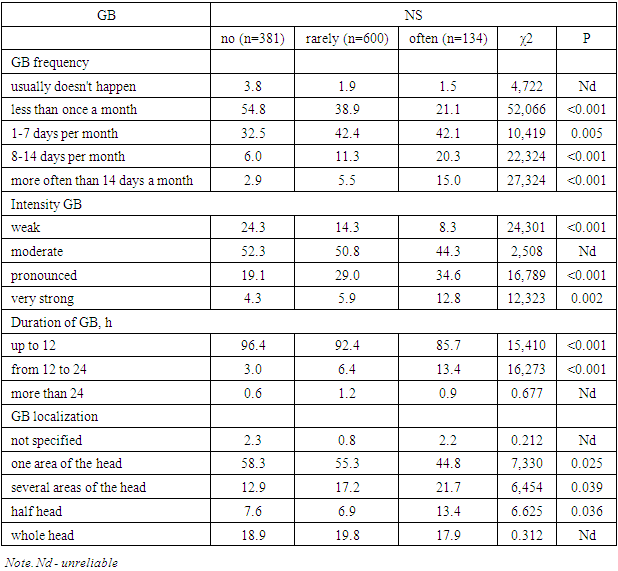
- So, it can be seen that when conducting the Spiegel Sleep Disorders Scale, a total of 15 sleep disturbance points were obtained in groups of 43 patients with primary headache. In a group of 3–9 patients with an asthenic diagnosis of VSD, this indicator was 22 points. In our following table, the high rates of headaches caused by sleep disorders were 5.5 points for primary headaches and 3.2 points for patients with an asthenic diagnosis of VSD.
|
|
|
4. Conclusions
- In conclusion, it should be said that primary headaches due to sleep disorders, vegetative-vascular dystonia, compared with sleep disorders of the asthenic type, formed a high rate.Thus, early diagnosis of sleep disorders in patients with primary headaches and vegetative-vascular dystonia is important for improving the quality of life and maintaining labor productivity, and early treatment and preventive measures are important for various types of headaches that occur in patients. pain is prevented.The data obtained indicate the possibility of identifying the category of patients with excess body weight using lateral typing. The results obtained on sleep disturbances in overweight patients with ambi-LPPA at the pregravid stage, which, on the one hand, are the result of hormonal changes against the background of existing metabolic and autonomic abnormalities in patients.Preventive measures in patients should be avoided primarily from stress, psycho-emotional stress, various weather conditions, people working in various professions, especially those working at night, should develop a daily routine, diet, diet and food should contain sufficient amounts of minerals and vitamins.Various painkillers and sleeping pills give us temporary relief, but cannot eliminate the root cause.Therefore, patients with various sleep disorders need to consult a specialist (neurologist, psychoneurologist, somnologist, psychiatrist) and receive the necessary recommendations.
References
| [1] | Bozorov Shakhobjon Ismatovich “MODERN DIAGNOSTIC METHODS OF SLEEP DISORDERS IN PRIMARY HEADACHES” IBAST/Volume 3, Issue 6, June. /2023. // INTERNATIONAL BULLETIN OF APPLIED SCIENCE AND TECHNOLOGY //. C 926-929. |
| [2] | A. Ismatov, D. Tolibov, G. Rakhimbaeva. Features of mri signs in patients with Parkinson's disease Parkinsonism and Related Disorders 113 (2023) 105512, P020. |
| [3] | Bozorov Shahobjon Ismatovich CLINICAL SIGNIFICANCE AND PREVALENCE OF SLEEP DISTURBANCE IN PRIMARY HEADACHES No. 3 2023 // JOURNAL OF NEUROLOGY AND NEUROSURGICAL RESEARCH //. C 86-88. 83 Bozorov Shaxobjon Ismat o'gli, Tolibov Dilshod Sirojovich. // REDUCED CONCENTRATION OF ATTENTION IN PRIMARY HEADACHES //. Journal NEW DAY IN MEDICINE. Entered 07/20/2023. 8 (58) 2023. pp. 192-195. |
| [4] | Talibov DS, Karshiboyeva NI. Ischemic stroke caused by lack of blood coagulation system inhibitors in young people. "Neurology" — 3(95), 2023, str. 44-467. |
| [5] | Tolibov Dilshod, Ismatov Alimardon Qon tomir demensiyasi rivojlanishining xavf omillari “Journal of neurology and neurosurgical research”, 2/2021, 22-25b. |
| [6] | Dilshod Sirojovich Tolibov, Rushana Abubakirovna Salimova, Jamoliddin Muxiddin-O'g'li Sharafiddinov. Optimization of approaches to early diagnosis of Alzheimer's type dementia at the outpatient level The American Journal of Medical Sciences and Pharmaceutical Research (ISSN – 2689-1026) VOLUME 04 ISSUE 04 2022y. Pages: 28-31. |
| [7] | G.S. Rakhimbaeva, Sh.R. Gazieva, M.K. Ataniyazov, F.Ch. Muratov, D.S. Tolibov, U.D. Shodiev. Features of treatment and rehabilitation of patients who have suffered COVID-19 with ischemic stroke. Journal of Neurology and Psychiatry. S.S. Korsakova 2023, vol. 23, no. 3, issue. 2, p. 76–84. |
| [8] | Tolibov Dilshod Sirojovich., Bozorov Shaxobjon Ismat o'gli. Sleep Disturbances in Primary Headaches Vol. 1 No. 4 (2022): // INTERNATIONAL JOURNAL OF HEALTH SYSTEMS AND MEDICAL SCIENCES// C 93-96. |
| [9] | Bozorov Shaxobjon Ismat o'gli, Tolibov Dilshod Sirojovich. // Effect of stressors on primary headache. IBAST Volume 3, Issue 10, October. // International Bulletin of Applied Science And Technology // C 481-485. |
| [10] | G. Goyibova, A. Umarov, A. Ismatov, D. Tolibov. Clinical tremor-study with gender features in patients with essential tremor in Uzbekistan Parkinsonism and Related Disorders 113 (2023) 105512, P2. |
| [11] | A. Ismatov, D. Tolibov, A. Umarov. Study of the difficulties of late diagnostics in patients with Huntington's disease in Uzbekistan Parkinsonism and Related Disorders 113 (2023) 105512, P200. |
| [12] | Azamatjon Umarov, Dilshod Tolibov Specifications of epilepsy and cerebral palsy in children Journal of the Neurological sciences, 2021y, EP0399/#2985, ISSN 0022-510X. |
| [13] | Tolibov DS, Maxmudov E. Covid- Assotsirlangan kavernoz sinus trombozini erta tashxislash. International scientific and educational electronic journal, Education and science in the 21st century, No. 23 (volume 6) (February, 2022). |
| [14] | Tolibov Dilshod Sirojovich, Ismatov Alimardon Nabijon o'g'li. Cognitive functions in the early diagnosis of vascular dementia of stenosis of the main arteries of the head. British Medical Journal Volume 3, No.1, January 2023, pages 17-22. |
| [15] | Tolibov DS, Qarshiboyeva NI Yoshlarda qon ivish tizimi ingibitorlarining etishmasligi tufayli yuzaga kelgan ishemik insult. "Nevrologiya"—3(95), 2023, str. 44-46. |
| [16] | GS Rakhimbaeva, DS Tolibov. Principles of early diagnosis and modern treatment of Alzheimer's disease Monograph 2023y. |
| [17] | Gaffarova VF Clinic -eeg correlation somatogenous of conditioned febrile seizures in children. // International Journal of Human Computing Studies. 2021. – R. 114-116. |
| [18] | Davronova X. Z. Decline coefficient factional anisotropy How factor development cognitive violations at post-stroke sick // Actual Issues and Solution of Development of Economic Sectors of the Republic of Uzbekistan in Modern Conditions Proceedings of the international conference. – Jizzakh, 2022. - No. 1. – pp. 764-770. |
| [19] | Davronova Hilola Zavkiddinovna. Reduced concentration of attention in type II diabetes. // INNOVATIONS IN TECHNOLOGY AND SCIENCE ED UCATION. ISSN 2181-371X, SJIS 2023: 5.305 VOLUME 2, ISSUE 8 P. 1250 to 1254. |
| [20] | Salomova, N. K. (2022). Risk factors for recurrent stroke. // Polish journal of science N, 52, 33-35. |
| [21] | Salomova, N. K. (2021). Features of the course and clinical and pathogenetic characteristics of primary and recurrent strokes. // Central Asian Journal of Medical and Natural Science, 249-253. |
| [22] | Rakhmatova DI Forecasting of complications of facial nerve neuropathy according to the results of electroneuromyography // World journal of pharmaceutical research. – India, 2020. –Vol. 9, Issue 5. - P. 1547-1555. ISSN 2277 – 7105. SJIF Impact Factor 8.084. |
| [23] | Rakhmatova DI Opportunities Of Acupuncture In Treatment Of Facial Nerve Neuropathy // European Journal of Molecular & Clinical Medicine. ISSN 2515-8260 Volume 07, Issue 07, 2020. – R. 567-572. |
| [24] | Tabeeva GR, Evdokimova EM, Shagbazyan AE Kognitiv buzilishlari bo'lgan bemorlarda uyqu buzilishi: clinic phenomenology va therapy strategiyalar. Asab kasalliklari, 2017, 2: S. 21-28. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML