-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1781-1783
doi:10.5923/j.ajmms.20241407.11
Received: Jun. 10, 2024; Accepted: Jul. 6, 2024; Published: Jul. 10, 2024

Analysis of the Etiological Structure of Respiratory Diseases in Children
Turaev Telman Temirovich
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Turaev Telman Temirovich, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Reducing the incidence of acute infectious respiratory diseases in children and mortality is currently considered as a strategic direction for the development of pediatric care in modern healthcare. According to modern concepts, innate immunity plays an important role in the implementation of the body's immune response in the early stages of infectious diseases. The authors conducted a study of indicators of humoral and cellular immunity in children to predict the development of emergency conditions in respiratory diseases in children. IgG control in dynamics determines the prognosis of the development of critical conditions in respiratory diseases in children. As an indicator of humoral immunity, IgG plays a complex role in the process of protecting against the re-entry of foreign antigen into the body, which prevents reinfection.
Keywords: Cellular immunity, Cytokines, Children, Respiratory diseases, Immune response, Urgent conditions
Cite this paper: Turaev Telman Temirovich, Analysis of the Etiological Structure of Respiratory Diseases in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1781-1783. doi: 10.5923/j.ajmms.20241407.11.
Article Outline
1. Introduction
- Currently, a steady increase in the frequency of respiratory allergic diseases is relevant. Allergies are very often associated with the recurrent nature of the course of respiratory diseases. The symptoms of respiratory atopy can both mimic the symptoms of a respiratory infection, and be the cause of chronic inflammation of the respiratory tract and immunodeficiency, against which the child has frequent infections [4,6]. In recent years, persistent infections caused by representatives of the Herpesviridae family, the primary infection of which in the population of our country occurs more often at preschool age, have become particularly relevant. The immediate and long-term prognosis for a person infected with herpesviruses depends on the presence and severity of immune dysfunction. At the same time, representatives of the Herpesviridae family themselves are capable of causing significant disturbances in the immune status of the macroorganism, causing lymphoproliferation and chronic inflammation [2,5,8].According to the World Health Organization (WHO), in the global structure of pathologies of children, the incidence of infectious diseases is more than 90%. Infectious agents are the cause of 35% of deaths among children [3].Over the past 4 years, there has been an increase in the number of children's intensive care units (ICU) by 17.8%, while deaths have decreased by 38% of the total number of cases. Infants, toddlers, and high school age children predominate among all pediatric ICU patients. More than 60% of the total mortality of patients in children's intensive care units is due to unfavorable outcomes of critical conditions in children of the first three years of life [7].In Switzerland and Italy, almost 50% of the total number of pediatrician consultations are conducted for acute respiratory diseases (ARI), in the USA acute respiratory infections are one of the main causes of hospitalizations, in the Russian Federation – 90% of outpatient visits and home visits are for respiratory diseases [1,9].The purpose of the research: study of the etiological structure of respiratory diseases in children.
2. Materials and Methods of Research
- 280 patients who applied for respiratory symptoms similar to allergies in the periods from 2020-2022 to the advisory polyclinic of the BODMPMC in Bukhara were under observation. The Chi of the square, the two-sided Fisher criterion, the normalized value of the Pearson coefficient and the bond strength for the two-by-two matrix were calculated simultaneously in an online calculator.
3. Results and Discussion
- Of all those who applied to the polyclinic for outpatient consultation, boys were 1.35 times more -161 (57.5%) than girls -119 (42.5%). The age distribution of patients showed a predominance of preschool children -185 (66.0%). At the same time, there were 59 (21.0%) young children, 185 (66.0%) preschool children, 25 (9.0%) 8-11 years old and 11 (4.0%) 12-18 years old, Fig. 1.
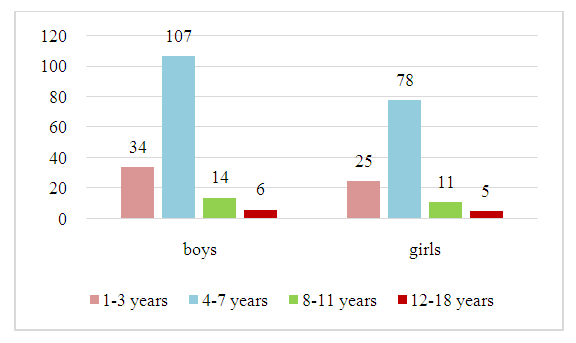 | Figure 1. Distribution of sick children by gender and age |
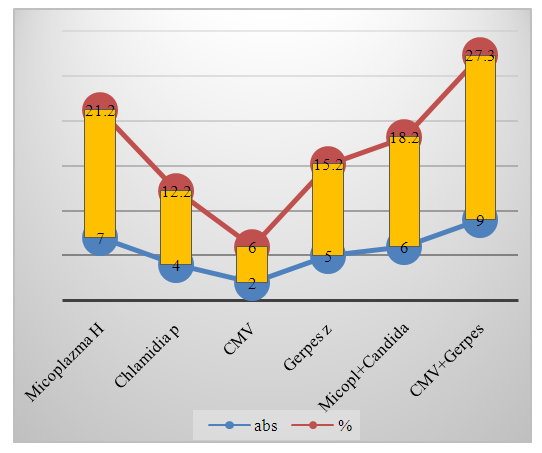 | Figure 2. Pathogens of respiratory diseases in young children |
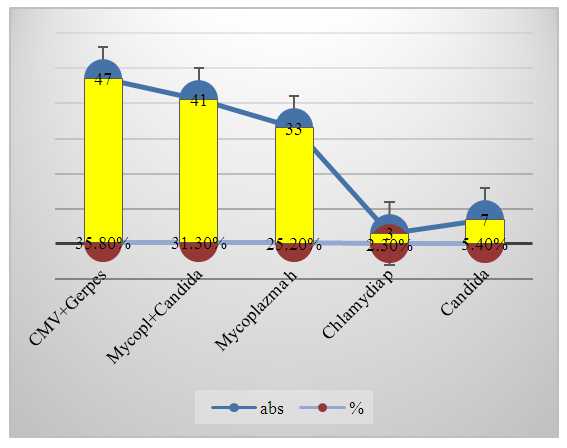 | Figure 3. Pathogens of respiratory diseases in preschool children |
4. Conclusions
- Thus, the study of the etiology of respiratory diseases in children made it possible to establish cases of coinfection in children with RRI. Respiratory diseases with persistent infections in our studies account for 62.2%, which is 1.64 times more than the combination with atopy in children.At the same time, the association of viruses with each other, bacteria with each other, the virus is fungal, the virus is mycoplasmic and parasitic. Age-related features of the association of respiratory pathogens have been established.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML