-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(7): 1763-1769
doi:10.5923/j.ajmms.20241407.08
Received: Jun. 5, 2024; Accepted: Jun. 25, 2024; Published: Jul. 5, 2024

Combined Pelvic Floor Muscle Training and Electrical Stimulation in Managing Sexual Dysfunction
Nargiza Mirkhamidova1, Adibakhon Usmankhodjaeva2
1Department of Rehabilitology, Traditional Folk Medicine and Physical Education, Tashkent Medical Academy, Tashkent, Uzbekistan
2Head of the Department of Rehabilitology, Traditional Folk Medicine and Physical Education, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Nargiza Mirkhamidova, Department of Rehabilitology, Traditional Folk Medicine and Physical Education, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

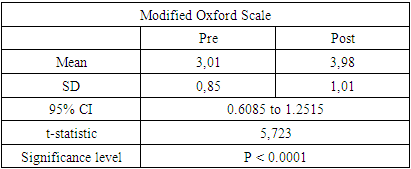
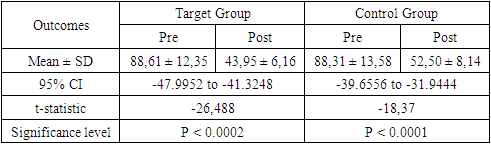
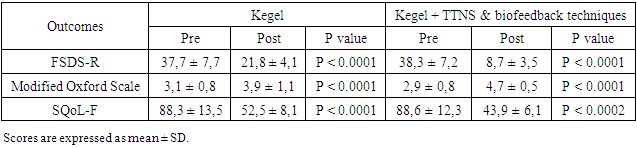
While restoring sexual function is critical for women with neurological disorders, its evaluation is often neglected. Methods: The study assessed 133 women aged 18–74 with neurological disorders, evaluating the effectiveness of biofeedback, transcutaneous tibial nerve stimulation (TTNS), and Kegel device therapy, through a three-step questionnaire process. Results: Target group showed significant reductions in FSDS-R scores, with increases in Modified Oxford Scale and SQoL-F scores indicating improved pelvic floor muscle strength and enhanced sexual quality of life. The control group's improvements were less pronounced. Conclusion: The findings revealed enhancements in sexual function and overall quality of life among the participants following the therapeutic interventions.
Keywords: FSDS-R, SQoL-F, Female sexual dysfunction, Modified oxford scale, Biofeedback, Kegel device, Transcutaneous tibial nerve stimulation
Cite this paper: Nargiza Mirkhamidova, Adibakhon Usmankhodjaeva, Combined Pelvic Floor Muscle Training and Electrical Stimulation in Managing Sexual Dysfunction, American Journal of Medicine and Medical Sciences, Vol. 14 No. 7, 2024, pp. 1763-1769. doi: 10.5923/j.ajmms.20241407.08.
1. Introduction
- Investigations into women with neurological disorders such as stroke, multiple sclerosis (MS), and traumatic brain injury (TBI) have grown, demonstrating sexual challenges are widespread and demand comprehensive appraisal and intervention to elevate the quality of life for these demographics. Despite this progress, current research points to persistent unmet needs related to sexuality among these neurological groups, highlighting the potential for healthcare providers to enhance their evaluation and response to these concerns more proficiently [1]. Urinary incontinence, spasticity and pain can disrupt sexual function and significantly impact the willingness to engage in sexual activities, although desire, arousal, and orgasm are attainable, women have reported experiencing additional complications [2-5]. On the other hand, some studies have observed occurrences of increased sexual desire in women who have suffered from a stroke [6]. The interplay of neurological impairments and the intimate nature of sexual function creates a unique set of challenges for these patients. Traditional treatment modalities often fail to address the multifaceted nature of sexual dysfunction and recent findings in the field of neurorehabilitation and sexual health have emphasized the need to integrate various therapeutic strategies to address these issues effectively [7,8]. The concept of pelvic floor physiotherapy from its historical development to its contemporary applications, empowers healthcare professionals to implement the therapy effectively with their patients. It underscores that various pelvic floor therapy strategies are in use, yet a clear understanding is lacking among professionals, occasionally resulting in more harm than benefits [9].The findings from research indicate that both transcutaneous tibial nerve stimulation (TTNS) and pelvic floor muscle training (PFMT) effectively improved symptoms in female multiple sclerosis patients [10,11].Patients enhance their awareness of positive physiological sensations by using mindfulness strategies while improving voluntary control over pelvic muscles through biofeedback. Moreover, the Sexual Wellness Enhancement and Enrichment Training Model, a group therapy method, is fundamentally structured around the combination of biofeedback and mindfulness [12-13]. Biofeedback therapy is effective in alleviating sexual pain in women, though it has not been shown to be superior to other treatments [14]. The Revised Female Sexual Distress Scale (FSDS-R) for assessing sexual distress in women with hypoactive sexual desire disorder (HSDD). Have been used with findings revealed that the FSDS-R, along with its item 13, demonstrated strong discriminant validity, high test-retest reliability, and consistent internal consistency in differentiating women with HSDD or other female sexual dysfunctions from those without, confirming the scale's effectiveness in measuring sexually related personal distress [15-16].The effectiveness of supervised and unsupervised PFMT was assessed in managing stress urinary incontinence (SUI) among women. The study utilized the Oxford Grading Scale to measure pelvic floor muscle strength, finding significant enhancements in muscle strength, overall quality of life, and reductions in urine loss for both training modalities [17]. There were successfully validated the Sexual Quality of Life-Female (SQOL-F) questionnaire with analysis confirmed the questionnaire's robust four-factor structure, making it a reliable tool for assessing female sexual quality of life in reproductive health care [18].The aim of the study is to assess the efficacy of a comprehensive treatment approach, which includes TTNS, biofeedback therapy, and the use of a Kegel device, in treating sexual dysfunction in women with neurological disorders.
2. Methods
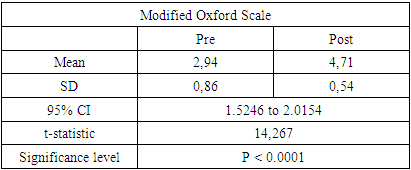
- The research took place at the 1st governmental hospital's clinic and Jacksoft MDS clinics, located in Tashkent, Uzbekistan. Participants were recruited and underwent testing from January 2022 through December 2024.This study included 133 women, ranging in age (Table 1) from 25 to 66 (45,0±11,6), with diagnosed neurological conditions.
|
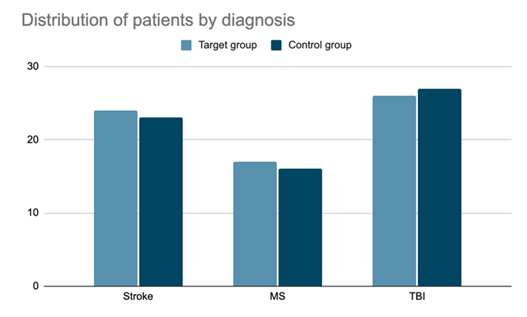 | Figure 1. Distribution of patients by diagnosis |
3. Results
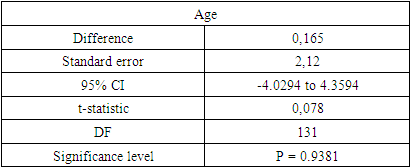
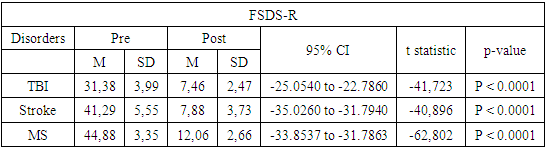
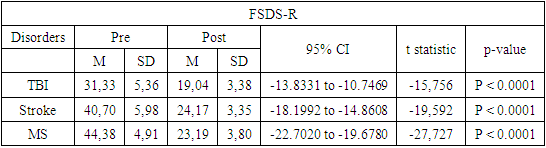
- The results for the target group in this study demonstrate more significant improvements compared to the control group in sexual function following the intervention. According to the FSDS-R, there were marked improvements across these neurological conditions. Before the intervention, mean scores for TBI patients were 31.38, which improved to 7.46 post-treatment. Similarly, stroke patients showed an improvement from an initial mean of 41.29 to 7.88, and MS patients improved from 44.88 to 12.06. The standard deviations also decreased, indicating a convergence of scores towards the mean improvement. Statistically, these results were highly significant with p-values less than 0.0001 across all conditions. The t-statistics were -41.723 for TBI, -40.896 for stroke, and -62.802 for MS, with confidence intervals strongly excluding zero, further substantiating the effectiveness of the treatment (Table 2).
|
|
|
|
|
|
4. Discussion
- In many regions, especially for women, cultural and societal constraints severely limit the ability to openly address sexual concerns, despite the well-documented fact that neurological disorders frequently lead to considerable instances of sexual dysfunction [20-23].The remarkable improvements observed in the target group, as demonstrated by the substantial changes in both the Modified Oxford Scale and the SQoL-F questionnaire scores, highlight the efficacy of integrating biofeedback techniques, TTNS, and Kegel device therapy into the treatment plan. Previous investigations have sought to determine the therapeutic effectiveness of individual treatments in comparison to control groups, resulting in varied outcomes. Nevertheless, as far as we are aware, no study has yet explored the comparative efficacy of these four therapies and their influence on the extensive array of anorectal physiological aspects [24-29].The results of the study demonstrate that PFMT, either as a standalone treatment or when integrated with intravaginal neuromuscular electrical stimulation (NMES) or TTNS, is effective in managing symptoms related to sexual dysfunction, often associated with urinary tract issues in women diagnosed with MS. Notably, the synergistic approach of combining PFMT with NMES exhibited superior efficacy in diminishing pelvic floor muscle tone and symptoms associated with an overactive bladder [30,31].Neurological impairments can lead to a range of issues including sensory deficits, motor function loss, and emotional disturbances, all of which can severely impact sexual function [32,33]. Traditional treatment modalities often fail to address these multifaceted challenges. However, comprehensive treatment approach that includes TTNS, biofeedback, and Kegel exercises can effectively target these diverse aspects [34-36]. The use of TTNS in the target group is notable for its role in enhancing neural function and facilitating the recovery of pelvic floor muscle control [37]. By stimulating the tibial nerve, TTNS can influence the neural pathways that are essential for maintaining pelvic floor strength and sexual function [38-41]. Biofeedback therapy, on the other hand, helps patients gain awareness and control over their physiological responses, enhancing their ability to manage and improve sexual function consciously [42]. Finally, the regular use of Kegel devices strengthens the pelvic floor muscles, which is vital for sexual health and urinary continence [43]. This integrative approach not only improves physical aspects of sexual function but also addresses the psychological and emotional dimensions [44]. The significant improvement in SQoL-F scores indicates that participants experienced not only physical benefits but also an enhanced perception of their sexual life, contributing to a better overall quality of life [45,46].
5. Conclusions
- This study underscores the importance of a comprehensive and integrative approach to managing sexual dysfunction in women with neurological disorders. The combination of TTNS, biofeedback techniques, and Kegel device therapy demonstrated efficacy, particularly in enhancing pelvic floor muscle strength and sexual quality of life. These improvements in the target group not only mitigate physical symptoms but also significantly boost the emotional and psychological well-being of the patients, thus elevating their overall quality of life. By laying a solid foundation for future research, this study emphasizes the critical need for all-encompassing treatment strategies to address the complexities of sexual dysfunction in individuals with neurological conditions effectively.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML