-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(6): 1632-1634
doi:10.5923/j.ajmms.20241406.34
Received: May 16, 2024; Accepted: Jun. 3, 2024; Published: Jun. 19, 2024

Studying the Effectiveness of Albendazole as a Local Germiticide after Liver Echinococcectomy
Davlatov Salim Sulaymonovich1, Rakhmanov Kosim Erdanovich2, Radjabov Jasur Pardabayevich2
1Bukhara State Medical Institute, Bukhara, Republic of Uzbekistan
2Samarkand State Medical University, Samarkand, Republic of Uzbekistan
Correspondence to: Rakhmanov Kosim Erdanovich, Samarkand State Medical University, Samarkand, Republic of Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

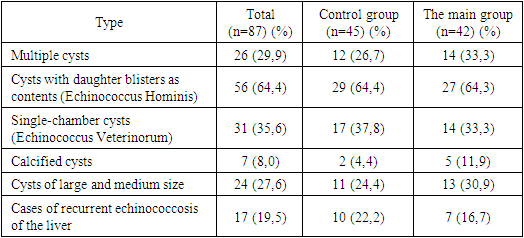
One of the most common causes of parasitic liver invasions found in surgical practice is echinococcosis. According to WHO, about three million people worldwide get sick with echinococcosis every year. Objective: The aim of the study is to improve the quality of treatment of patients with liver echinococcosis by using albendazole as a local germicide. Material and research methods. The clinical study consisted of 87 patients with liver echinococcus. Research results. The control group included 45 patients with liver echinococcosis who took. Albendazole according to the standard regimen. The main group included 42 patients with liver echinococcosis, who, along with oral administration of Albendazole in the postoperative period at a dose of 5 mg/kg/day, underwent antiparasitic contact treatment of the walls of the residual cavity with this drug according to our method. Conclusions. The use of small doses of Albendazole in combination with the use of this drug as a local germicidal agent according to the developed method showed a positive anti-relapse effect from their use.
Keywords: Liver echinococcosis, Local germicide, Relapse, Prevention
Cite this paper: Davlatov Salim Sulaymonovich, Rakhmanov Kosim Erdanovich, Radjabov Jasur Pardabayevich, Studying the Effectiveness of Albendazole as a Local Germiticide after Liver Echinococcectomy, American Journal of Medicine and Medical Sciences, Vol. 14 No. 6, 2024, pp. 1632-1634. doi: 10.5923/j.ajmms.20241406.34.
Article Outline
1. The Relevance of Research
- One of the most common causes of parasitic liver invasions found in surgical practice is echinococcosis [4,6]. According to WHO, about three million people worldwide get sick with echinococcosis every year. Uzbekistan is one of the regions endemic to echinococcosis. Climatic, geographical, social and economic conditions have traditionally developed in such a way that there are a number of zoonotic foci with varying degrees of intensity of epizootic processes on the territory of the republic. At the same time, the incidence of echinococcal disease in humans correlates directly with the intensity of the epizootic process in zoonotic foci. Currently, the surgical method of treating liver echinococcosis, in the vast majority of cases, is the method of choice [4,8,12]. However, the operation is a risk factor, which is determined by a number of reasons: the patient's condition, the localization of parasitic foci, the number of previous operations.Echinococcosis of the liver, being a serious disease, can be complicated by the development of recurrent cysts. Repeated surgical interventions in echinococcosis are technically very difficult, and under certain circumstances (multiple lesions and repeated relapses) lead to disability and even death of patients. A wide range of recurrence rates (from 3% to 54%), according to various authors, is due to many factors: the pathogenicity of the pathogen, the peculiarities of treatment and prevention. Unfortunately, to date, there is no unified approach to the etiological causes of relapse [1,3,10,15]. There are metastatic, implantation, residual, and invasive relapse theories. It is impossible to reliably determine the cause of the origin of recurrent cysts using currently existing methods. Rather, there are no reliable methods for determining the causes of relapse. The establishment of the cause of relapse will contribute to the correct choice of surgical treatment tactics and the effectiveness of prevention due to the "targeted" effect [1,9,14]. In connection with the above, the most significant and important in the prevention of relapses, regardless of the causes of their occurrence, is chemotherapy. Since 1983, the anthelmintic drug Albendazole, prescribed for the treatment and anti-relapse prevention of echinococcosis, has been widely used in the world. On the territory of the CIS countries, this drug was also recommended for use as a therapeutic and prophylactic agent during the congress of the Association of Hepatological Surgeons of Russia and the CIS countries in 2014 [2,3,7,11]. The following scheme of Albendazole application has become the most widespread: the drug is prescribed at a dose of 10-20 mg / kg of weight per day, the number of courses is from 3 to 10 with a break of 14-15 days. This scheme is consistent with the scheme proposed by Horton (1989) and approved by WHO [10,12].An analysis of international literature has shown that Albendazole, once in the human body, does not have a direct effect, but quickly undergoes biotransformation. Currently, it is known that in the human body albendazole (ABZ) is converted into albendazole sulfoxide (ABZ-CD), which has an anthelmintic effect. The latter, in turn, is metabolized into albendazole sulfone (ABZ-CH), which has no biological activity. Then, ABZ-CH is hydroxylated and is mostly excreted in bile and urine [5,8].The use of the drug has a number of side effects well described in the literature, which causes many patients to stop taking it prematurely. Known methods of preventing echinococcosis with Albendazole, depending on the severity of the course (solitary, multiple), according to the literature, show their effectiveness in the range of 40% - 70% [4]. This is due to the fact that the metabolism of Albendazole in the body proceeds differently due to the unique morphological, physiological and biochemical properties of each person due to genetic polymorphism [7,10].The proposed standard regimen of Albendazole (at a dose of 10-20 mg / kg of weight per day, the number of courses 3-10 per year with a break of 14-15 days, in practice, is used in different ways, since uniform criteria have not yet been developed, which also does not improve treatment results. Albendazole, local application of the drug as a contact germicide has become quite widespread, especially among surgeons who actively use minimally invasive techniques. As a rule, injection of a solution of 10% Albendazole and 20% hypertonic solution into the cyst cavity is used, followed by its aspiration or without it. Despite its simplicity of implementation, the technique has a number of negative aspects, manifested, among other things, in the form of suppurative processes.
2. Materials and Methods of Research
- In order to circumvent the negative aspects associated with the use of Albendazole in oral or injectable form, we have developed a chemotherapy technique based on contact antiparasitic treatment of liver tissue with Albendazole and oral administration of this drug in "small" doses (5 mg / kg / day) and conducted a study of its effectiveness in order to prevent recurrence of echinococcosis liver in patients admitted to the multidisciplinary clinic of the Samarkand State Medical University in the period from 2017 to 2020. The essence of the technique is that due to the tamponing of the wound surface of the liver with Spongostan sponge treated with Albendazole solution, a long-term local effect of the drug on the pathological focus is achieved. In accordance with it, we impregnated a sterile sponge sponge with a size of 7×5×1 cm with 50 ml of 0.9% saline solution with Albendazole dissolved in it at a concentration of 10 µg/mL (Fig. 1).
 | Figure 1. Treatment of the residual cavity after echinococcectomy from the liver with Spongostane sponge impregnated with albendazole |
|
3. The Results of the Study
- After discharge from the hospital, patients were taken under medical supervision with ultrasound, ELISA control and examination of biochemical parameters of the functional state of the liver (ALT, AST) every 6 months for 1.5-2 years. According to the results of the study, a recurrence of the disease occurred in 5 (11.1%) patients of the control group. There was no recurrence of the disease in patients from the main group. There were also no cases of local and general complications in patients treated according to our method.
4. Conclusions
- Despite the small volume of the study performed, the use of "small" doses of Albendazole in combination with the use of this drug as a topical germicidal agent according to the developed methodology showed the presence of a positive anti-relapse effect from their use.
Conflict of Interest
- The authors declare no conflicts of interest or special funding for the current study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML