-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(6): 1612-1617
doi:10.5923/j.ajmms.20241406.29
Received: May 7, 2024; Accepted: Jun. 1, 2024; Published: Jun. 19, 2024

Assessment of the Relationship between Clinical and Immunologic Parameters in Patients with Rheumatoid Arthritis
Babamuradova Zarrina Bakhtiyarovna1, Shodikulova Gulandom Zikriyaevna2
1Head of the Department of Internal Medicine, Pediatric Faculty, Samarkand State Medical University, Samarkand, Uzbekistan
2Head of the Department of Internal Medicine No. 3, Doctor of Medical Sciences, Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Babamuradova Zarrina Bakhtiyarovna, Head of the Department of Internal Medicine, Pediatric Faculty, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. Rheumatoid arthritis (RA) is one of the most common forms of rheumatologic pathology (0.5-1.3% of the total population), often developing in people of working age, leading to rapid formation of disability and reduced life expectancy of patients. The aim of the study was to investigate clinical and immunologic interrelationships in patients with rheumatoid arthritis. Material and methods. To solve the tasks set in the work, 125 RA patients (78% women, 22% men) were examined. The age of the patients ranged from 18 to 76 years (mean age 57.3±1.6 years). The early rheumatoid arthritis group consisted of 85 patients with disease duration from 1 to 12 months (mean duration was 9.7±1.4 months). The comparison group included 40 patients with disease duration of more than 1 year (mean duration was 11.7±1.8 years). The control group consisted of healthy people comparable in sex and age. Results of the study. At the first stage of the study, we studied the occurrence of signs characterizing the joint syndrome in RA at different stages of the disease course. These signs included the presence of arthralgias in the hand joints, swelling of at least 1 hand joint, symmetrical arthritis (defined as involvement of any joints within 1 anatomical zone), and swelling of at least 1 major joint (knee, ankle, elbow, shoulder). In addition, the incidence of arthritis of the small joints of the feet was assessed, as well as the presence and duration of morning stiffness. Conclusions. Thus, the identified features of cytokine status depending on the serologic variant according to ACCP are in good agreement with our data on the presence of an inverse correlation between clinical parameters of disease activity and the content of TNF-α and IL-4 in the serum of RRA patients and the known unfavorable prognostic value of antibodies to citrullinated proteins. The above changes may indicate in favor of the important diagnostic role of ACCP at the stage of early rheumatoid arthritis.
Keywords: Rheumatoid arthritis, Antibodies to citrullinated proteins, Proinflammatory cytokines
Cite this paper: Babamuradova Zarrina Bakhtiyarovna, Shodikulova Gulandom Zikriyaevna, Assessment of the Relationship between Clinical and Immunologic Parameters in Patients with Rheumatoid Arthritis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 6, 2024, pp. 1612-1617. doi: 10.5923/j.ajmms.20241406.29.
Article Outline
1. Introduction
- It is known that in recent years in the developed countries of the world there has been a significant increase in the incidence of diseases of the musculoskeletal system and, above all, inflammatory diseases of the joints. Of particular medical and social importance is rheumatoid arthritis (RA), which is a chronic systemic autoimmune disease of connective tissue, accompanied by a predominant lesion of peripheral joints with the development of erosive-destructive changes and ankylosing [1]. Rheumatoid arthritis is one of the most common forms of rheumatologic pathology (0.5-1.3% of the total population), often developing in people of working age, leading to rapid disability and decreased life expectancy of patients [2].Currently, the concept of early rheumatoid arthritis (ERA) - a conditional clinical and pathogenetic stage of the disease with the duration of active synovitis not more than 1 year, characterized by antigen-specific activation of SE4+ T-lymphocytes, hyperproduction of proinflammatory cytokines in the absence of a number of characteristic morphological features of this disease (formed pannus).The classical concepts of RA pathogenesis were based on several complementary ideas, including the following. First, the leading role in the initiation and maintenance of the immunoinflammatory process belongs to SB4 T cells [7,11,13]. Cells of monocytic-macrophage origin play a leading role in the local production of proinflammatory cytokines [9]. Destruction of articular cartilage and pannus formation at late stages of RA is caused by the development of autonomous non-immune mechanisms that determine "tumor-like" growth and proliferation of synovial tissue [8].It has been established that circulating immune complexes containing autoantibodies can cause hyperproduction by immunocompetent cells of a number of cytokines, in particular TNF-α, IL-1, IFN-α, which occurs in such autoimmune diseases as RA and systemic lupus erythematosus (SLE) [3-6]. It should be noted that so far there has been no direct evidence of the pathogenic role of rheumatoid factor and antibodies to cyclic citrullinated proteins (ACCP), the main families of autoantibodies found in RA patients.In-depth study of molecular targets of antifilaggrin antibodies allowed us to identify citrulline-containing fragments of the filaggrin molecule as antigenic epitopes. Citrulline is an unusual amino acid formed by the deamination of arginine by the enzyme peptidyl arginine deaminase and is incorporated into the structure of a number of proteins. The necessity of using a combination of peptides was determined by a wide spectrum of anti-citrulline antibodies presented in the serum of RA patients. The possibility of synthesis of ACCP by plasma cells of synovial membrane and synovial fluid in patients seropositive for these autoantibodies was shown [12]. Currently, ACCP are one of the most promising laboratory markers of rheumatoid arthritis, since the use of ELISA technique makes the test easily standardizable and allows quantitative consideration of the obtained result.At the same time, the American College of Rheumatologists (ACR) classification criteria used since 1987 do not allow to establish the diagnosis of early RA with high accuracy and differential diagnosis with other forms of arthritis. The only laboratory criterion, rheumatoid factor (RF), which is included in the ACR criteria, is often negative at the onset of the disease and is characterized by low specificity.It is proved that immune disorders in early rheumatoid arthritis are diverse and cover the cellular and humoral parts of the immune system. Of particular interest is the study of SB-antigens of lymphocytes, as well as indicators of the cytokine spectrum, which play a key role in the development of the immunoinflammatory process. In recent years, a number of studies have been devoted to the study of lymphocyte phenotype and cytokine immunity parameters, with only a few of them conducted at the early stage of RA. However, there have been no comprehensive studies of immunologic changes in RA in comparison with clinical parameters in dynamics. The system of anti-inflammatory cytokines attracts unremitting interest of researchers. This is due to the dominant ideas that among the mechanisms of immunoinflammatory process observed in autoimmune diseases, including rheumatoid arthritis, the most important is the balance between pro- and anti-inflammatory cytokine systems, rather than an isolated increase in any component of the proinflammatory link.The anti-inflammatory cytokines involved in the realization of synovitis primarily include IL-lα, IL-1β, IL-6, and TNF-α [10]. This group unites cytokines of predominantly monocytic-macrophage origin. These are key effector molecules that trigger most pathogenetic mechanisms of inflammation, including cell activation and proliferation, expression of adhesion molecules, adhesion mechanisms, destruction of bone and cartilage tissue, as well as affecting angiogenesis, which has been shown in many in vivo and in vitro models of inflammation.Thus, due to the absence of characteristic clinical and laboratory changes at the early stage of rheumatoid arthritis, verification of the diagnosis is often difficult, which raises the question of the need for further search for additional immunologic diagnostic criteria and predictors of an unfavorable clinical course of this disease.The aim of the study was to investigate the clinical-immunologic relationships in patients with rheumatoid arthritis.
2. Material and Methods
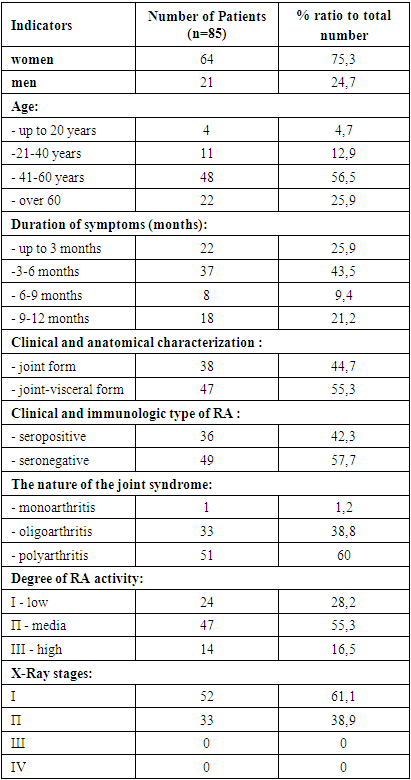
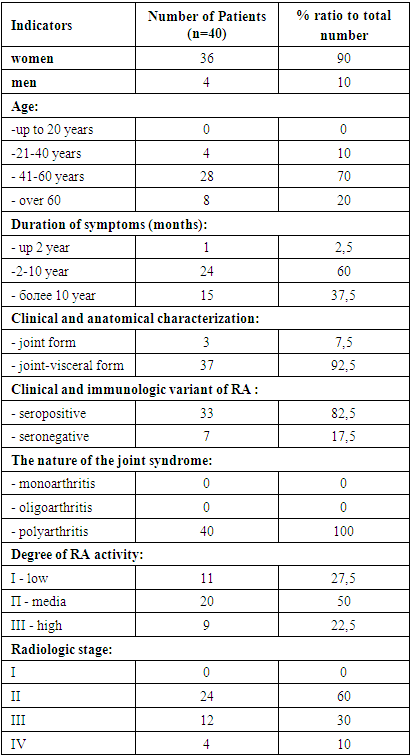
- To solve the tasks set in the work, 125 RA patients (78% women, 22% men) were examined. The age of the patients ranged from 18 to 76 years (mean age 57.3±1.6 years). The early rheumatoid arthritis group consisted of 85 patients with disease duration from 1 to 12 months (mean duration was 9.7±1.4 months). The comparison group included 40 patients with disease duration of more than 1 year (mean duration was 11.7±1.8 years). The control group consisted of healthy people comparable in sex and age (n=26).The clinical characteristics of patients with early RA are presented in Table 1.
|
|
|
3. Results of the Study
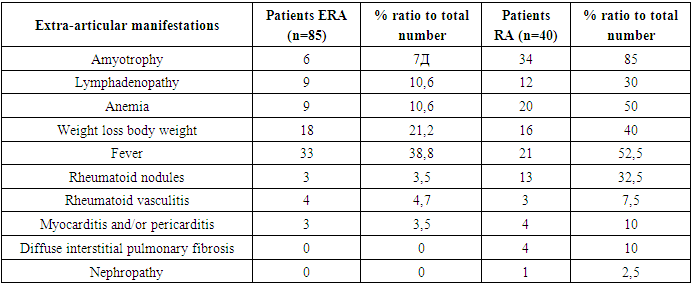
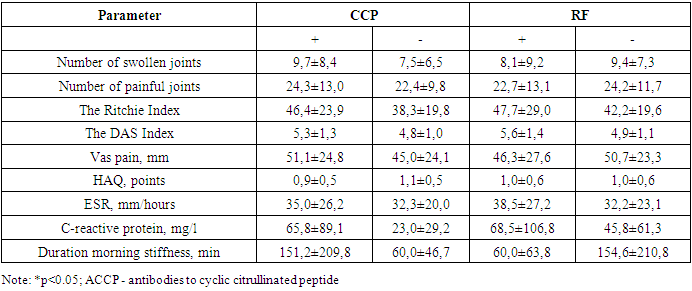
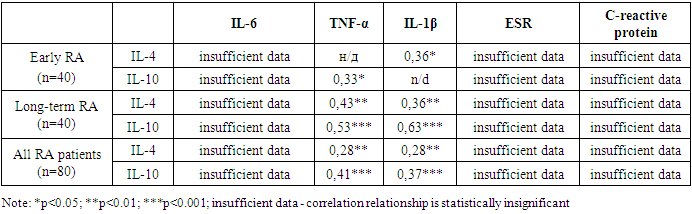
- At the first stage of the study, we studied the occurrence of signs characterizing the joint syndrome in RA at different stages of the disease course. These signs included the presence of arthralgias in the hand joints, swelling of at least 1 hand joint, symmetrical arthritis (defined as involvement of any joints within 1 anatomical zone), and swelling of at least 1 major joint (knee, ankle, elbow, shoulder). In addition, the incidence of arthritis of the small joints of the feet was assessed, as well as the presence and duration of morning stiffness. The frequency of the above signs was assessed at three points: from anamnesis during the first month from the onset of the joint syndrome (ascertained from the patient by filling out a formalized questionnaire), during examination by a rheumatologist in the process of establishing the diagnosis, and during prospective follow-up after 1 year.One of the most frequent symptoms of arthritis is pain in the affected joint - arthralgia. We evaluated the frequency of arthralgias of the hand joints in patients with early RA at different stages of the disease course.Arthralgias of small joints of the hands were described by 52.5% of patients in the main group during the first month of the disease, and by 92.5% of patients with early RA at the time of diagnosis verification. Differences in the frequency of this sign between patients at the debut of rheumatoid arthritis and at the time of diagnosis were highly statistically reliable (p<0.001). However, in patients under prospective follow-up for 1 year after diagnosis verification, we found a decrease in the occurrence of this symptom to 67.5%. Significant differences in the frequency of detection of these signs between the subgroups of patients with early RA at the time of diagnosis and after 1 year of prospective follow-up are also reliable (p<0.01). The differences between the subgroups of patients with early RA at the disease debut and after 1 year from the moment of diagnosis are not reliable.An important diagnostic sign of RA, along with symmetric lesions of small joints of the hands, is the involvement of small joints of the feet in the pathologic process. This is reflected in the well-known statement that "hands and feet are the visiting card of a patient with rheumatoid arthritis". The average duration of morning stiffness in patients with early RA was 20.3±29.4 minutes at the disease debut, 123.8±181.3 minutes at the time of diagnosis, and 105.7±114.8 minutes after 1 year of prospective follow-up. Differences between this index in RA patients at the disease debut and at the time of diagnosis were statistically reliable (p<0.01). We studied the occurrence of rheumatoid factor and ACCP. In patients with early rheumatoid arthritis, RF is detected in 44% of cases. At the same time, ACCP are detected much more frequently - in 62% of cases. Differences in the frequency of detection of these autoantibodies in patients of the main group are reliable in favor of ACCP (p<0.05). On the other hand, in patients with long-term rheumatoid arthritis the occurrence of RF and ACCP is 88% and 82%, respectively. When conducting a comparative study to establish relationships between the levels of ACCP and the severity of the joint syndrome assessed by the Ritchie index, DAS index, HAQ, VAS pain score, as well as the presence of systemic manifestations, we were able to identify significantly higher values of indicators characterizing the severity of the joint syndrome, as well as VAS pain parameters in ACCP -seropositive patients with RA.
|
|
4. Conclusions
- Thus, the identified features of cytokine status depending on the serologic variant according to ACCP are in good agreement with our data on the presence of an inverse correlation between clinical parameters of disease activity and the content of TNF-α and IL-4 in the serum of RRA patients and the known unfavorable prognostic value of antibodies to citrullinated proteins. The above changes may indicate in favor of the important diagnostic role of ACCP at the stage of early rheumatoid arthritis. Determination of cytokine immunity parameters, especially IL-1β, IL-4, IL-6, TNF-α, can be used to assess the degree of RA activity and as prognostic criteria.
Conflict of Interest
- The authors declare no conflicts of interest or special funding for the current study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML