Khamdamov Bakhtiyor Zarifovich1, Napasov Ilkhomjon Zubaydulloevich2
1Bukhara State Medical Institute, Bukhara, Uzbekistan
2Samarkand State Medical University, Uzbekistan
Correspondence to: Khamdamov Bakhtiyor Zarifovich, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Introduction. It is believed that a violation of bone regeneration in closed fractures of tubular bones, leading to the formation of a false joint, occurs in about 2% of all fractures, but with certain injuries this violation can reach 20%. The consequences of impaired bone regeneration in closed fractures of tubular bones, in the form of the formation of a false joint, in the UK is estimated at 20 per 100,000 population, with men of working age being the most common group. The aim of the study was to improve the results of immunological control and prediction of bone regeneration in patients with closed fractures of tubular bones. Materials and methods. The results of a comprehensive examination and treatment of 226 patients with closed fractures of long tubular bones were analyzed. All patients were treated and examined at the Samarkand branch of the Republican Specialized Scientific and Practical Medical Center for Traumatology and Orthopedics from 2017 to 2022 inclusive. The criteria for inclusion of patients in the study were: age of patients from 18 to 70 years; closed fracture of the femur or tibia; absence of concomitant diseases from the musculoskeletal system; absence of concomitant diseases in the acute stage; absence of local complications of bone fractures (vascular and nerve damage); absence of general complications of bone fractures (traumatic shock, fatty embolism and thromboembolism); use of surgical treatment methods. Results and their discussion. Analyzing the data on monitoring changes in cellular immunity during bone regeneration, it can be noted that in patients of the first subgroup, the uncomplicated course of bone regeneration was accompanied by a stable curve. At the same time, in patients of the second subgroup, regenerative processes of bone tissue, after a fracture, occurred with a double leveling in relation to the dynamics of patients of the first subgroup. Conclusions. To predict bone regeneration disorders in closed fractures of tubular bones, the optimal indicators are the integrated criteria of the ultrasound picture of the bone regeneration phase, the presence or absence of a local purulent-inflammatory complication and the studied indicators of cellular and humoral immunity. They served as the basis for the construction of the computational program IPBR (Method for predicting bone regeneration). At the same time, the prognostic probability of impaired bone regeneration can be divided into low and high. In the absence of a coincidence of the studied criteria with the developed software product, the probability of a violation of bone regulation is excluded.
Keywords:
Bone tissue, Fracture, Regeneration, Prognosis
Cite this paper: Khamdamov Bakhtiyor Zarifovich, Napasov Ilkhomjon Zubaydulloevich, The Role and Place of Methods for Predicting Bone Regeneration Disorders in Closed Fractures of Tubular Bones, American Journal of Medicine and Medical Sciences, Vol. 14 No. 6, 2024, pp. 1588-1602. doi: 10.5923/j.ajmms.20241406.26.
1. Introduction
It is believed that a violation of bone regeneration in closed fractures of tubular bones, leading to the formation of a false joint, occurs in about 2% of all fractures [1,3], but with certain injuries this violation can reach 20%.The consequences of impaired bone regeneration in closed fractures of tubular bones, in the form of the formation of a false joint [2,4,12], in the UK is estimated at 20 per 100,000 population, with men of working age being the most common group [10,13,14].The main problems associated with impaired bone regeneration in closed fractures of tubular bones are associated with prolonged pain syndrome, loss of limb function and mental stress conditions [5,7,15,16].The financial consequences can often be significant for patients due to the loss of potential earnings and estimated medical costs of up to 79,000 pounds for each possible case [6,8,17,18].Most often, a violation of bone regeneration, leading to the formation of a false joint, occurs with fractures of the bones of the forearm, humerus, tibia, collarbone and femur [9,11,19,20].The exact definition of false joints, as a result of impaired bone regeneration, is difficult. According to the definition of the US Food and Drug Administration, a fracture that is not joined 9 months after injury, or a fracture in which regeneration failed during the previous three months, can be classified as a violation with the formation of a false joint.However, 9 months is a long period of time during which patients wait for bone fracture regeneration. The specific length of time to identify a false joint should be related to the fracture site and the severity of the initial injury, two factors that will have a profound effect on the time of unification.In recent decades, scientists have focused on studying the close relationship between the immune system and bone tissue. So much close attention has led to the emergence of a new term – osteoimmunology [1,2,3]. To date, it has been convincingly proven that most components of the immune system, including numerous molecules, cytokines, chemokines, hormones, receptors and transcription factors, etc. have a close connection with the regenerative processes of bone tissue. Moreover, studies were conducted under both physiological and pathological conditions [5,9].To date, it is already known that the main immune cells interact with bone tissue as the main components of the system, and sometimes as auxiliary ones. In particular, it became known that T cells, as well as their auxiliary components, are actively involved in the regeneration of bone tissue and their auxiliary cells. First of all, this directly concerns the formation of the osteoclastogenesis process [2,4].There is information regarding the controlled role of cytokines in the process of bone tissue regeneration. Specific morphogenetic proteins and cytokines of tumor necrosis factor determine the process of bone regeneration [8,10,21,22].Cytokines produced by helper T cells also play an important role in osteoclastogenesis. IL-8 and IL-18, which induce Th1 cell differentiation, and INF-γ, a cytokine produced by Th1, together have an inhibitory effect on osteoclast formation. However, Th1 cells can also promote bone resorption by interfering with the connection of osteoclasts and osteoblasts through differentiation of TNFa osteoblasts. Cytokines produced by Th2, mainly IL-4 and IL-10, have an inhibitory effect on osteoclast formation [6,8,23,24].Inhibition of T cell activation suppresses induced T cell expression, which leads to inhibition of osteoclastogenesis [K. Wing, T. Yamaguchi, S. Sakaguchi, 2021]. It has been proven that T cells can influence osteoclastogenesis both indirectly and directly through the active secretion of IL-17, which leads to the secretion of TNF-α and IL-1, which, in turn, support osteoclastogenesis [11,25,26].Activated T cells induce osteoclastogenesis by directly affecting osteoclast progenitor cells. In contrast, resting T cells inhibit osteoclastogenesis through a mechanism that involves mediating the complete suppression of mechanisms by B cells. In addition, T cells can also differentiate into CD4 and CD8 T cells, which continue to affect osteoclastogenesis. CD4 T cells do not affect osteoclast formation, while depletion of CD8 T cells leads to an increase in osteoclast formation by 40% [5,7]. This suggests that differentiated T cells play a role primarily in promoting osteoclastogenesis.Thus, the importance of immunological aspects of predicting bone regeneration disorders in closed fractures of tubular bones, at the present level, becomes relevant both on fundamental issues and applied ones that affect the outcome of treatment in general.Meanwhile, to date, the peculiarities of changes in cellular and humoral immunity indicators in patients with closed fractures of tubular bones, depending on the outcome of bone regeneration, have not been studied. Along with this, analyzing the results of monitoring cellular-humoral immunity indicators and data from instrumental diagnostic methods in the process of bone tissue regeneration, in our opinion, would reveal many important aspects in predicting the outcome of the treatment. All of the above has determined the main direction of this work.
2. The Aim of the Study
The aim of the study was to improve the results of immunological control and prediction of bone regeneration in patients with closed fractures of tubular bones.
3. Materials and Methods
The results of a comprehensive examination and treatment of 226 patients with closed fractures of long tubular bones were analyzed. All patients were treated and examined at the Samarkand branch of the Republican Specialized Scientific and Practical Medical Center for Traumatology and Orthopedics from 2017 to 2022 inclusive. The criteria for inclusion of patients in the study were: age of patients from 18 to 70 years; closed fracture of the femur or tibia; absence of concomitant diseases from the musculoskeletal system; absence of concomitant diseases in the acute stage; absence of local complications of bone fractures (vascular and nerve damage); absence of general complications of bone fractures (traumatic shock, fatty embolism and thromboembolism); use of surgical treatment methods.We divided the clinical material into two groups: the control and the main one. The main group of patients consisted of 112 patients in whom clinical and immunological monitoring was used to predict bone tissue regeneration using the IPBR program developed by us ("Method for predicting bone tissue regeneration"). In the control group, against the background of the use of traditional methods for assessing bone tissue regeneration, the main parameters of cellular and humoral immunity were studied. The patients of young and mature age (61.5%) were male (77.4%). In the control group of patients in 71.1%, and in the main group in 74.1% of cases, the treatment of patients was for a closed fracture of the tibia. The remaining patients had closed femoral fractures (28.9% and 25.9%, respectively). In the control and main groups, household and street injuries were the main causes of tubular bone fractures (44.7% and 49.1%, respectively). The classification of M.E. Muller et al. was used in the diagnosis. (1996). All patients with fractures of long tubular bones were operated on. Intramedual osteosynthesis was used in 79 (35%) patients, bone (extramedual) osteosynthesis was used in 93 (41.2%) patients, and transosseous osteosynthesis using the Ilizarov apparatus was used in 54 (23.9%) patients. Each group of patients was divided into three subgroups depending on the course and outcome of treatment. The first subgroup consisted of patients who had no complications during the postoperative period with normal bone regeneration (39.8% of patients). The second group consisted of patients in whom the postoperative period proceeded with the development of a local purulent-inflammatory complication, and the outcome of treatment ended in a satisfactory condition (50.4%). The third subgroup consisted of patients who had impaired bone regeneration against the background of the development of postoperative local purulent-inflammatory complications.The research methods were comprehensive and conducted in accordance with the regulations approved by the Ministry of Health of the Republic of Uzbekistan standards of medical care for traumatological and orthopedic patients.The leukocyte reaction of the blood was evaluated by determining the populations of leukocytes in blood smears stained using the Romanovsky-Gimze method [T.N. Soboleva, E.B. Vladimirskaya, 2000].From the indicators of cellular immunity, the content of T-lymphocytes and B-lymphocytes was determined according to CD3+ and CD19+ indicators by the indirect immunofluorescence Merchant test using monoclonal antibodies of the CD series. Serum immunoglobulins were determined in a one-dimensional immunodiffusion reaction in agar gel using the Manzini method using monospecific sera against IgA, IgM, IgG (g/l).Quantitative determination of cytokine secretion (pg/ml) of IL-1α, IL-1β, IL-8, IL-10 and TNF-α was determined by sandwich enzyme immunoassay using standard monoclonal and polyclonal antibodies produced.The dynamics of bone fragment regeneration was evaluated using ultrasound diagnostics of the fracture zone in comparison with a healthy limb in the dynamics of the postoperative period.The studies were conducted on the day of the patient's visit to the clinic and in the postoperative period, broken down into certain periods for 3-10 days and 1, 3, 6 and 12 months after surgery.
4. Results and Their Discussion
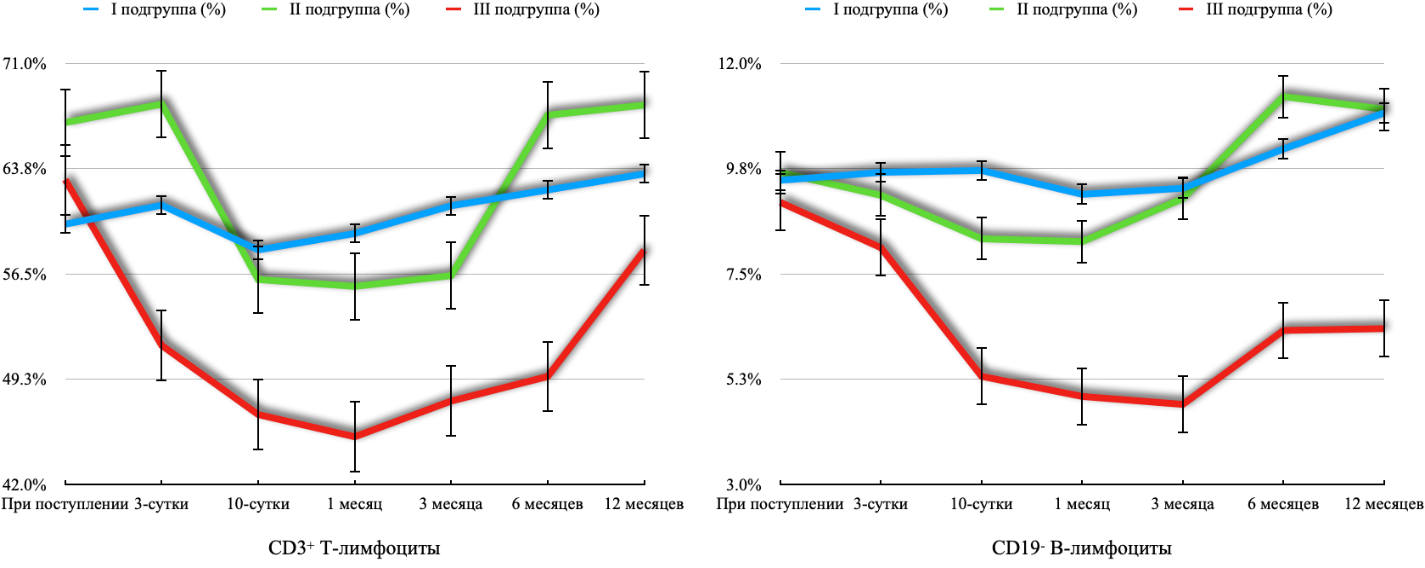
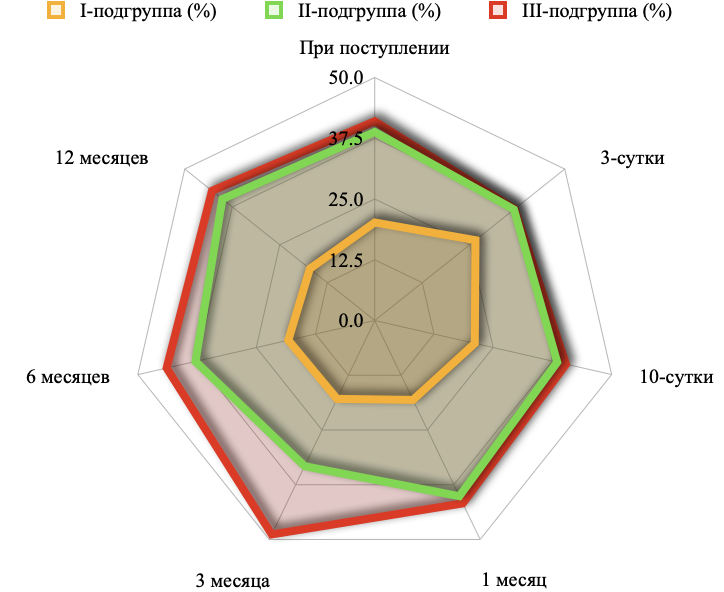
Analyzing the data on monitoring changes in cellular immunity during bone regeneration, it can be noted that in patients of the first subgroup, the uncomplicated course of bone regeneration was accompanied by a stable curve. At the same time, in patients of the second subgroup, regenerative processes of bone tissue, after a fracture, occurred with a double leveling in relation to the dynamics of patients of the first subgroup (Figure 1).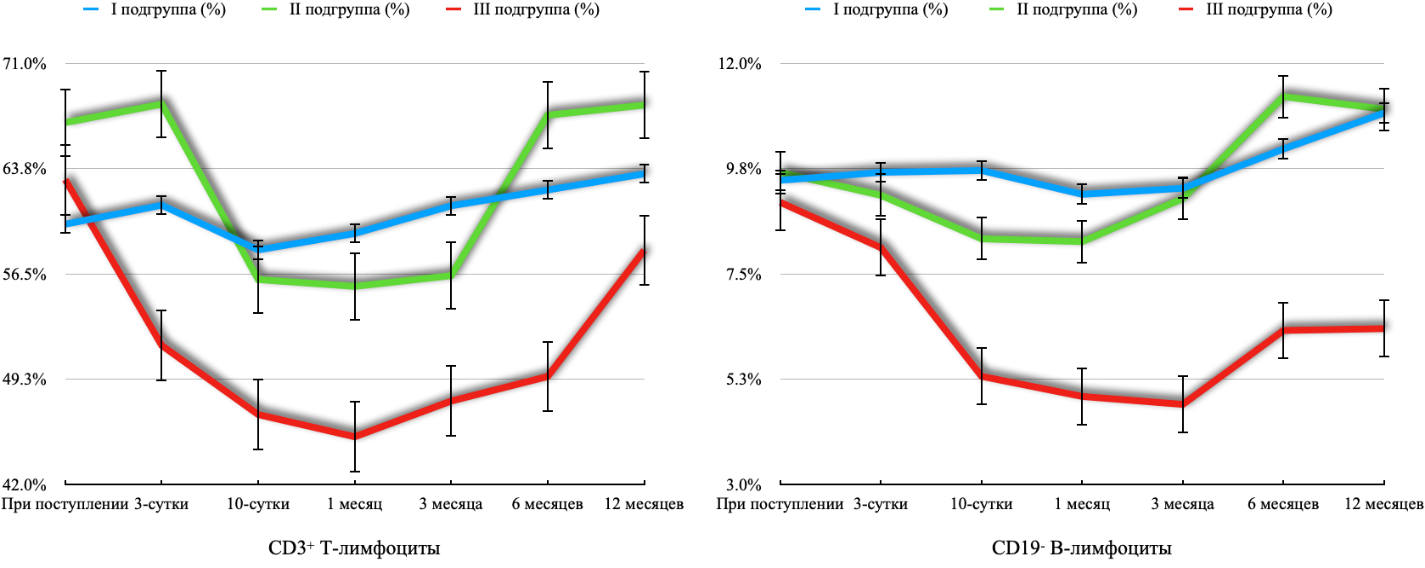 | Figure 1. Comparative assessment of the leveled curves of the number of cellular immunity indicators (%) in patients of various subgroups with fractures of long tubular bones in dynamics after osteosynthesis |
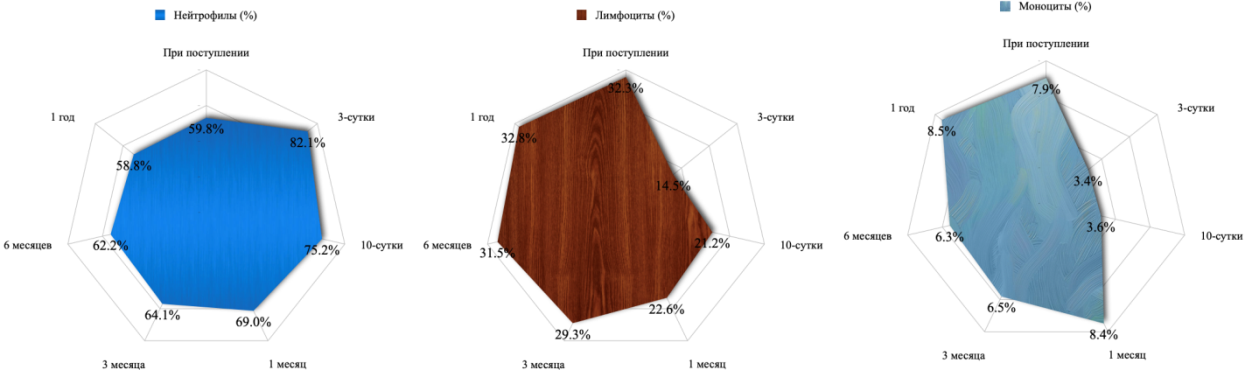
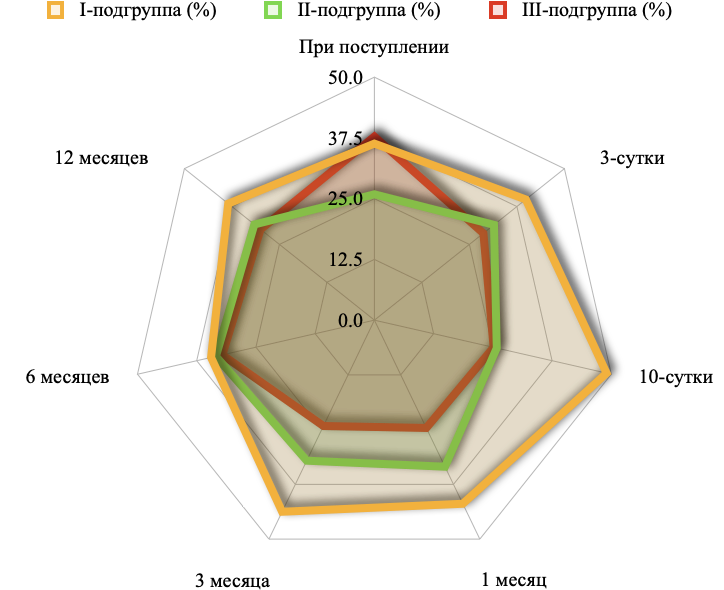
Leveling occurred during the development of a local purulent-inflammatory process, including osteomyelitis in the range of CD3+ T lymphocytes in the blood from 51.31% to 60.32%. Such a variation in the number of CD3+ T lymphocytes in the blood in patients of the second subgroup, apparently, made it possible to achieve normal consolidation of bone fracture even after suffering from chronic local purulent inflammatory disease. However, in patients of the third subgroup, the absence of recurrent leveling, unfortunately, did not lead to normal bone regeneration.Regarding the monitoring of changes in the number of CD19-B lymphocyte cells in the blood of patients of the second subgroup, the development of a local chronic purulent-inflammatory process led to a leveling of dynamics, the transition period of which occurred in the long-term period of regeneration of long tubular bones. We intentionally state this fact of leveling the dynamics of the curve, since in patients of the third subgroup such a character was not manifested by a graphical mane. A progressive decrease in the number of CD19-B lymphocyte cells in the blood of patients of the third subgroup was characteristic of impaired regeneration after osteosynthesis of long tubular bones.The dynamics of changes in the concentration of Ig-A in the blood of patients with impaired bone regeneration was characterized by a decrease in this indicator, which did not have the possibility of reaching the initial level back.However, judging by the dynamics of changes in the concentration of Ig-M in the blood of patients of the first subgroup, it can be stated that the high value of its production led to increased bone regeneration, creating conditions for satisfactory results in the treatment of long tubular bone fractures.In patients of the third subgroup, a pronounced progressive decrease in Ig-M in the blood was accompanied by the development of not only a local chronic purulent-inflammatory complication, but also a violation of bone regeneration.The average concentration of Ig-M in patients of the third subgroup was exactly 2 times lower than in patients of the first subgroup (p<0.05), which may indicate the key character of this indicator in predicting the outcome of regeneration of long tubular bones.Judging by the concentration curves, it is possible to notice a double leveling of Ig-G in the blood of patients of the third subgroup. The first leveling occurring in the early period of bone tissue regeneration was characterized by a low concentration of Ig-G, which, apparently, was associated with the development of local chronic purulent-inflammatory complications after bone osteosynthesis. Subsequently, as the postoperative period progressed, the concentration of this immunoglobulin increased, which exceeded both the initial values and the values of the first and second subgroups, which, apparently, was associated with the development of chronic inflammatory processes with impaired regeneration of long tubular bones.The studied cytokine profile in patients with closed fractures of long tubular bones allowed us to identify certain patterns of dynamics when dividing them into subgroups.The concentration of IL-1α, IL-1β and TNF-α levels in the blood at the maximum value made it possible to achieve bone regeneration without the development of local purulent-inflammatory complications, whereas a lack of abundance in the release of this cytokine led to the development of chronic osteomyelitis and a slowdown in the formation of calluses.The identical dynamics of the IL-8 concentration curve was noted by us in patients of all subgroups. In patients of the first subgroup, the level of increase was maximum (p<0.05). Its increase was 9.67 times compared to the initial value.A very ambiguous picture of changes in concentration curves was found among patients with closed fractures of long tubular bones in the study of the anti-inflammatory cytokine IL-10 in the blood. An increase in the concentration of this cytokine in the blood of patients with the development of local chronic purulent-inflammatory complications (second and third subgroups) reflects an anti-inflammatory response. At the same time, in patients of the second subgroup, it was higher than in the third, which probably served as the main reason for normal bone regeneration despite the development of a local chronic purulent-inflammatory complication. In contrast to the dynamics of proinflammatory cytokines, it can be noted that in relation to patients of the third subgroup, the value of these indicators has a reliable prognostic value.The dynamics of changes in the leukocyte blood reaction in patients of the first subgroup was characterized by relative stability of changes, which is confirmed by the lack of comparative reliable values.In patients of the second subgroup, the relative increase (compared with the first subgroup) of the leukocyte reaction was not characterized by a certain regular reaction, which confirms the low prognostic significance of using this method of analysis.In comparison with the period of the first study of the level of lymphocytes and monocytes in patients admitted to the clinic with closed fractures of long tubular bones, on the 3rd day after surgery, relative lymphopenia (2.2 times) and monocytopenia (1.5 times) were noted – Figure 2.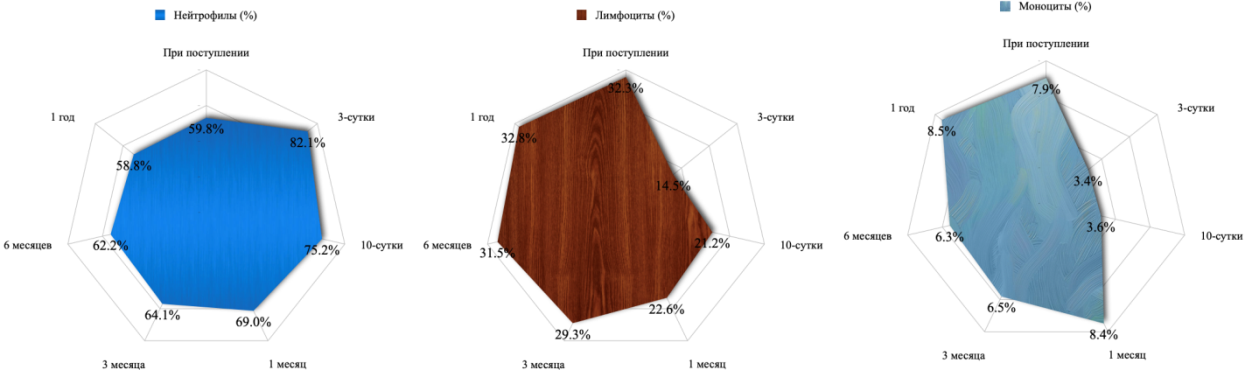 | Figure 2. Percentage ratio of leukocyte populations in patients with impaired bone regeneration in dynamics after osteosynthesis |
In patients with impaired bone regeneration, compared with patients with a normal treatment outcome, we revealed a pattern of changes in the leukocyte response by type of inflammatory character in a more pronounced variant. At the same time, the registered leukocytosis was characterized by a shift of the leukocyte formula to the left in the early stages after surgery. This was due to the development of purulent-inflammatory complications from the wound.Meanwhile, we also noted a similar pattern of changes in the early stages after surgery among patients of the second subgroup, who also experienced the development of a postoperative complication of a chronic purulent-inflammatory nature.However, as we have learned, bone regenerative processes were not disrupted in patients of the second subgroup. Most likely, in relation to the mechanism of formation of this pathological process and the corresponding leukocyte reaction of the blood, it is necessary to look for late treatment of patients. Moreover, it seems to us that we can get a similar answer when evaluating changes in leukocyte indices.Throughout the study, the predominant share in the organization of the level of leukocyte intoxication index belonged to patients of the second and third subgroups (Figure 3).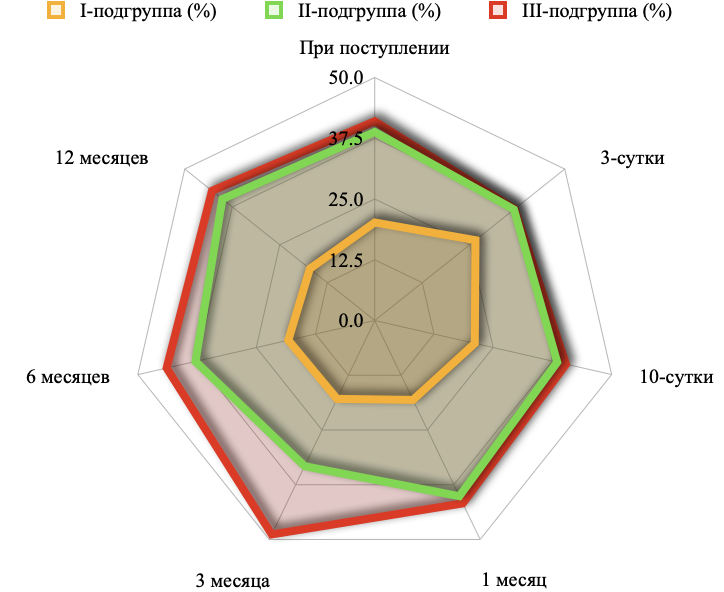 | Figure 3. The nature of the change in the percentage of leukocyte intoxication index in patients by subgroups in dynamics after osteosynthesis |
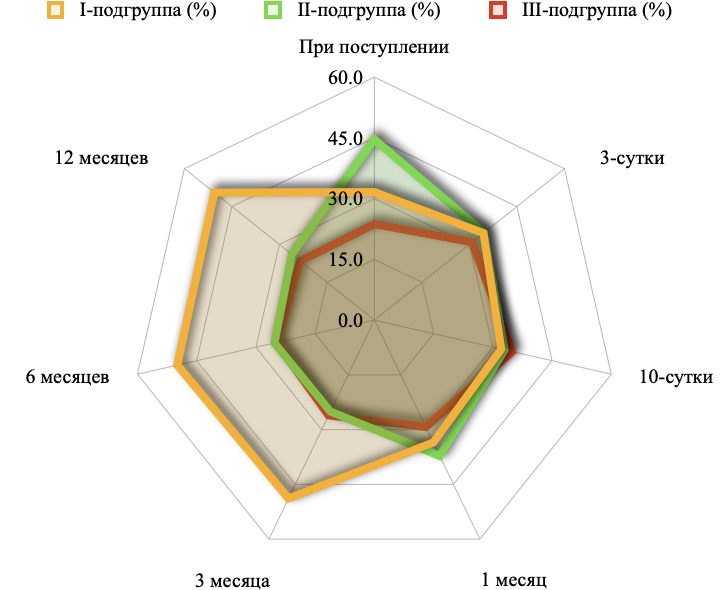
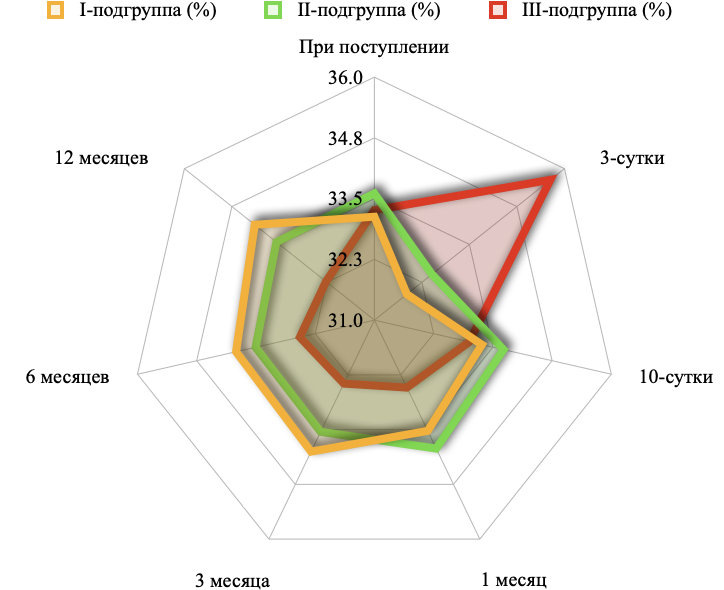
When patients were admitted to the clinic, the percentage of the total leukocyte intoxication index in the first subgroup of patients was 20.2%, in the second – 38.8%, and in the third subgroup – 41.0%.On the 3rd day after surgery, with a relative increase to 26.5% in the proportion of leukocyte intoxication index in the first subgroup of patients, there was a decrease in the second subgroup to 36.6% and to 36.8% in the third subgroup of patients.On the 10th day after osteosynthesis, the balance of the leukocyte intoxication index ratio changes again as in the time when patients are admitted to the clinic. At the same time, in the first subgroup of patients, the value of the leukocyte intoxication index decreased to 21.1%, and in the second and third subgroups it increased to 38.5% and 40.4%, respectively. Starting from this period, the trend no longer changed and against the background of a decrease in the proportion of leukocyte intoxication index in the first subgroup of patients, it only increased among patients of the second and third subgroups.A comparative assessment of laboratory parameters during the regeneration of a fracture of long tubular bones did not show the presence of high reliability between subgroups, especially in leukograms. However, when analyzing the reliability of the leukocyte intoxication index, reliable values were revealed in relation to patients of the first subgroup, which confirms the similarity of changes among patients of the second and third subgroups. This, apparently, can be recognized as a pattern, since such an assessment reflects the nonspecific reaction of leukocytes and the formation of cell populations. It became possible to evaluate such a reaction by calculating the leukocyte intoxication index.The similarity of changes in the leukocyte intoxication index among patients of the second and third subgroups indicates the identity of the body's responses, which coincided with the development of lymphopenia.The tendency to high monocyte values in the early stages after a closed fracture of long tubular bones and in the early postoperative period, apparently, was associated with the scale of traumatic injury. Such an assumption can be made based on the importance of monocytes in the regulation of macrophage reaction and, accordingly, osteogenesis.The high value of the leukocyte intoxication index that we identified remains interesting, which directly indicated the presence of a purulent-inflammatory process in the postoperative period. It is also interesting that this indicator has been growing for a long period after injury and surgery, which was noted among patients of both the second and third subgroups. The noted changes in the leukocyte reaction of the blood in closed fracture of long tubular bones, apparently, were also associated with the peculiarities of healing of long tubular bones. This fact should be taken into account when conducting prognostic monitoring in the treatment of patients with closed fractures of long tubular bones.The average proportion of the distribution of the leukocyte allergization index among patients with fractures of long tubular bones showed that in 40.54% of cases, the level of this indicator was the maximum level of this indicator in patients of the first subgroup. At the same time, it was 25.0% in patients of the second subgroup, and 31.3% among patients of the third subgroup (Figure 4). The peak of the leukocyte allergization index in patients of the first subgroup occurred on the 10th day after osteosynthesis surgery (49%), which accounted for almost half of all values in patients with fractures of long tubular bones. The minimum fractional level of the leukocyte allergization index in patients of the first subgroup was registered by us for a period of 6 months during the regenerative process of bones. Nevertheless, this indicator level still exceeded the proportion value than among patients of the second (33.4%) and third (32.1%) subgroups.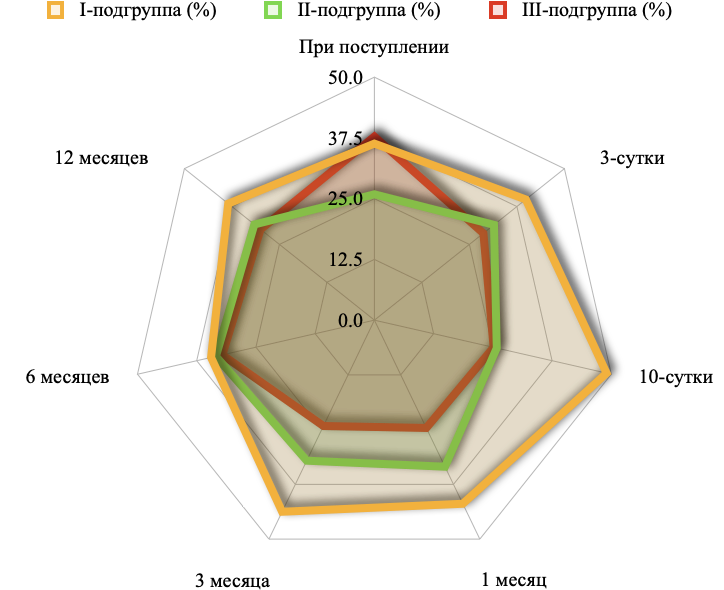 | Figure 4. The nature of the change in the percentage of leukocyte allergization index in patients with fractures of long tubular bones and in the context of subgroups in dynamics after osteosynthesis |
Thus, the leukocyte allergization index was not manifested in patients with purulent-inflammatory complications of osteosynthesis, both during the chronic process and impaired bone regeneration. The fact of high values of this indicator in patients with closed fractures of long tubular bones even before surgical treatment remains interesting.The data of patients of the third subgroup played an important role in the organization of the value of the nuclear leukocyte shift index.Most of these transformations could be noted in patients of the third subgroup on day 3-10 of bone tissue regeneration (64.3% and 57.1%, respectively).During 1-3 months, in patients of the third subgroup, the proportion of the organization of the value of the nuclear leukocyte shift index was equal to half (50%). Against this background, in the subsequent periods of bone tissue regeneration, a stable identical value can be observed in both the first and second subgroups of patients during 3-12 months of bone tissue regeneration. All possible changes in the level of the nuclear leukocyte shift index in the second subgroup of patients could be noted only in the early stages after osteosynthesis.Thus, the analysis of the leukocyte reaction of blood in patients with closed fractures of long tubular bones and in dynamics after osteosynthesis allows us to draw certain conclusions regarding their informational possibilities in predicting violations of bone consolidation. First of all, it should be noted that immune disorders in the body are most pronounced in the early stages after osteosynthesis, especially in patients with purulent-inflammatory complications in the form of suppuration of a postoperative wound and/ or the development of osteomyelitis, which is apparently associated with activation of leukopoiesis. Such a conclusion can also be made based on the ongoing changes in the nuclear shift index, which was associated with shifts in the immunological reactivity of the body in patients with impaired bone regeneration after fracture and osteosynthesis.Also, the indicators of the leukocyte intoxication index and the studied leukocyte populations can directly indicate signs of endogenous intoxication in the early stages of the development of purulent-inflammatory complications from wounds and long tubular bones.The average level of phagocytic activity in patients with closed fractures of long tubular bones throughout the dynamic study was 87.45±4.13%. The minimum average level of phagocytic activity occurred at the time of admission of patients to the clinic (86.46±3.49%) and 12 months after osteosynthesis (85.85±3.55%). This indicated, perhaps, the completion of phagocytosis processes in connection with the formation of a bone callus.The peak values of average phagocytic activity in patients with closed fractures of long tubular bones occurred during the period 3-90 days after osteosynthesis surgery. Such phagocyte activity was manifested already on the 3rd day after surgery in the form of an increase in its level to 90.40 ± 4.35%.Thus, the phagocytic index in patients with closed fractures of long tubular bones was characterized by wave-like changes, demonstrating activation in the early period of callus formation with a decrease in the indicators already in the process of completing the consolidation of bone fragments.In patients of the first subgroup, 2 characteristic periods of phagocytic index changes can be noted, in the form of a gradual increase in the early stages of bone marrow formation (up to 3 months after surgery), followed by stabilization of the curve at the end of regenerative processes. And even a year after the operation, in the case of bone regeneration without the development of any complications, the phagocytic index remains above the initial values, which, apparently, was associated with the transformation of the hematopoietic process in the bone marrow.The dynamics of changes in the phagocytic index in patients of the second subgroup, where normal bone consolidation occurred against the background of the development of purulent-inflammatory complications, also had a two-phase course. However, the phagocytic index in patients of the second subgroup was leveled in relation to the dynamics of patients of the first subgroup.We did not find any special difference between the subgroups in the share in the formation of the phagocytic index value of all patients with fractures of long tubular bones (Figure 5).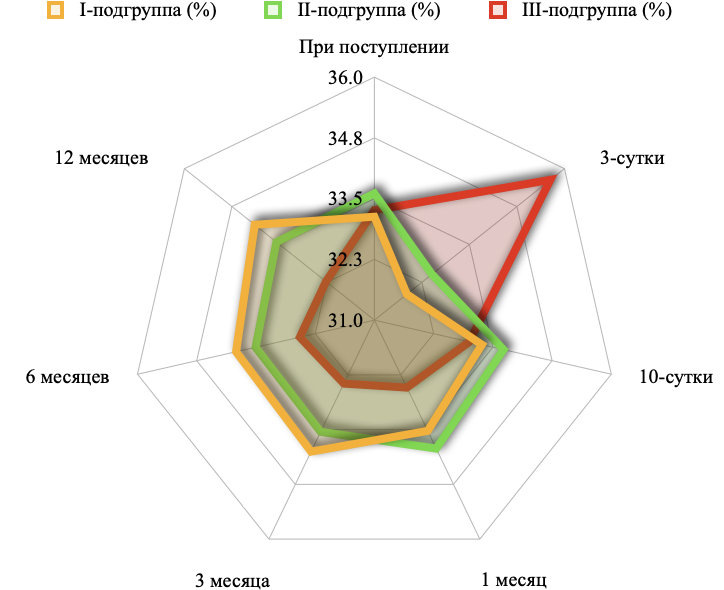 | Figure 5. The nature of the change in the percentage ratio of the phagocytic index in patients with closed fractures of long tubular bones in the context of subgroups in dynamics after osteosynthesis |
It should only be noted: the presence of a peak proportion of phagocytic activity among patients of the third subgroup on the 3rd day after osteosynthesis (35.6%); an increase in the proportion due to patients of the second subgroup in the early stages after surgery on 10-30 days (33.7% and 33.9%, respectively); a stable high proportion value during subsequent periods of treatment, up to a distant period. Thus, regarding the dynamics of changes in the phagocytic index, it can be noted that there is a differentiated manifestation in the randomized separation of patients depending on the course and outcome of the disease. At the same time, in patients with impaired bone regeneration, the phagocytic index does not change once, reflecting only the processes of development of a chronic inflammatory process against the background of a low immunological reaction of neutrophils.Regarding the percentage of the share of the number of phagocytes in the context of subgroups, priority can be noted in the second subgroup of patients (on average 35.4%), with the exception of 3 days after osteosynthesis, where the leading role was occupied by patients of the third subgroup (37.6%). Thus, drawing parallels between changes in phagocytic activity and the number of phagocytes, a certain correspondence can be noted. With a stable number of macrophages, the activity index changed in patients with different outcomes of bone regeneration. This indicates the activation of functional activity over hematopoietic, which, apparently, was associated with the transfer of cell formation towards osteoclasts and osteoblasts. Such changes contribute not only to the formation of a callus, but also, although indirectly, indicate the course of regenerative processes.A comparative change in the metabolic activity of phagocytes showed that the main increase in the metabolic activity of macrophages occurred in patients with purulent-inflammatory complications – 72.1% (Figure 6). Such changes intersected, creating an identical pattern of changes in the metabolic activity of phagocytes. However, in the long-term periods of treatment, starting from the 3-month treatment period, the entire priority in the proportion of the level of metabolic activity of phagocytes was determined by patients of the first subgroup (48.9%, 49.9% and 50.5%, respectively, at 3, 6 and 12 months of the study).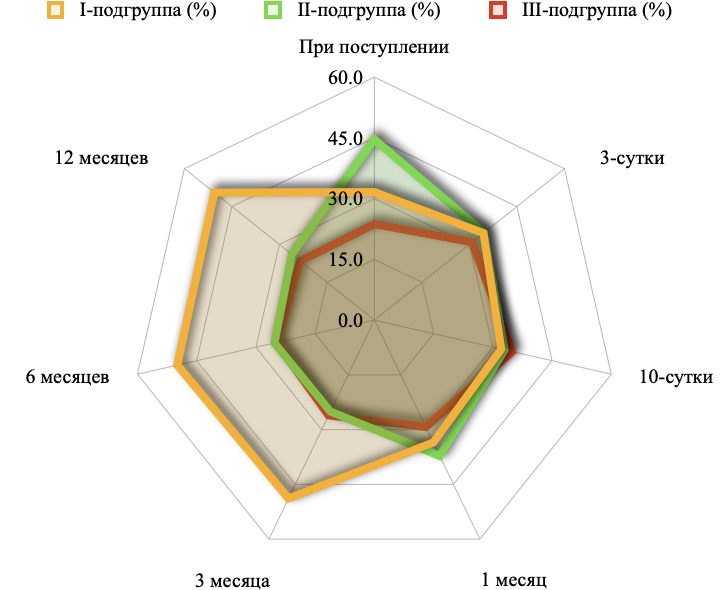 | Figure 6. The nature of the change in the percentage of metabolic activity of phagocytes in patients with closed fractures of long tubular bones in the context of subgroups in dynamics after osteosynthesis |
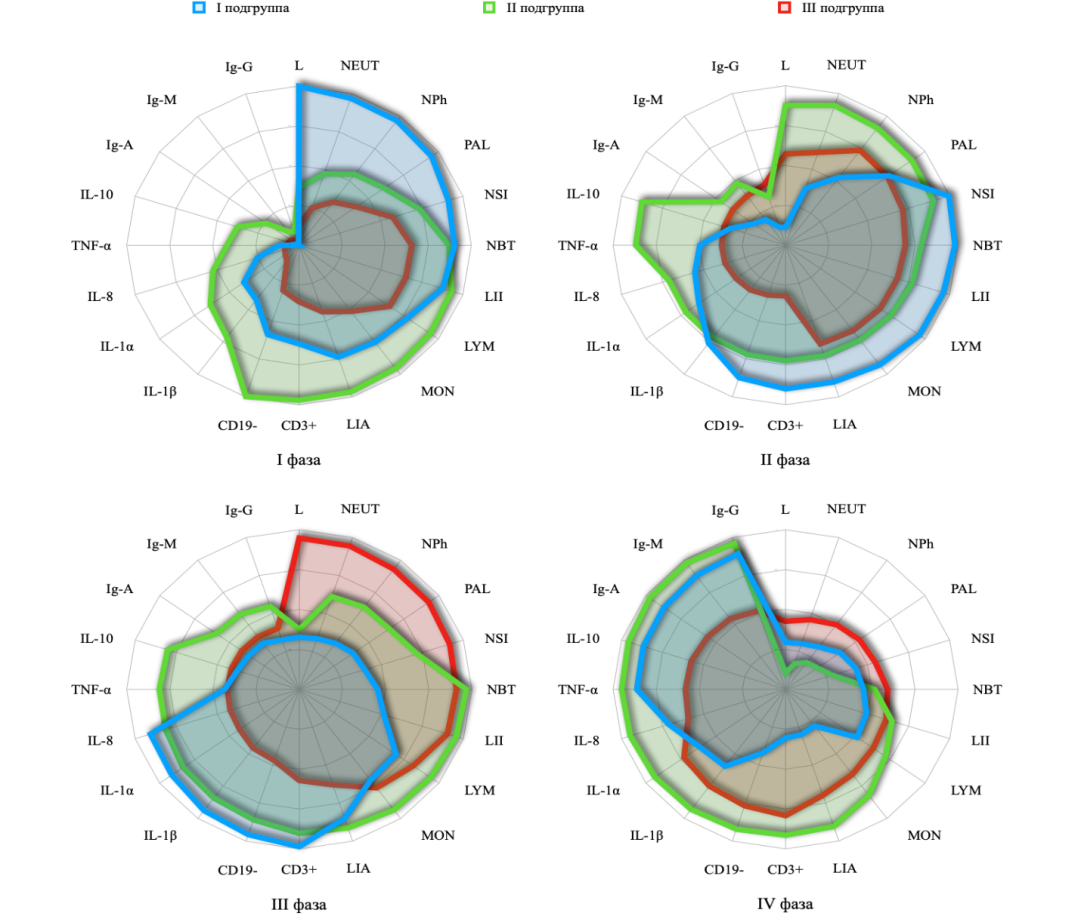
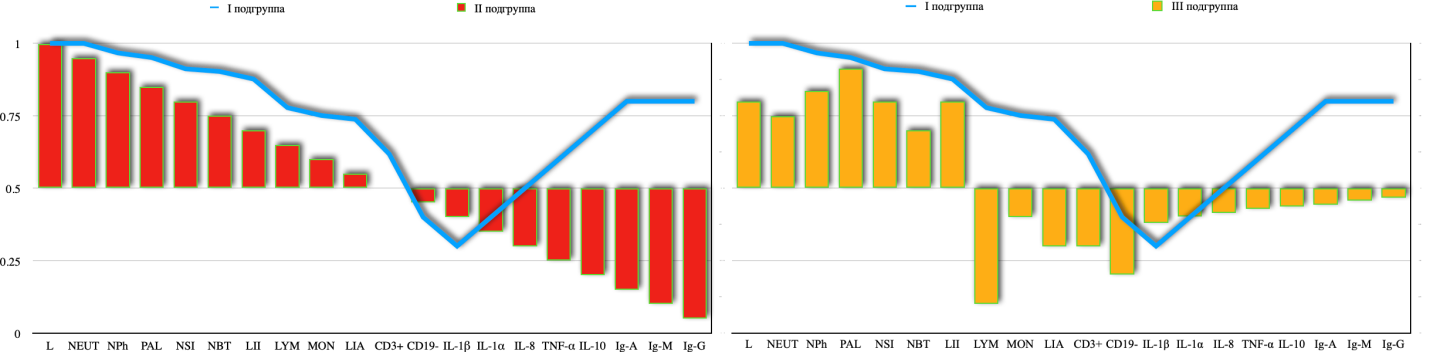
Thus, changes in the results of monitoring indicators of cellular and humoral immunity and ultrasound diagnostics of the fracture zone during bone tissue regeneration are of a phase nature in the form of acute circulatory disorders and increased leukocyte blood reaction, increased phagocytic activity and active production of lymphocyte subpopulations; periosteal reaction with increased vascularization in the fracture zone, the formation of an immunological response involving leukocyte subpopulations, with active expression of T-lymphocytes and B-lymphocytes, increased metabolic activity of macrophages and other leukocyte populations; formation of bone-cartilaginous corns and a fully formed cellular and humoral immune response of the body (expression of T-lymphocytes and B-lymphocytes against the background of active release of proinflammatory cytokines; the formation of a bone marrow against the background of the completion of the production of immunoglobulins and anti-inflammatory cytokines.The clinical and immunological comparison of the course of regenerative processes of bone tissue, carried out on the basis of comparing the data of ultrasound examination of the fracture zone and the information obtained from monitoring changes in immunological parameters of blood, allowed us to identify a number of features of the immunological reaction of the body. This, to a certain extent, reflects the peculiarities of the course of bone tissue regeneration, which can be interpreted as possible effective prognostic markers. To carry out such an assessment, the most effective may be the application of principles and analyses based on the rules of evidence-based medicine.The development of a method for predicting impaired bone regeneration was carried out by correlation and factor analysis. To identify the factors that determine the process of bone tissue regeneration, we gave a visual assessment of the dynamics of the formation of a bone callus.It was revealed that in patients after extramedullary osteosynthesis in the early postoperative period (3 days), ultrasound examination of the fracture zone revealed the presence of an interruption of periosteal echoes 2-4 mm in size in the direction of the fracture line. There was swelling of all layers in the soft tissues around the fracture zone, but to a greater extent in subcutaneous fat. Compared with healthy areas of soft tissues, soft tissues in the fracture zone had an intermittent character, which were combined with high and low signals of echogenic path formation. There were no signs of blood accumulation in the fracture zone and in the area of the postoperative wound. The extramedullary structure for osteosynthesis is visualized in full contour, with smooth edges. The presence of small vessels with their different types is traced.In patients with intramedullary osteosynthesis, an interruption of the high sound signal in the periosteal zone was detected. In most cases, it was variable in the form of steps. The area of the fracture line is traced by a linear image with jagged contours. The furrow of the fracture line, between the clearly traceable bone ends, has a regular shape with a thickness of 2.1 ± 0.4 cm. Fragments of fractures of increased echogenicity located around the fracture line averaged up to 28.1±1.2 mm in volume. Their shape was not even, which is usually considered characteristic of bone fragments. The contours of soft tissues, especially in the area around the bone fracture zone, do not have clear boundaries. The structure of the soft tissues is not uniform, edematous. Areas of formed hematomas were visualized between the muscles and in the bone fracture zone. Their boundaries were clearly traced, however, in some cases it was possible to notice the spread of accumulated blood at a short distance into the intermuscular space. Ultrasound assessment of the blood supply in the fracture zone showed no signs of angiogenesis.During 7-10 days after surgery, ultrasound examination of the fracture zone showed no fundamental differences compared to the previous period, except for a local increase in the number of microvessels by 1.8 times in patients with extramedullary osteosynthesis and 2.6 times in patients with intramedullary osteosynthesis. The blood flow through these vessels in patients with extramedullary osteosynthesis, compared with the previous period, indicated the achievement of relative maturity. This sign was considered as a positive dynamics of changes, which differed from the visual data in patients with extramedullary osteosynthesis. We considered this feature as the formation of primary bone fusion. Externally, the local pattern of the skin was characterized by obvious hyperemia, which was associated with vascular germination and restoration of microcirculation in the fracture zone.In patients with intramedullary osteosynthesis, clear edges of the fracture zone were still visible at this time. Bone fragments could also be clearly visualized around. Along with this, the space between the bone ends was filled with a low sound formation. The area of the vascular growth increased, exceeding the initial values by 2.5 times.1 month after extramedullary osteosynthesis, the structure of soft tissues in the fracture zone acquires an anatomical one. This was due to a decrease in local tissue and interstitial edema and hematoma lysis. The surfaces of the bone fragments were smoothed and, along with this, there was a significant narrowing of the fracture line. In the area of bone fragment diastasis, ultrasound examination begins to produce low echogenicity signals. This feature can be considered as the formation of an increase in the area of bone fragments. Vascular growth continues, but not as intensively as on the first day after surgery. Similar changes could be noted in patients after intramedullary osteosynthesis. However, in the fracture zone, the formation of a cartilaginous callus was clearly traced, which, on ultrasound examination, revealed a structure of low echogenicity compared to other parts of a healthy bone. The same signal could be detected over fragments of bone fragments, which were also characterized by the formation of bone-cartilaginous junctions. All soft tissues, including subcutaneous adipose tissue, according to ultrasound examination did not differ in their structure in comparison with the opposite (healthy limb).The dynamics of visual control of bone fragment repair in patients with extramedullary osteosynthesis continued its tendency to decrease the fracture furrow after 2 months. At the same time, the area of the regenerative pattern increased according to the echocarts. The amount of vascular germination increased significantly, in the order of 3.6 times compared to the previous observation period. The increase in the area of cartilaginous callus formation and the growth of blood vessels in the fracture zone directly indicated the ongoing process of bone regeneration after the imposition of an extramedullary structure. Similar changes were noted by us after intramedullary osteosynthesis, which indicated the formation of a regeneration zone. The same changes were typical for patients after intramedullary osteosynthesis. The regeneration zone increased in size compared to the previous study period, acquiring increased echogenicity. However, low-level echogenic signals still persisted.3 months after the operation, the bone groove was not visualized both in the fracture zone and in the area of bone fragments. The bone density acquired the same character. Vascular localization decreased. In a number of patients, signs of callus formation could be detected. This pattern was characterized by a decrease in echogenic signals, the reinfused part of the callus had a linear shape. It could completely cover the fracture zone and spread both above and below the structure.Starting from 6 months after surgery and in the subsequent period up to 1 year, the changes were identical in both patients with extramedullary and intramedullary osteosynthesis. The bone callus in the fracture zone acquired a continuous character of echogenicity throughout. In patients with intramedullary osteosynthesis, density increased in the area of callus formation against the background of a decrease in the number of germinating vessels.In the long term, the callus overlapped the defect area throughout. This type of echogenic changes was typical for patients with a normal course of the regenerative process.Thus, visual control of bone regeneration in patients with fractures of tubular bones revealed the division of the process into 4 phases.The first phase is characterized by acute circulatory disorders in the fracture zone of long tubular bones, with the formation of hematomas and compression of soft tissues, which contributes to the development of autocompression.The second phase of the regenerative process is characterized by the prevalence of vascular changes, which were more manifested both by their formation and active growth. At the same time, the growth activity depended on the type of osteosynthesis. Extramedullary osteosynthesis, due to the extended preservation of the bone marrow, manifested greater activity of angiogenesis. The periosteal reaction is based on vascularization in the fracture zone.The third and fourth phases of bone tissue regenerative processes are characterized by the formation of a bone callus. At the same time, if in the third phase there is a decrease in the processes of angiogenesis with the predominance of the process of formation of bone-cartilaginous callus, then in the fourth phase of bone tissue regeneration, bone tissue formation continues due to an increase in bone density.In the first subgroup of patients, the longest period was noted by us at the stage of bone marrow formation with a relatively pronounced confidence interval [CI: 91.7; 150.3].In the second and third subgroups of patients, the highest variability of the confidence interval was noted at the stage of formation of bone and cartilaginous calluses ([CI: 80.5; 131.3] and [CI: 131.4; 177.0], respectively).The shortest confidence interval in the last stage of tubular bone regeneration was noted by us among patients in whom the treatment process was completed without an overgrown bone fracture [CI: 194.3; 236.5]. In all other stages of bone regeneration, patients of the first subgroup accounted for.Thus, the analysis of visual control of bone regeneration after a fracture allows you to structure the stages of this process. The method is effective for controlling the dynamics of the process. However, the possibilities of this method for forecasting are limited, since the basis of the ongoing regeneration processes is determined by the timing. In other words, having statistical information about the timing of the changes that are taking place, we can only state the fact that has happened, but in no way predict.Based on the identified phases of bone marrow formation, we have formed the corresponding 4 factors of significance, which, in our opinion, when correlated with immunological monitoring data, will allow us to form a matrix for predicting the development of impaired bone regeneration. In this case, the axis of the matrix can be considered the average value of immunological monitoring of the general group of patients, which will also reveal the significance of certain markers depending on the actual outcome of bone regeneration. For this purpose, the division of patients into appropriate subgroups can be considered justified, since it reflects both the process and the outcome of the course of bone tissue regeneration.Before drawing parallels between factorial and correlation analysis of the distribution of variances in the indicators of immunological monitoring of bone regeneration, it is necessary to identify the "normal" level of the course of the postoperative period. As such a parameter, we selected data from patients of the first subgroup, whose bone tissue regeneration was complete without the development of any local purulent-inflammatory complications.In the first phase of bone tissue regeneration, out of the studied 20 indicators, an even half of them had high direct correlation values with respect to the dynamics of the entire group of patients. All of them were represented by indicators of cellular immunity, namely leukocyte response. Among them, the correlation values of leukocytes (R=0.998), neutrophils (R=0.971), the number of phagocytes (R=0.967), phagocytic activity (R=0.951), nuclear shift index (R=0.912), metabolic activity of phagocytes (R=0.903), leukocyte intoxication index (R=0.877), lymphocytes (R=0.778), monocytes (R=0.751) and leukocyte allergization index (R=0.738).The average level of direct correlation value was CD3+ (R=0.618), CD19- (R=0.588) and IL-1ß (R=0.422). The remaining 7 indicators of immunological monitoring were represented by a low direct correlation. Among them, cytokines IL-1α (R=0.395), IL-8 (R=0.255), TNF-α (R=0.117), IL-10 (R=0.019) and immunoglobulins Ig-A (R=0.015), Ig-M (R=0.012) and Ig-G (R=0.007).Thus, the first phase in patients with a normal outcome of bone tissue regeneration is characterized by a predominant proportion of indicators of the leukocyte blood reaction, activation of the phagocytic reaction and an adequate response to the inflammatory process. At the same time, half of the total values were determined by data from the first subgroup of patients.In the second phase of bone tissue regeneration, phagocytic activity (R=0.741), nuclear shift index (R=0.996), metabolic activity of phagocytes (R=0.982), leukocyte intoxication index (R=0.962), lymphocytes (R=0.959), monocytes (R=0.928), leukocyte allergization index (R=0.902), CD3+ (R=0.901), CD19- (R=0.873) and IL-1ß (R=0.759). The average level of correlation was noted in relation to the number of phagocytes (R=0.526), IL-1α (R=0.621), IL-8 (R=0.553) and TNF-α (R=0.497). Well, leukocytes (R=0.112), neutrophils (R=0.374), IL-10 (R=0.339) and immunoglobulins Ig-A (R=0.229), Ig-M (R=0.198) and Ig-G (R=0.118) distinguished themselves by a low correlation.Thus, in the second phase of bone tissue regeneration, T- and B-lymphocyte indices and the proinflammatory cytokine IL-1ß become active. At the same time, the primary cells of the leukocyte reaction of the blood acquired a low value.In the third phase of bone tissue regeneration, 45% of immunological monitoring indicators acquired low correlation significance, which was due to a decrease in activity in the formation of cartilaginous bone marrow. Among the indicators with a high correlation dependence, 7 indicators were identified, such as monocytes (R=0.703), leukocyte allergization index (R=0.851), CD3+ (R=0.986), CD19- (R=0.957), IL-1β (R=0.939), IL-1α (R=0.913), IL-8 (R=0.907). Four indicators had an average correlation of the overall indicators. Among them are the metabolic activity of phagocytes (R=0.454), leukocyte intoxication index (R=0.516), lymphocytes (R=0.694), TNF-α (R=0.432). Most of the indicators of immunological monitoring had a low correlation dependence, which indicated their loss from the active process of bone regeneration. These included such indicators as leukocytes (R=0.327), neutrophils (R=334), phagocyte count (R=0.357), phagocytic activity (R=0.386) and immunoglobulins A, M and G (R=0.361; R=0.357 and R=0.326, respectively).In the fourth phase of bone tissue regeneration, the proinflammatory cytokines IL-8 (R=0.712), TNF-α (R=0.863), anti-inflammatory cytokine IL-10 (R=0.868) and immunoglobulins A, M and G (R=0.872; R=0.881 and R=0.893, respectively, were distinguished by a high correlation dependence).Thus, immunological monitoring showed that in the initial phase of bone tissue regeneration, leukocyte cells are activated. Subsequently, subpopulations of cellular immunity and proinflammatory cytokines are involved in this process. In later periods, anti-inflammatory cytokines and immunoglobulins were more active in the process of bone tissue regeneration.Based on this scheme of immunological transformations in the process of normal bone regeneration, it seems to us, when compared with other subgroups of patients, to identify prognostic criteria for impaired bone marrow formation.Graphical analysis showed that under the conditions of the course of bone tissue regeneration, culminating in the formation of a callus without signs of the development of local purulent-inflammatory complications, all phases of the process have the corresponding four coverage zones (Figure 7). In the first phase of bone tissue regeneration, when the activity of the leukocyte reaction of the blood prevails, the process ends with the normal formation of a bone callus. A decrease in the activity of leukocyte activity of blood in the first phase of bone tissue regeneration was noted by us among patients of the second subgroup, in whom the course of the process of bone marrow formation occurred after the development of purulent-septic complication. In patients of this subgroup, activation of leukocyte subpopulations and the production of T and B lymphocytes initially occurred. Such a transformation of the regenerative process was associated with the addition of a local purulent-inflammatory complication and the process of callus formation left the zone of priority, as the fight against infection became a priority. As for the patients of the third subgroup, as can be seen from the nomogram, immunological reactions were the lowest, despite the development of local purulent-inflammatory complications.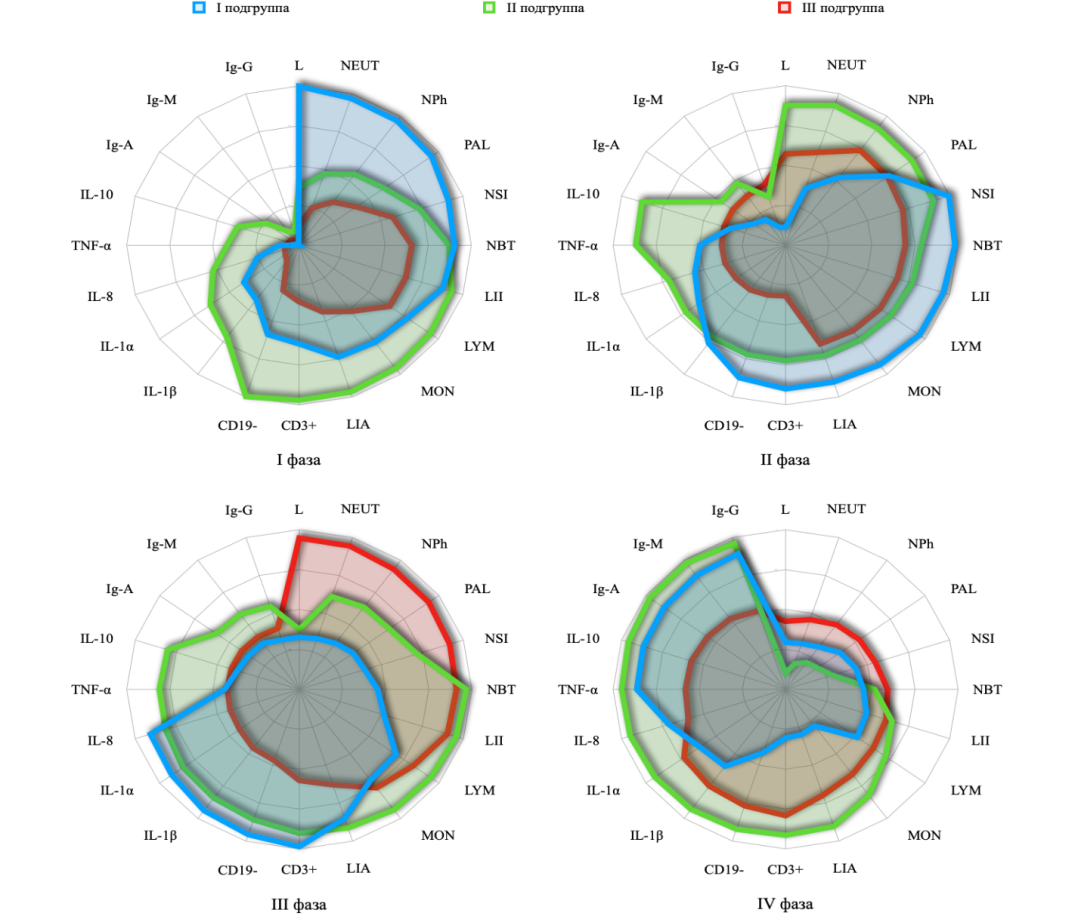 | Figure 7. The nature of the correlation significance of the indicators of immunological monitoring of bone regeneration in patients with closed fractures of long tubular bones in the context of subgroups after osteosynthesis |
In the second phase of bone regeneration in patients of the first subgroup, judging by the nomogram, the priority shifts clockwise towards the formation of an immunological response involving leukocyte subpopulations, with active expression of T-lymphocytes and B-lymphocytes, increased metabolic activity of macrophages and other leukocyte populations. In patients of the second subgroup, this process of immunological response also develops, however, not as pronounced as in patients of the first subgroup. Moreover, in patients of the second subgroup, the priority is still the development of leukocytosis, the formation of neutrophils and the beginning of the production of proinflammatory cytokines. Apparently, this reaction was dictated by the body's response to the inflammatory onset. In patients of the third subgroup, the nature of the immunological response of the body proceeds according to the scenario of patients of the second subgroup, however, as can be seen from the nomogram, its activity was 2 times lower, which apparently led to a more complex course of local purulent-inflammatory complications. This fact deserves special attention, since only during the third phase of bone tissue regeneration, in patients of the third subgroup, there is a surge in the leukocyte reaction of the blood, which prevailed in all the above-described subgroups of patients.In patients of the first subgroup, in the third phase of bone tissue regeneration, the full formed cellular and humoral immune response of the body becomes a priority. The expression of T-lymphocytes and B-lymphocytes occurred against the background of an active release of proinflammatory cytokines. In patients of the second subgroup, this reaction acquired a wider range of coverage of immunological control markers. However, in terms of its intensity, it was inferior to the transformations occurring in patients of the first subgroup. In other words, if we take the immunological response of the body in patients of the first subgroup into a local process of exposure, then in patients of the second subgroup the immunological response of the body acquired a larger scale.The onset of the fourth phase of bone tissue regeneration led to the expression of an immunological response of the body in patients of the second subgroup. Against this background, the local purulent-inflammatory complication was resolved and the process of bone tissue regeneration acquired a normal course. In contrast, in patients of the first subgroup, the main vector of the body's immunological response was directed at the priority production of immunoglobulins and anti-inflammatory cytokines (IL-10). In patients with impaired bone tissue regeneration, due to the formation of an inadequate immune response of the body, the formation of a callus leaves much to be desired. The low activity of involvement in the immune response of all key factors in the fight against infection and the inflammatory process resulted in a protracted process of bone marrow formation with complications in the long-term period after osteosynthesis.The graphical construction of the comparative curve of the phases of bone tissue regeneration after its fracture showed the priority of independence in the formation of an immunological reaction in patients of the first subgroup (Figure 8).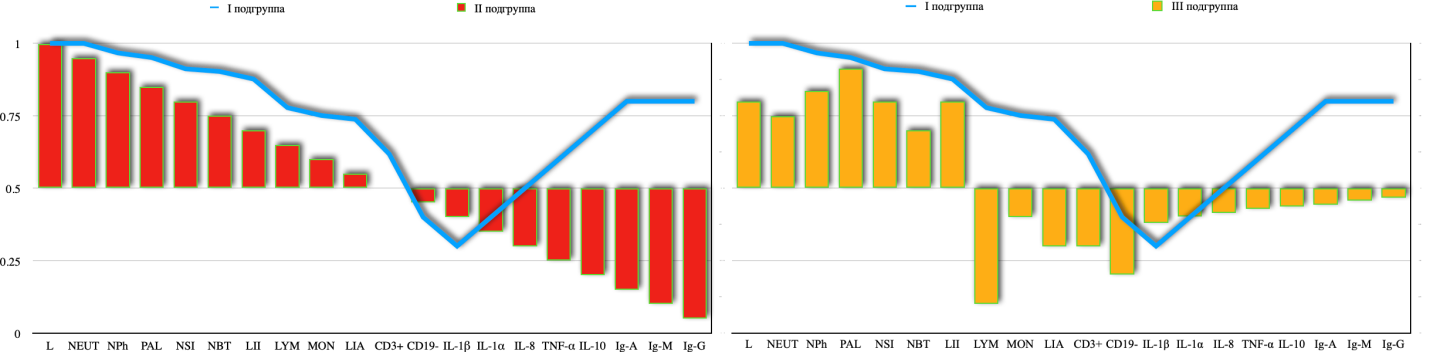 | Figure 8. Graphical dependence of immunological parameters in patients with closed fractures of long tubular bones in the context of subgroups after osteosynthesis |
This allows us to form a matrix of the biased dependence of the indicators of the immunological response of the body, which formed the basis of a software product called.Such a calculation formula was created by us as a software product called "IPBR" (Immunological Prediction of Bone Regeneration), and included criteria for an ultrasound picture of the bone regeneration phase, the presence or absence of a local purulent-inflammatory complication and the studied indicators of cellular and humoral immunity. They served as the basis for the construction of the computational program "IPBR" ("Method for predicting bone regeneration".At the same time, the prognostic probability of impaired bone regeneration was divided into low and high. In the absence of coincidence of the studied criteria with the developed software product, the probability of violation of bone regulation was excluded.The software product developed by us is available for wide implementation in practical healthcare, as it can function on any computer platform in various modes. This, in turn, minimizes the estimated time on the part of the medical staff.Thus, for predicting bone regeneration disorders in closed fractures of tubular bones, the optimal indicators are the integrated criteria of the ultrasound picture of the bone regeneration phase, the presence or absence of a local purulent-inflammatory complication and the studied indicators of cellular and humoral immunity. They served as the basis for the construction of the computational program "IPBR" ("Method for predicting bone regeneration"). At the same time, the prognostic probability of impaired bone regeneration can be divided into low and high. In the absence of a coincidence of the studied criteria with the developed software product, the probability of a violation of bone regulation is excluded. Next, a comparative assessment of the effectiveness of the developed clinical and immunological method for predicting bone regeneration disorders in closed fractures of tubular bones was performed. In the control group of patients, 62 (54.4%) patients had a postoperative period with various types of local complications. In most cases, these complications were combined and could occur in each patient in several of their varieties. In the main group of patients, there were 11.7% more such complications. In total, according to the medical history, 128 postoperative local complications were registered – on average, 2 complications per patient. This frequency of local postoperative complications was due to the frequency of hematomas and seromas.Of the main names of postoperative local complications, suppuration of the postoperative wound was registered in 54.4% of cases. Of these, in 28.1% of cases, we found the presence of contact postoperative osteomyelitis. 20 (17.5%) patients developed osteomyelitis spokes. All these complications were detected by us in the first month of the treatment.In the main group of patients, such complications were noted by us in the early postoperative period to a greater extent. So, if suppuration of the postoperative wound was recorded by us in 66.1% of cases, then contact osteomyelitis developed in 31.3% of patients, and spoke osteomyelitis – in 20.5% of patients. In all cases, the development of early postoperative complications in the main group of patients was significant, which dictated the need to improve methods for predicting the outcome of bone regeneration.The increase in the number of local postoperative complications from wounds and bones in the main group of patients was due to the decision-making on the need for repeated interventions in order to improve the results of bone regeneration.In the long-term period, unsatisfactory bone regeneration results were represented by non-accreted fractures (5.4%), improperly fused fractures (2.7%) and the formation of false joints (0.9%). In general, there were 12 patients in the control group and 10 patients in the main group with impaired bone regeneration in the long–term period.To comparatively evaluate the effectiveness of the developed method for predicting bone regeneration disorders, we compared traditional assessment methods (LII, LIA, NBT test and bone X-ray) and IPBR using evidence-based medicine criteria in 62 patients of the control and 74 patients of the main groups.The first comparison criterion was to identify the sensitivity of the test, indicating the possible development of a violation of bone regeneration.The sensitivity of traditional forecasting methods for admission to the clinic of patients with closed fractures of tubular bones fluctuated at an average level [CI: 41.2%; 54.6%]. At the same time, in comparison with these data, in patients of the main group, the sensitivity of the clinical and immunological test developed by us exceeded the traditional methods only by 1.2 times [CI: 48.8%; 63.0%] - Figure 5. On the 3rd day of the postoperative period, in patients of the control group, the sensitivity of the traditional prognostic test increased by 1.7 times than in the previous period [CI: 73.1%; 86.7%]. In patients of the main group, the sensitivity of the clinical and immunological test developed by us also increased (1.6 times; p<0.05) compared with the previous examination period. However, compared with traditional methods, it did not have a significant difference [CI: 77.1%; 99.9%].Meanwhile, studies on the 10th day of the postoperative period showed differences in the level of sensitivity due to a decrease in this value in the control group of patients by 1.5 times (p<0.05) compared with the previous study period [CI: 45.8%; 58.4%].In contrast to these data, in the main group of patients, we noted an increase in sensitivity based on clinical and immunological monitoring by 1.8 times (p<0.05) compared with traditional methods of predicting bone regeneration disorders [CI: 92.8%; 99.6%].In the period 30 days after osteosynthesis, the sensitivity of traditional tests decreased significantly (p<0.05). The significance of the changes was expressed in a decrease [CI: 26.9%; 32.7%] in the sensitivity of traditional forecasting methods by 1.6 times compared with the initial data (p<0.05), by 2.7 times compared with 3 days after surgery (p<0.05) and by 1.7 times compared with the previous study period (p<0.05). Nevertheless, in the main group of patients, the sensitivity of the clinical and immunological tests developed by us exceeded the traditional methods by 2.6 times (p<0.05), although it was reduced by 1.2 times compared to the previous period [CI: 76.1%; 79.7%].In the early long-term period, 3 months after osteosynthesis, the sensitivity of traditional methods for predicting impaired bone regeneration decreased to a minimum value [CI: 20.4%; 24.6%] of the entire monitoring period by 2.1 times compared with the preoperative period (p<0.05), by 3.5 times compared with 3 days (p<0.05), 2.3 times compared to 10 days (p<0.05) and 1.3 times compared to 30 days of the postoperative period (p<0.05).In the main group of patients, the sensitivity of the clinical and immunological test developed by us also decreased (by 1.1 times) compared to the previous study period, however, it exceeded the traditional methods of predicting bone regeneration disorders by 3.1 times (p<0.05). The reliability of the values of clinical and immunological tests in the main group of patients at this time was confirmed by the data of the confidence interval [CI: 67.7%; 69.9%].Thus, a comparative analysis of the average statistical sensitivity values of methods for predicting impaired bone regeneration in fractured tubular bones revealed a 2-fold increase in this indicator among patients of the main group. Traditional methods of predicting bone tissue regeneration disorders had an average test sensitivity of 46.4±5.1% [CI: 41.4%; 51.5%], whereas in the main group it was 77.5±5.3% (p<0.05) [CI: 72.2%; 82.7%].The next comparative assessment was the specificity of prognostic tests, where bone radiography data played an important role in patients of the control group. At the same time, both clinical and immunological tests turned out to be specific in patients of the main group.In patients of the control group, the initial level of test specificity was not high [CI: 33.9%; 42.3%], however, as in patients of the main group [CI: 36.9%; 42.7%]. The difference between them was not significant (p>0.05). However, already on the 3rd day after osteosynthesis, the comparative dynamics of changes in the specificity of prognostic tests changed in the opposite vector. In patients of the control group, the specificity of prognostic tests decreased by 1.1 times compared to the previous study period [CI: 29.0%; 36.8%], whereas in patients of the main group it increased by 1.5 times [CI: 57.3%; 64,9%]. Such changes were significant both in relation to the previous study period (p<0.05) and in relation to traditional methods of predicting bone regeneration in this studied period (p<0.05) with an increase of 1.9 times.Changes in the specificity of prognostic tests of bone regeneration in patients of the control group on the 10th day after osteosynthesis were not significant compared to previous study periods [CI: 31.3%; 36.9%]. In patients of the main group, the use of the developed test revealed an increase in the specificity of prognostic clinical and immunological tests by 1.7 times compared with the initial data (p<0.05) and 2 times more than traditional methods (p<0.05).1 month after osteosynthesis, the specificity level of traditional tests for predicting impaired bone regeneration decreased by 1.3 times compared with the initial values [CI: 26.4%; 31.4%], and in the main group of patients it increased by 1.7 times [CI: 63.8%; 75.6%]. The difference between traditional and original forecasting methods in this period was 2.4 times (p<0.05).In subsequent periods of the study, this trend continued. In the control group of patients, the decrease was already 1.7 times [CI: 19.8%; 24.6%], and in the main group of patients – an increase of 1.9 times [CI: 69.8%; 80.8%] compared with the baseline data (p<0.05).
5. Conclusions
To predict bone regeneration disorders in closed fractures of tubular bones, the optimal indicators are the integrated criteria of the ultrasound picture of the bone regeneration phase, the presence or absence of a local purulent-inflammatory complication and the studied indicators of cellular and humoral immunity. They served as the basis for the construction of the computational program "IPBR" ("Method for predicting bone regeneration"). At the same time, the prognostic probability of impaired bone regeneration can be divided into low and high. In the absence of a coincidence of the studied criteria with the developed software product, the probability of a violation of bone regulation is excluded. A comparative assessment of the effectiveness of the developed clinical and immunological method for predicting bone regeneration disorders in patients with closed fractures of tubular bones showed the possibility of increasing, compared with traditional methods, its average sensitivity level from 46.4±5.1% to 77.5±5.2%, and the average level of specificity from 31.2±3.2% to 62.9±4.5%, which was achieved by optimizing immunological monitoring of osteosynthesis.Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest: The authors have no conflicts of interest.
References
| [1] | Belokhvostikova T.S. Cytokine regulation of osteogenesis // Byul. VSNTS SB RAMS. Irkutsk: "NTO NCRVH VSNC SB RAMS", 1999; 1(9): Pp.147-152. |
| [2] | New perspectives on bone tissue regeneration in atrophy and defects of jaw bone tissue / A. Yu. Ryabov, M. V. Lekishvili // Topical issues of tissue and cell transplantology: Collection of abstracts on VII All-Russian Symposium with International participation, Astrakhan, April 27-28, 2017. – Astrakhan: Astrakhan State Medical University, 2017. – pp. 10-11. |
| [3] | Experimental substantiation of the use of combined biomaterials for bone tissue regeneration / S. M. Hefzollesan, F. Y. Mammadov, G. G. Musayeva, A.M. Mammadov // Bulletin of dentistry. - 2022. – Volume 120, No. 3. – pp. 76-82. |
| [4] | Bal Z., Kushioka J., Kodama J., Kaito T., Yoshikawa H., Korkusuz P., Korkusuz F. The use and release of BMP and TGFß in bone regeneration. Turk J Med Sci. 2020, November 3; 50(SI-2): 1707-1722. |
| [5] | Human lactoferrin interacts with soluble CD14 and inhibits the expression of endothelial adhesion molecules, E-selectin and ICAM-1 induced by the CD14 - lipopolysaccharide complex / S. Bavey, E. Elass, D.G. Fernig, S. Blankwart et al. // J. Infect Immun. – 2020;68:Pp.6519-6S2S. |
| [6] | Immunological defects after injury: delayed synthesis of immunoglobulin by cultured B cells after traumatic events, but not elective surgery / M. Richter, K.A. Joduen, D. Moher, PhD. Barron // J. Trauma. – 2020; 30(5): pp.590-596. |
| [7] | Palanisami P., Alam M., Li S., Chou S.S., Zheng Y.P. Low-intensity pulsed ultrasound stimulation for bone fracture healing: a review. J Ultrasound Med., March 2022; 41(3): 547-563. |
| [8] | Schoenvelder S.M., Burridge K. Bidirectional signaling between the cytoskeleton and integrins // J. Curr. Opinion. Cell biology. – 2019; 11: pp.274-286. |
| [9] | Sequential expression of bone morphogenetic protein, tumor necrosis factor and their receptors in the bone formation reaction after removal of bone marrow from the mouse femur / T. Shimizu, R. Mehdi, Y. Yoshimura, H. Yoshikawa et al. // Bone, 2018; 23:127-133. |
| [10] | Song S Yun Sh Kim M.H. Yun X Activin A and chimera BMP (AB204) induced bone fusion in the spine with osteoporosis in a rat model with an ovary removed. Spine Magazine. 2020; 20: 809-820. |
| [11] | Wozniak J.M., Rosen V. Bone morphogenetic protein and the family of bone morphogenetic protein genes in bone formation and repair // Klin. Orthopedist, 2018; 346:26-37. |
| [12] | Tegaev O.R., Morozov A.Sh., Sadykov R.R., Khamdamov B.Z. Improvement of the results of treatment of purulent wounds with the combined use of photodynamic therapy and CO2 laser in an experiment. The European Scientific Review. Austria, Vienna, March-April 2016, No. 3-4. – pp. 185-189. |
| [13] | Leonova S.N. A method for predicting bone tissue regeneration // Byul. VSNTS SB RAMS. 2002. - Vol. 2, No. 6. - pp. 47-49. |
| [14] | Khamdamov B.Z. Comparative assessment of amputation methods in hip joint and severe forms of diadetic foot syndrome. The European Scientific Review. Austria, Vienna 2014 September-October No. 9-10. - pp. 58-60. |
| [15] | Khamdamov B.Z. Diabetic tovon sindromida bazhariladigan yukori amputationalardan sung bemorlarning hayet kechirish sifatidagi uzgarishlar takhlili. Samarkand. Biology of tibbiet muammolari. №1, 2019., (107) - Pp. 115-117. |
| [16] | Khamdamov B.Z. Complex treatment of diabetic foot syndrome with critical ischemia of the lower extremities. Journal of Biomedicine and Practice. Tashkent 2020, Special issue. Part 5. – pp. 801-814. |
| [17] | Khamdamov B.Z. Method of laser photodynamic therapy in the treatment of wound infection in diabetic foot syndrome. Biology of tibbiet muammolari No.1 (116) 2020. – pp. 142-148. |
| [18] | Khamdamov B.Z. Morphological changes in the application of photodynamic therapy in the treatment of wound infection in an experiment. Journal of Morphology. St. Petersburg. 2020. Volume 157 (2-3). –pp. 223-224. |
| [19] | Khamdamov B.Z. Optimization of methods of local treatment of purulent-necrotic foot lesions in diabetes mellitus. Journal. Tibbietda yangi kun. 2018, No.4 (24) - pp. 112-115. |
| [20] | Aarden E.M., Burger E., Naivaide P.Ya. Function of osteocytes in bone // J. Cell. Biochemistry. 1994. - Volume 55, number 3. - pp. 287-299. |
| [21] | Baron R. Molecular mechanisms of bone resorption // Acta Orthop. Scand. 1995. - Volume 66. - Appendix 266. - pp. 66-76. |
| [22] | Khamdamov B. Z., Akhmedov R. M., Khamdamov A. B. The use of laser photodynamic therapy in the prevention of purulent-necrotic complications after high amputations of the lower extremities at the shin level in patients with diabetes mellitus. Review in Scopus. International Journal of Pharmaceutical Research. Volume 11, Issue 3, July-September 2019. |
| [23] | Khamdamov B.Z., Nuraliev N.A. Pathogenetic approach in the complex treatment of diabetic foot syndrome with critical lower limb ischemia. American Journal of Medicine and Medical Sciences, 2020 10 (1) 17-24 DOI:10.5923/j.20201001.05. |
| [24] | Khamdamov B.Z. Indicators of immunocytocin status in purulent-necrotic lesions of the lower extremities in patients with diabetes mellitus. American Journal of Medicine and Medical Sciences, 2020 10 (7): 473-478 DOI:10.5923/j.20201001.08. |
| [25] | Khamdamov B., Dekhkonov A. (2022). Clinical and laboratory indicators of the wound process complicated by systemic inflammatory reaction syndrome in patients with diabetes mellitus. Journal of Education and Scientific Medicine, 2(3), 25-29. Extracted from https://journals.tma.uz/index.php/jesm/article/view/349. |
| [26] | Khamroev U., Khamdamov B. (2022). Features of changes in the parameters of the endothelial system in patients with diffuse toxic goiter. Journal of Educational and Scientific Medicine, 2(3), 62-67. Extracted from https://journals.tma.uz/index.php/jesm/article/view/358. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML