-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(6): 1581-1583
doi:10.5923/j.ajmms.20241406.24
Received: May 28, 2024; Accepted: Jun. 16, 2024; Published: Jun. 19, 2024

Changes in Cerebral Hemodynamics in Children with Type 1 Diabetes with Cognitive Impairments
Hasanova N. O., Majidova Y. N.
Tashkent Pediatric Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article presents changes in cerebral hemodynamics in children with type 1 diabetes mellitus, with a history of the disease of 3 years or more. The earliest diagnosis and adequate correction will prevent the worsening of cerebral disorders in this category of patients with diabetes.
Keywords: Diabetes mellitus, Hemodynamics, Cognitive impairment, Children
Cite this paper: Hasanova N. O., Majidova Y. N., Changes in Cerebral Hemodynamics in Children with Type 1 Diabetes with Cognitive Impairments, American Journal of Medicine and Medical Sciences, Vol. 14 No. 6, 2024, pp. 1581-1583. doi: 10.5923/j.ajmms.20241406.24.
Article Outline
1. Introduction
- Diabetes mellitus (DM) is considered to be an endocrine autoimmune pathology that develops as a result of an absolute or relative deficiency of insulin caused by the destruction of beta cells of the pancreas. At the present stage, diabetes is a serious medical and social problem, as it remains one of the leading causes of decreased quality of life and the occurrence of early disability due to the formation of long-term complications [5].Chronic high glycemia inherent in diabetes mellitus causes functional and structural disorders of organs and systems of the body, most often the organs of vision, cardiovascular system, kidneys and especially the nervous system are affected. This fact of the negative and sustainable impact of increased glycemia on the formation, frequency and severity of possible complications in diabetes was discovered and proven by scientists back in the middle of the last century [1,3,4].Currently, there is no doubt about the role of type 1 diabetes mellitus (DM) in the occurrence of vascular pathology of the brain with an increase in the likelihood of developing acute and chronic cerebrovascular accidents by 2-6 times. The main mechanisms for the development of cerebral vascular pathology in diabetes in childhood are cerebral chronic metabolic disorders and microcirculation disorders caused by changes in the structure of the walls of blood vessels, the biochemical composition of the blood and fluctuations in blood pressure [2].
2. Purpose of the Study
- The earliest diagnosis and adequate correction can prevent the worsening of cerebral disorders in this category of patients with diabetes.
3. Materials and Methods of Research
- We examined 102 patients with type 1 diabetes mellitus, with a history of the disease of 3 years or more. The studies were conducted in the children's department of the Republican Scientific and Practical Medical Center in 2022-2024 in children aged 7-18 years. A clinical and neurological examination of the children was carried out and anamnestic information about the severity of diabetes and the number of comatose states suffered was clarified.The study of cerebral hemodynamics was carried out according to standard methods using an ultrasonic Doppler device “Multi-Dop” T2 DWL – 2.55 MDT from Elektronische Systeme GmbH with a set of sensors generating ultrasonic waves with a frequency of 2; 4 and 8 Hz.Using transcranial Dopplerography (TCDG), indicators of cerebral blood flow were studied in the arteries of the base of the brain: paired 62 midcerebral (MCA), forebrain (AF) and basilar artery (BA), as well as in deep intracranial venous collectors (basal veins and straight sinus); at the extracranial level, indicators of cerebral hemodynamics were determined in the vertebral arteries (VA), as well as in the superior orbital veins, vertebral and internal jugular veins. In the studied arterial vessels, the components of linear blood flow velocity (LBV) were recorded: peak systolic (Vs), end-diastolic (Vd) and average (Vm); The index of peripheral vascular resistance (IR) was calculated using the generally accepted formula: IR = (Vs-Vd)/Vs. In the venous collectors, the intensity of venous outflow was assessed by the value of the maximum BSC in them (Vmax), and the direction of blood flow, in particular, along the orbital veins, was also taken into account.
4. Results and Discussions
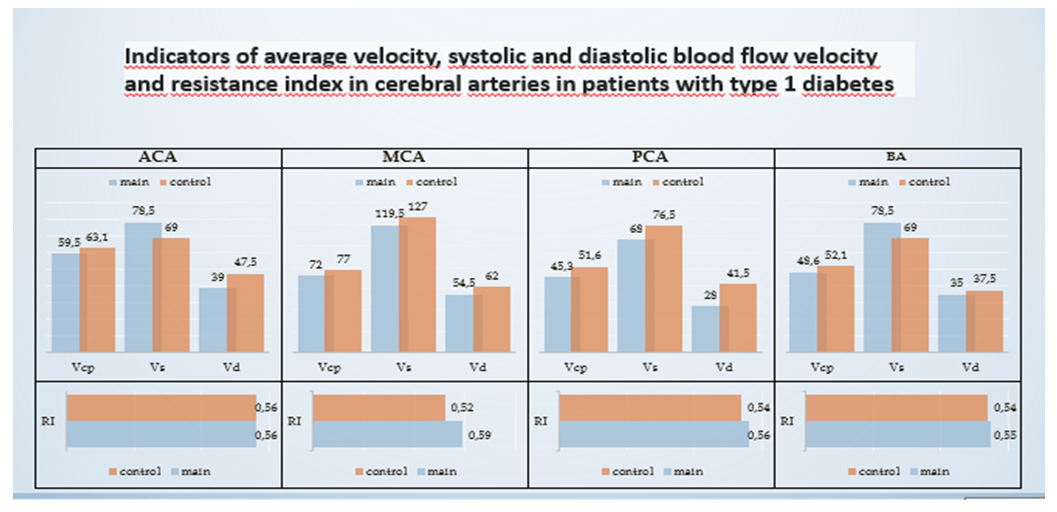
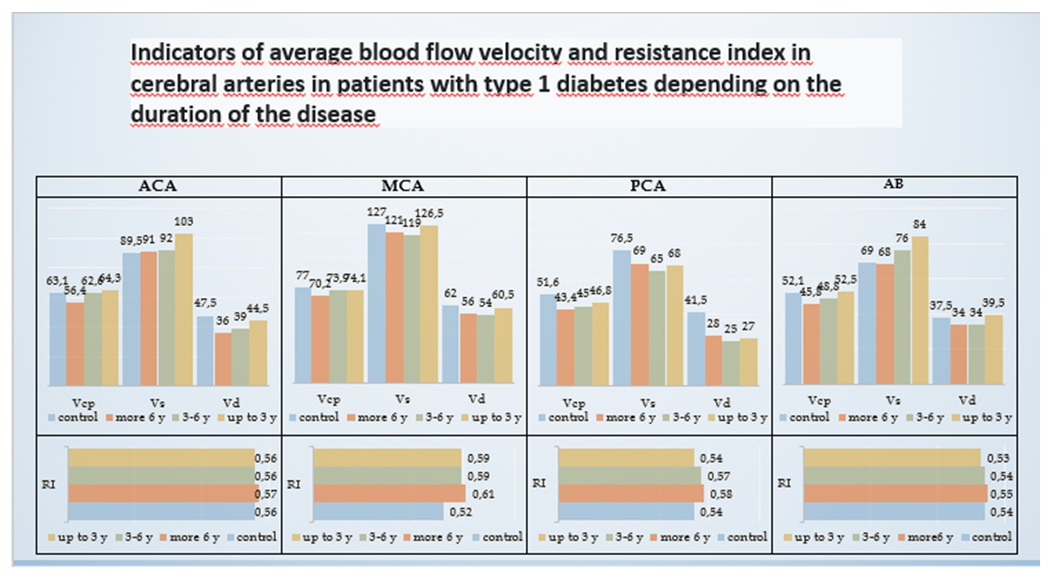
- To identify changes in cerebral hemodynamics, we created 3 groups of children depending on the length of the disease. Group I with a disease experience of up to 3 years, Group II from 3 to 6 years and Group III more than 6 years. 25 healthy children were also studied to compare the data. The results of changes in cerebral hemodynamics are presented in Fig. 1.
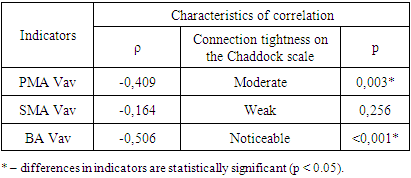
 | Figure 1. * – differences in indicators are statistically significant (p <0.05) |
 | Figure 2. * – differences in indicators are statistically significant (p < 0.05) |
|
5. Conclusions
- Thus, in patients with diabetes in childhood and adolescence, Dopplerographic signs of deterioration in cerebral blood flow, characterized mainly by a hypertensive-hypokinetic type of arterial blood flow and varying degrees of venous discirculation, are significantly more likely than in persons without carbohydrate metabolism disorders. The frequency and severity of these disorders increases with increasing experience of diabetes mellitus.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML