-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(6): 1563-1567
doi:10.5923/j.ajmms.20241406.20
Received: May 25, 2024; Accepted: Jun. 12, 2024; Published: Jun. 14, 2024

Dynamics of Changes in the Parameters of Thyroid Gland Hormones and Platelet Aggregation in Heat Developing Hyperthyrois
Khanov Alaviddin Shakhojayevich, Akhmedov Kamoliddin Khakimovich, Khujanazarova Shakhlo Khakimovna, Musurmonova Asal Isroilovna
Termez Branch of Tashkent Medical Academy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Various disorders of blood clotting and fibrinolysis observed in patients with hyperthyroidism can cause subclinical clinically significant disorders of blood clotting, bleeding and thromboembolism. Some authors indicate that a decrease in thyroid-stimulating hormone levels is an independent risk factor for an increase in plasma fibrinogen levels. Hyperthyroidism is usually associated with increased blood clotting and decreased fibrinolytic activity, but patients may also have hyperfibrinolytic reactions that negatively affect cardiovascular diseases in general. This section discusses functional changes in the thyroid gland, as well as the hemostatic system in experimental hyperthyroidism that developed in a hot climate.
Keywords: Hyperthyreosis, Aggregation, Platelet
Cite this paper: Khanov Alaviddin Shakhojayevich, Akhmedov Kamoliddin Khakimovich, Khujanazarova Shakhlo Khakimovna, Musurmonova Asal Isroilovna, Dynamics of Changes in the Parameters of Thyroid Gland Hormones and Platelet Aggregation in Heat Developing Hyperthyrois, American Journal of Medicine and Medical Sciences, Vol. 14 No. 6, 2024, pp. 1563-1567. doi: 10.5923/j.ajmms.20241406.20.
Article Outline
1. Introduction
- Currently, the world is increasingly experiencing diseases of the leading endocrine system in the adult population, such as diabetes, thyroid disease and obesity, nutritional and metabolic disorders. Endocrine glands occupy one of the central places in the specialized management of various vital processes at the level of the whole organism.There are various opposite types of opinion about the effect of hypothyroidism on hemostasis, so earlier studies have shown that thyroid hypofunction may be associated with hypo - or hypercoagulation conditions, but the relationship between QB disease and hematological anomalies and there were opposite side [1,2,8]. Platelets are not only important in the plasma reactions of the main vascular platelets hemostasis, inflammation, angiogenesis, but also participate in the formation of the immune system [3,9,13]. Platelet activation plays an important role in protective hemostasis and pathological thrombosis [7]. Currently, the generally accepted method in laboratory practice to assess the aggregation activity of platelet communication of hemostasis is aggregatometry [6,11].
2. Development Level
- Disorders of hemostasis in hypothyroidism are associated with a deficiency of thyroid hormones, but the mechanisms have not yet been determined [5,10]. An increase in platelet counts as inflammatory cells important for perioperative organ damage requires significant reassessment [4]. Thus, hypothyroidism and other non-toxic diseases, in patients with platelet reactions, have not been sufficiently studied, and their research is an urgent scientific and clinical problem [12]. In patients with impaired thyroid function, the functional activity of platelets is not well studied, and its study is an urgent issue. Platelets have been found to play an important role not only in hemostasis, but also in inflammatory reactions, immune defense reactions, angiogenesis. This is confirmed by numerous data confirming the idea of platelet activation in various pathological conditions, including pathological thrombosis. Platelets are involved not only in the formation of the main vascular platelets, but also in the formation of the immune system. Platelet activation plays an important role in defensive hemostasis and pathological thrombosis. Disorders of hemostasis in hypothyroidism are associated with a deficiency of thyroid hormones. An increase in the number of platelets as inflammatory cells, which are important for perioperative organ damage, requires a significant reassessment. Thyroid hormones are a powerful mediator of many physiological processes, and the fact that their amount is not in the norm can negatively affect their various stages in the coagulation cascade. Early data on the relationship between thyroid diseases and coagulation abnormalities date back to the early years of the last century. Thyroid dysfunction has been associated with conflicting scientific studies on coagulation abnormalities from subclinical laboratory disorders to clinical bleeding and thromboembolism. In obstetrics, blood clotting disorders of a thrombogemorrhagic nature develop with many complications of the pregnancy process, which are based on the processes of pathological activation of intravascular blood clotting, typical manifestations of decompensation of blood hemostasiological functions, which can be carried out during childbirth. The thrombotic manifestation of disorders of hemostatic functions, as a rule, has small pre-clinical signs, and the nature of hemorrhagic disorders is not always homogeneous due to the features of adaptive changes in the hemostasis system, which develop against the background of the development of pregnancy and affect them pregnancy complications [16,17].Pregnancy is seen as a hypercoagulation condition due to increased concentration of circulating procoagulation factors, decreased concentration of protein anticoagulants, and fibrinolysis [18].Hormonal and metabolic disorders that develop in pregnant women with autoimmune hyperthyroidism (AIG) directly affect the condition of various organs and systems, including the state of the hemostasis system [19].Most often, hypergomocysteinemia (GGT) is observed against the background of AIG in pregnant women. A number of studies studying the biochemical mechanisms of homocysteine toxicity have shown that the harmful effects of homocysteine on the components of the coagulation cascade increase in proportion to the concentration and duration of this effect [14,20].The negative effects of GGT on vascular endothelium and thrombosis lead to the development of a number of pregnancy complications: can lead to a violation of the placenta in the early stages of pregnancy, lead to impaired fetal circulation and loss of pregnancy; can later be the cause of chronic placental insufficiency, which leads to chronic hypoxia and malnutrition of the fetus.The development of pathogenetically based methods of prevention and treatment of pregnant women with AIG in ggtfoni reduces obstetrics and AIG.In humans, hyperthyroidism alters the coagulation-fibrinolytic balance, creating a hypercoagulation condition that increases the risk of thromboembolism. With a high concentration of free thyroxine in humans, the risk of venous thrombosis increases. The mechanisms by which hyperthyroidism causes hypercoagulation in humans include all stages of hemostasis. Primary hemostasis is exacerbated by an increase in the concentration of the circular von Willebrand factor (WF), which allows platelets to adhere to the subendothelium. Hyperthyroidism also enhances secondary hemostatic function with an increase in coagulation proteins such as factor VIII, factor IX and fibrinogen, and in addition, fibrinolysis is impaired as a result of an increase in the concentration of plasminogen activator inhibitors and, finally, hyperthyroidism leads to endothelial dysfunction, which contributes to hypercoagulation in humans.Research material and methods: experiments, the hyperthyroidism model arose by administering L – thyroxine at an ambient temperature of 35-38°C every day for 30 days at a dose of 100 mcg /kg in 96 white– breed male rats in a mixed population with an initial weight of 130-180 gr, kept on a laboratory diet in vivarium. As a control group, 12 intact rats were obtained. Samples for analysis were examined on the 1st and 7th day after the hyperthyroidism model was called in experimental groups. The content of TTG, T4, T3 in the blood was determined by the enzyme-related method of IXLA. The number of red blood cells was determined by the camera method with Goryaev networks.
3. Research Results and Their Discussion
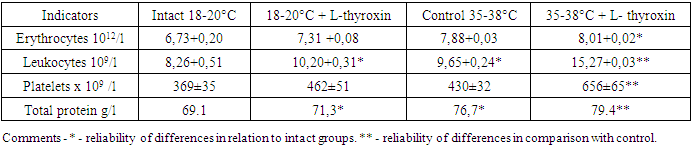
- A study of the composition of blood cells of experimental animals showed that the number of erythrocytes in Intact Group animals is 6.73 + 0.20 x 1012 / l, leukocytes are 8.26 + 0.51 x 109/L, platelets are 369±35 x 109 / L. In the case of animal preservation under conditions of high ambient temperatures, the same parameters were 17.1% higher, 16.8% and 16.5% (table), respectively. These results indicate a significant thickening of the blood under the influence of high ambient temperatures.
|
|
4. Conclusions
- The development of experimental hyperthyroidism at normal ambient temperatures is characterized by an increase in the number of single elements of the blood.The development of experimental hyperthyroidism at high ambient temperatures is characterized by an increase in the parameters of single elements of the blood. The detected changes in the procoagulatory properties of the blood, characteristic of hyperthyroidism under conditions of high ambient temperature, determine the high relevance of antithrombic measures. High ambient temperatures help to increase the amount of TTG and thyroid hormones in the blood more precisely in experimental hyperthyroidism.Increased levels of hormones in the blood in turn reveal the main mechanisms of the dynamics of the influence of blood on changes in the procoagulatory property in hyperthyroidism, which develop under thermal conditions.The results of our studies were characterized by the fact that in experimental hyperthyroidism at high ambient temperatures, an increase in the amount of hormones in the blood provides hypercoagulation, and, as a result of high temperatures, the development of experimental hyperthyroidism is accompanied by an increase in platelet self-i.e. spontaneous aggregation parameters (Day 1 and 7). Thus, the results of the study show the peculiarities of changes in the content of TTG and thyroid hormones in animals with experimental hyperthyroidism, the composition of elements in the blood and the uniformity of hemostasiological reactions, depending on the temperature of the environment. Under conditions of high environmental temperatures, the development of experimental hyperthyroidism contributes more precisely to the interpretation of a significant increase in the procoagulatory activity of TTG, T4, T3 and platelets in the blood.
5. Recommended
- 1. The thyroid gland plays an important role in regulating the functional state of organs and systems. Therefore, an increase in the amount of thyroid hormones can cause pathologies of cardiovascular, neuropsychiatric, Gastroenterological, hematological diseases, diseases of the reproductive system and some immunopathological processes. For this reason, patients with hyperthyroidism are not recommended to control hormone levels and be exposed to high environmental temperatures. 2. Patients with hyperthyroidism are not recommended to be in the sun and at high temperatures for a long time, are characterized by a further increase in the procoagulatory activity of platelets under conditions of high ambient temperatures, and an increase in platelet aggregation is observed under the influence of high temperatures.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML