-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1413-1417
doi:10.5923/j.ajmms.20241405.58
Received: Apr. 1, 2024; Accepted: May 2, 2024; Published: May 23, 2024

Clinical-Neurological, Instrumental, and Neuropsychological Aspects of Changes in Children with Bronchial Asthma
Samatov Farrukh Farkhodovich1, Jurabekova Aziza Tokhiovna2, Himmatov Shuhrat Abdurasul Ugli3
1Independent Researcher, Department of Neurology of Samarkand State Medical University, Assistant, Department of Medical Psychology, Neurology and Psychiatry, Termiz branch of the Tashkent Medical Academy, Uzbekistan
2Doctor of Medical Sciences, Professor, Department of Neurological Diseases, Samarkand State Medical University, Uzbekistan
3Family Polyclinic No. 4, General Practitioner, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This paper explores the clinical-neurological, instrumental, and neuropsychological dimensions of bronchial asthma in children. Asthma, a chronic respiratory condition, not only affects pulmonary function but also has profound impacts on neurological and neuropsychological aspects. Clinical manifestations include exacerbations, cognitive deficits, and emotional disturbances. Instrumental assessments such as neuroimaging and pulmonary function tests reveal structural and functional abnormalities in the brain and respiratory system. Neuropsychological evaluations highlight deficits in attention, memory, and executive functions. Understanding these multifaceted aspects is crucial for comprehensive management and improved outcomes in children with asthma.
Keywords: Bronchial asthma, Children, Clinical-neurological, Instrumental assessments, Neurological impacts, Neuropsychological impacts, Respiratory function, Cognitive deficits, Emotional disturbances
Cite this paper: Samatov Farrukh Farkhodovich, Jurabekova Aziza Tokhiovna, Himmatov Shuhrat Abdurasul Ugli, Clinical-Neurological, Instrumental, and Neuropsychological Aspects of Changes in Children with Bronchial Asthma, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1413-1417. doi: 10.5923/j.ajmms.20241405.58.
1. Introduction
- Bronchial asthma in children (BA) in modern times is one of the most pressing problems in children's health. Research over the past ten years has shown an increase in morbidity and mortality from asthma. According to the Global Asthma Report 2022, compiled by 97 experts from 31 countries, 262 million people worldwide suffered from the disease in 2019 [1,5,9]. In 2022, according to various sources, there are about 300 thousand patients in the world. 14% of them are children. If we consider the indicators of different countries on the prevalence of asthma in children, then today in Russia the incidence is 6-8%, while the frequency of high numbers can be traced among children of early school age. in the USA - among children, asthma disease 6.2 million (8.4%) are children, while 4.4% are patients aged 0 to 4 years; 8.8% – children from 5 to 14 years old; 11.1% – from 15 to 17 years old. WHO statistics show an increase in the disease in countries by 8-10 times over the past 10 years, especially among children living in the Megapole, which causes a huge resonance among medical organizations working in this direction. The widespread implementation of the National Program made it possible to form a unified position in the fight against asthma in children and achieve significant success in the diagnosis and treatment of this disease, reducing mortality and disability of patients [2,6,10]. However, some issues remain debatable, in particular, violations of social adaptation, psychotraumatization, and behavioral disorders, cognitive disorders - this is a far from complete list of problems associated with changes in the central nervous system (CNS), reducing the quality of life of children and increasing the comorbid background of disease progression. Cognitive disorders, as a complication of comorbid somatoneurological diseases, are now increasingly observed in patients with chronic diseases (Compas et al., 2017; Berger et al., 2016); However, asthma, a fairly common chronic disease that primarily affects the respiratory tract, remains poorly studied (Ranzini et al., 2020). Dunleavy and Baade were the first to write about the connection between behavioral disorders and AD in 1980; their research proved a comparative difference in children’s schooling and a decrease in cognitive abilities in children with AD compared with healthy peers (Dunleavy and Baade, 1980) [3,7,11]. Scientific literature, including experimental work, studying the problem of asthma and mental performance, speaks of a large-scale contribution of neurons in asthma, where the process is focused mainly on the hippocampus (a neural region involved in memory and signal synthesis (Fan et al., 2017). Thus, according to a randomized study, European scientists found (n=1287) in 10.8% of patients diagnosed with AD to have a decrease in hippocampal volume compared to a control group of the same age without asthma (Carlson et al., 2017). changes in the structure of the central nervous system, according to neuroimaging data in patients with AD, reveals significant damage to the integrity of the white matter and changes in metabolism in the overall structure (Juliet L. Kroll 2023) [3,4,8]. Neurological communication pathways are known to activate the sympathetic-parasympathetic. nervous system, thanks to inflammatory and immune processes, thereby causing a parallel proliferation (activation) of microglia and astrocytes, with a damaging effect on neurons, therefore, the reverse regulation of the neuroendocrine basis is triggered, which, in a vicious circle, affects the lungs, and increasing the symptoms of AD (Yao Wang etall 2023). Thus, it seems relevant to comprehensively study the characteristics of the central nervous system in children with various forms of asthma, which will not only overcome the neurological disorders characteristic of this disease but also prevent the formation of typical cognitive disorders that reduce the quality of life of children with asthma.Purpose of the study: To study the clinical, neurological, neurophysiological, and neuropsychological characteristics of children with different courses of bronchial asthma.
2. Material and Methods of Research
- The work was carried out from 2022-2024 in the regional hospital of the Surkhandarya region, in the children's department, departments of the Children's Multidisciplinary Hospital department, and the Children's department of the Multidisciplinary Clinic of SamSMU in Samarkand. The source material was children undergoing inpatient and outpatient treatment with a diagnosis of bronchial asthma (BA), in the amount of 59 patients, who made up the main group, who underwent pediatric, neurological, and neuropsychological examinations; The comparison group included children identical in age and gender, healthy and without asthma. The age of the children examined varied from 7 to 14 years, there were fewer boys compared to girls, so boys made up 41%, and girls, respectively, 59%. In the first stage, a survey was conducted with parents and teachers of patients taken for examination, in addition, a survey and conversation with peers (classmates) were conducted on the aspect of the behavior and emotional character of the patients; The questionnaires were compiled randomly and approved by the departmental and thematic council at the department of neurology. The evaluation criteria for the subsequent examination were a clinical neurological examination, and a neurophysiological examination using an electroencephalography apparatus. The most difficult thing turned out to be the neuroimaging of the brain, since according to the protocol standards this procedure is contraindicated in patients with asthma (especially young children), in addition, testing the feeling of fear in children before the examination can lead to the onset of an attack of shortness of breath, but on the other hand it was necessary to obtain a picture of the structure of the brain, and therefore, with the permission of pediatricians, children over 15 years of age, and the severity of mild and moderate severity served as a criterion for neuroimaging of the brain. Patients underwent neuropsychological testing using the Wechsler scales and the Luscher test. Statistical indicators were assessed on an individual computer, with a standard package of deviation criteria used and Spearman, Mann-Whitney correlation, where p-0.05.
3. Result
- Under the purpose of the study, it was necessary to determine the level of general analysis of optimization of children among their peers (healthy without AD), the characteristics of the psychological state in the opinion of parents, teachers at school, for this purpose how a survey was organized from the patients’ environment as adults and peers. When surveyed by teachers at school, it turned out that children with asthma have some deviations, in the form of immaturity in communication, and lack of confidence in their actions (decision-making). Thus, according to statistical indicators, in comparison with a healthy group of children, P < 0.05. In addition, the survey revealed problems with learning, in the form of a slower reaction to a question asked, solving problems assigned to the patient, “going out” to the board is accompanied by fear of the audience, many began to choke, pallor of the skin appeared, girls (more often) began their speech with tears, decreased self-esteem, in comparison with the healthy contingent, the reliability indicator was P <0.01. Learning difficulties were noted in children of the main group in 26% of cases (mild impairment), and in 13% (learning lag is considered below average). A survey conducted by parents indicated the difficulty of contacting the child, lack of understanding, “isolation,” lack of desire to help parents around the house, emotional lability (reaction), decreased appetite, drowsiness (not related to taking antiallergic therapy), and fear of the dark. It should be noted that on the part of the parents, a peculiarity is noted: the more the parents surround the child with asthma with care and attention, the more they lose the relationship and mutual understanding; in the comparative analysis of children with asthma and healthy children (in this family), the reliability indicator reached P <0.05. Evaluating the results of the (anonymous) survey questionnaire from peers, it turned out to be quite diverse, the majority of the children did not care (lack of interest), and some considered them “weak-willed”, suspicious, and complex because the opinion of peers could not be called objective, This survey was conducted to strengthen the overall picture of the patient’s psychoneurological character; the indicators were not reliable enough. (Figure 1).
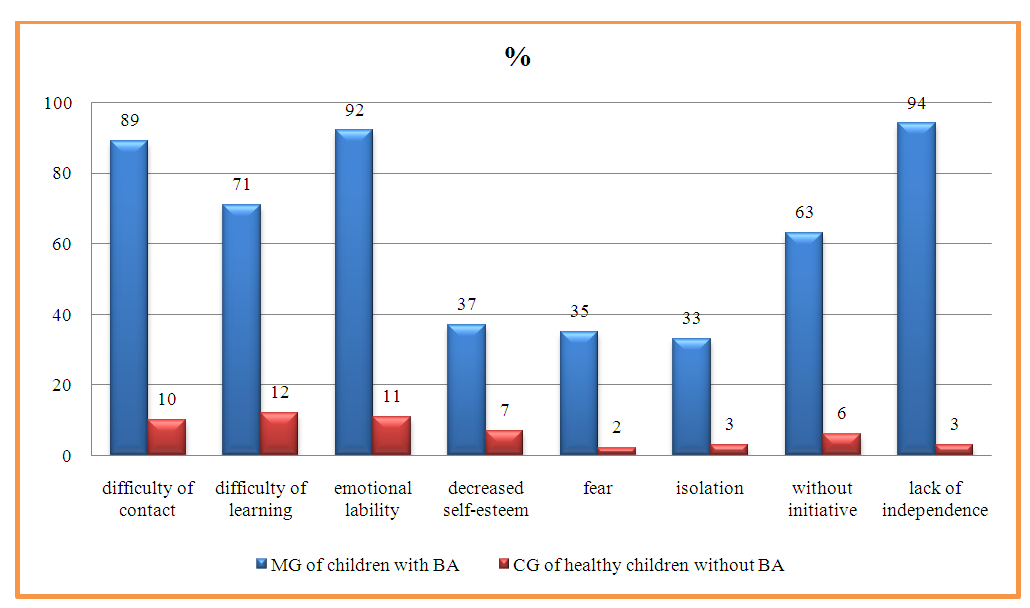 | Figure 1. Analysis of the results of a survey of teachers and parents regarding the attitude of children with bronchial asthma to the level of psychoneurological disorders |
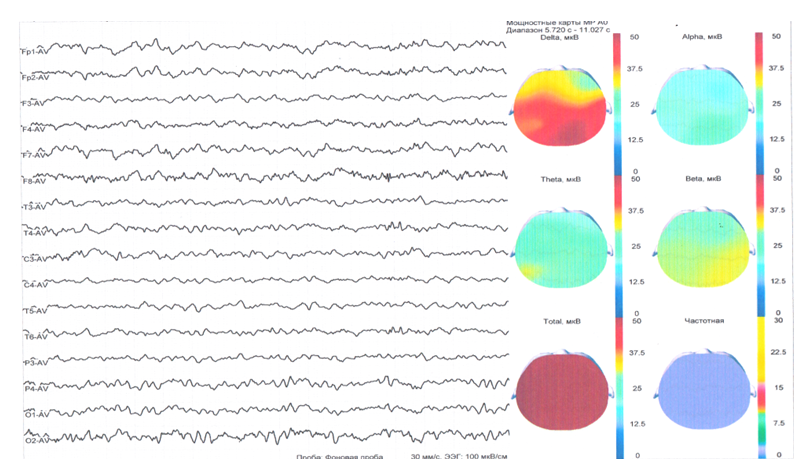
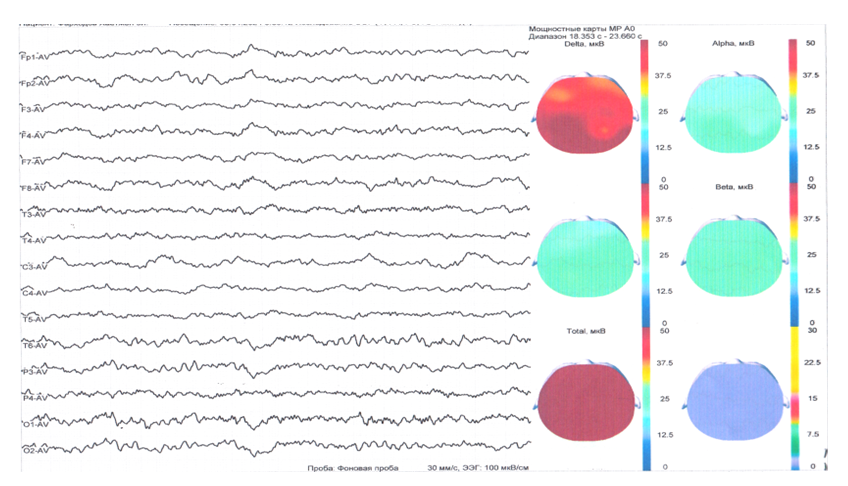 | Figure 2. Patient F., born in 2015 Minor diffuse EEG changes without signs of local pathology are recorded. A decrease in sharpness and deformation of the background rhythm is recorded |
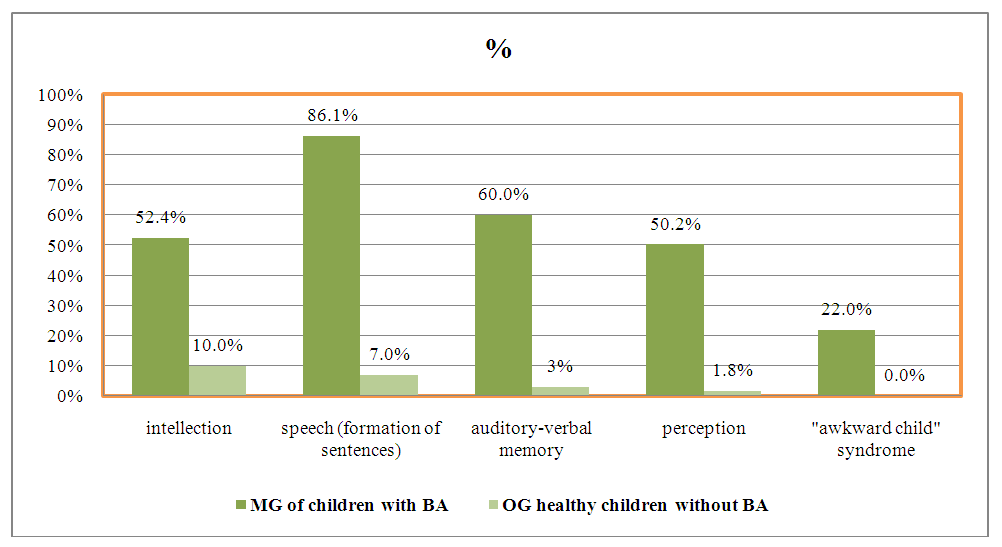 | Figure 4. Analysis of the results of examination of children with bronchial asthma for the level of cognitive impairment according to the Wechsler scale |
4. Conclusions
- Analysis of the results of a comprehensive clinical-neurological, neurophysiological, neuropsychological and neuroimaging study of children with bronchial asthma presented the peculiarity of the nature of the state of the central nervous system of children, which reflects the relationship of these changes with the level of severity of the underlying disease, period and duration of the disease. Clinical neurological signs in the form of small focal symptoms, neurophysiological indicators of general diffuse bioelectrical changes, decreased functional activity of the brain were found to be significant for the diagnosis of children with AD; testing revealed a high percentage of impaired cognitive symptoms and emotional cognition, anxiety disorders, decreased mental performance, depending on different course of asthma.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML