-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1409-1412
doi:10.5923/j.ajmms.20241405.57
Received: Apr. 1, 2024; Accepted: May 3, 2024; Published: May 23, 2024

Pathomorphology of Disregenerator Processes Developed in the Chronic Period of Nonspecific Ulcerative Colitis
Saydaliev Sodikjon Saibjanovich1, Isroilov Rajab Isroilovich2, Saidjonova Feruza Latifjonova1
1Department of Pathological anatomy and Forensic Medicine, Andijan State Medical Institute, Andijan, Uzbekistan
2Department of Pathological Anatomy, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this article, the morphological changes characteristic of the chronic period of NUC were studied. As a material, a biopsy of a piece of intestine obtained during surgical practice in the proctology department of the ASMI clinic in the years 2012-2022 was studied morphologically. The results showed that in the chronic period of NUC morphologically most of the mucous membrane of the large intestine is superficial, i.e., occupying the surface layers of the mucous membrane, both small and large-scale, with the presence of wounds that penetrate into the submucosa layer in some cases, with hyperplasia of lymphoid follicles, infiltration into the surrounding tissues. It was confirmed that it was manifested by the spread. It has been proven that the appearance of pseudopolyps, which develop as dysregenerative processes during the remission period of NUC, has two different histological structures, that is, the appearance of hyperplastic tumors of the private plate with connective tissue and the appearance of metaplastic small papillae-like polyps in the form of papillae on the surface of the mucous membrane.
Keywords: Intestine, NUC (Nonspecific ulcerative colitis), Biopsy, Morphology, Remission, Pseudopolyp
Cite this paper: Saydaliev Sodikjon Saibjanovich, Isroilov Rajab Isroilovich, Saidjonova Feruza Latifjonova, Pathomorphology of Disregenerator Processes Developed in the Chronic Period of Nonspecific Ulcerative Colitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1409-1412. doi: 10.5923/j.ajmms.20241405.57.
1. Introduction
- Nonspecific ulcerative colitis (NUC) is a chronic relapsing autoimmune inflammatory disease of the colon mucosa in the human body, characterized by the development of intestinal and extraintestinal changes and complications, which in most cases causes disability and death of patients [7,9]. In the world, NUC occurs in 35-100 people per 100,000 people, and it occurs in less than 0.1% of the world's population [1,2]. The disease is more often observed in patients under the age of 20-40 years.From the initial clinical signs of the disease to the clinical-pathogistological diagnosis, it takes several months and even years, and long-term manifestations are manifested by extraintestinal symptoms. In 15-20% of cases, NUC is recorded in the entire large intestine, in 30-50% of cases in the large intestine, and in 30-50% of cases in the rectum. The main part of NUC is observed between the ages of 20 and 40, and it appears with the same frequency in men and women. Nonspecific ulcerative colitis can lead to the development of systemic toxic reactions of the body, life-threatening pathologies.Nonspecific risk factors for the development of ulcerative colitis include: the spread of the process, the duration of the disease, the early onset of the disease, family history of colon cancer, the presence of primary sclerosing cholangitis, folic acid deficiency, etc. [3,4,5,6]. The duration of development of colon cancer from NUC is often noted when it is more than 7-8 years. The most important risk factor for the development of colon cancer in the general population is the age of the patients: the highest rate occurs in men and women over 60 years of age. Recently, it is observed that the incidence of colon cancer is moving towards middle-aged people - getting younger: the average age of patients is 30-45 years [8,10,11].According to WHO data, studying the clinical and morphological characteristics of the organs of the gastrointestinal tract, in particular, the nonspecific ulcerative colitis of the large intestine, remains an actual source of medical research. Particular attention is paid to ulcerative colitis, which can lead to the development of intestinal and extraintestinal complications, such as the development of systemic toxic reactions, bleeding, pseudopolyps, toxic expansion, intestinal perforation, malignancy and metastasis. Based on this, the study of disregenerative processes in the pathomorphological changes of the stages of ulcerative colitis, the search for methods of early detection of pre-tumor and tumor processes with probable origin, their use in practice remains one of the most important directions in this field.
2. Material and Methods
- In the course of the research, diagnostic biopsy materials of patients treated surgically with chronic non-specific ulcerative colitis in the proctology department of ADTI in 2012-2022 were studied by pathogistological, i.e. general-morphological, morphometric, histochemical and immunohistochemical methods. Tissue pieces were first fixed in 10% phosphate-buffered formalin for 72 hours, then washed in running water for 4 hours. Dehydration was carried out in portions of increasing concentration of alcohol, paraffin with wax was poured, and blocks were prepared. Histological sections with a thickness of 5-7 μm were taken from paraffin blocks, deparaffinized, and stained with nematoxylin and eosin. Preparations were studied under 10, 20, 40 lenses of a microscope, microphotographs of the necessary areas were downloaded to the computer.
3. Results and Discussion
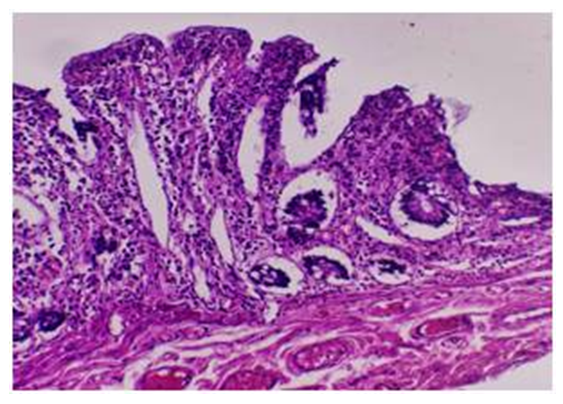
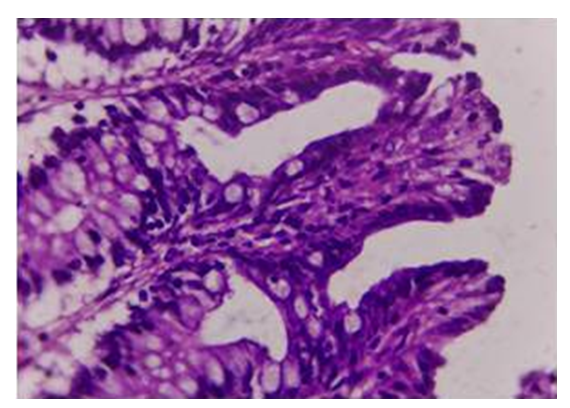
- In the chronic form of NUC, when the part of the colon removed during surgery was examined macroscopically, it was found that the folds of the mucous membrane of the colon are deformed, and it has an uneven appearance due to the presence of ulcers of various sizes and shapes and polypoid bumps. It is determined that the wound defects are round or of an unclear shape, most of them are small and superficial, occupy a large area in some places, and have uneven edges. It is determined that the outer serous membrane of the intestinal wall is almost diffusely hyperemic, reddened, swollen, and blood is poured in some places. In some cases, it is determined that the wounds on the mucous membrane of the large intestine are relatively closed, and in their place, small and numerous pseudopolyps appear, slightly protruding from the mucous membrane.Microscopic examination showed that the mucous membrane of the large intestine is thickened to varying degrees due to the presence of chronic inflammation and wounding foci. It is found that covering epithelium has migrated in almost all areas, crypts are deformed due to swelling and inflammatory infiltrate, crypts have disappeared in some areas and chronic proliferative inflammatory infiltrate has taken their place (Fig. 1). When the cellular composition of the inflammatory infiltrate is studied, it is found that mainly proliferated and activated lymphoid and histiocytic cells are located in a diffuse and dense manner. From lymphoid cells, small and medium-sized lymphocytes, plasma cells are found scattered (Fig. 2). Young histiocytic cells, macrophages, epithelioid cells, polynuclear leukocytes, neutrophils and eosinophils are found among histiocytic cells. It is observed that there are relatively few fibrous structures between cells and they are located in small fragments.
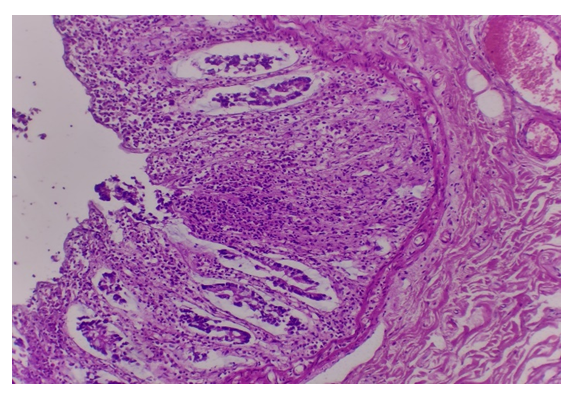 | Figure 1. The chronic period of NUC, the presence of focal proliferative inflammatory infiltrate in the mucous membrane. Paint: H-E. Zoom: 10x10 |
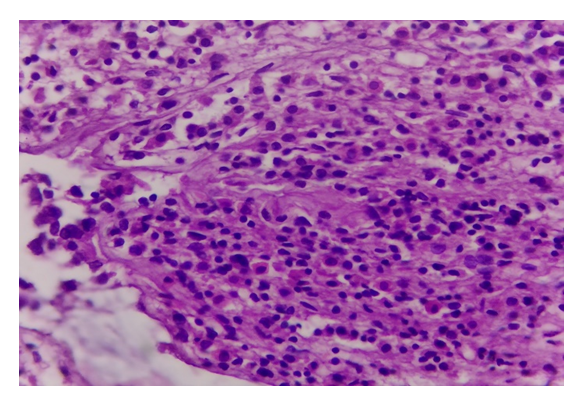 | Figure 2. The chronic period of NUC, the proliferative infiltrate consists of lymphoid and histiocytic cells. Paint: H-E. Zoom: 10x40 |
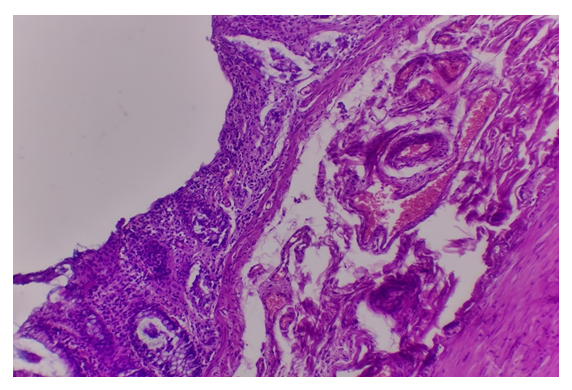 | Figure 3. The chronic period of NUC, the presence of a superficial ulcer on the mucous membrane of the large intestine. Paint: H-E. Zoom: 10x10 |
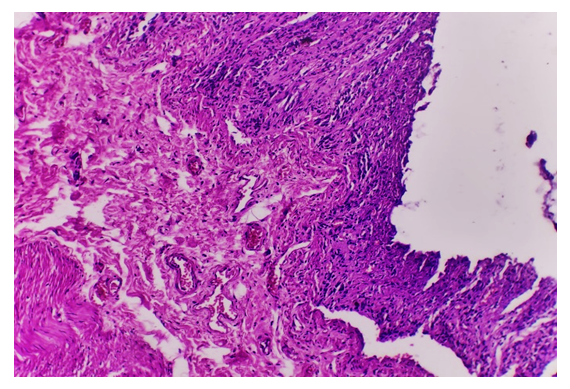 | Figure 4. The chronic period of NUC, the appearance of a deep ulcer in the mucous membrane of the large intestine. Paint: H-E. Zoom: 10x10 |
 | Figure 5. In the chronic period of NUC, swelling in the form of a pseudopolyp due to the proliferation and inflammation of the private plate on the mucous membrane. Paint: H-E. Zoom: 10x40 |
 | Figure 6. In the chronic period of NUC, the appearance of small papillary polypous tumors, the surface of which is covered with epithelium, in the mucous membrane. Paint: H-E. Zoom: 10x40 |
4. Conclusions
- The chronic phase of the chronic period of the colonic mucosa is morphologically manifested by the presence of ulcers, which occupy the surface layers of the mucous membrane, both small and large-scale, and in some cases penetrate into the submucosa, hyperplasia of lymphoid follicles, infiltrating and spreading to the surrounding tissues. confirmed.It was found that the composition of the chronic proliferative inflammatory infiltrate consisted mainly of activated lymphoid and histiocytic cells, among which neutrophils and eosinophilic polynuclear leukocytes took place.It has been proven that the appearance of pseudopolyps, which develop as dysregenerative processes during the remission period of NUC, has two different histological structures, that is, the appearance of hyperplastic tumors of the private plate with connective tissue and the appearance of metaplastic small papillae-like polyps in the form of papillae on the surface of the mucous membrane.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML