-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1404-1408
doi:10.5923/j.ajmms.20241405.56
Received: Apr. 1, 2024; Accepted: May 3, 2024; Published: May 23, 2024

Epilepsy and COVID-19
Khanifa Khalimova, Nilufar Rashidova, Saykha Ilkhomova
Tashkent Medical Academy Department of Neurology and Medical Psychology, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In late 2019, a new virus causing respiratory disease emerged in Wuhan, China. It soon spread around the world, and on March 11, 2020, the World Health Organization officially declared a pandemic of a new coronavirus infection, COVID-19. COVID-19 is caused by the SARS-CoV-2 coronavirus, which is transmitted from person to person through droplets released by coughing or sneezing. Symptoms of the disease include fever, cough, fatigue, muscle aches, and headache. Some people may have more serious symptoms, including pneumonia and acute respiratory failure, which can be fatal. The disease has triggered a worldwide pandemic that has had a significant impact on health because it affects people's nervous systems. COVID-19 can lead to a variety of short- and long-term health effects. The main symptoms of the disease include fever, cough, difficulty breathing, loss of smell and impaired taste. However, some patients may experience more serious consequences.
Keywords: Affects people's nervous systems, Illness, Headaches, Dizziness, Impaired coordination
Cite this paper: Khanifa Khalimova, Nilufar Rashidova, Saykha Ilkhomova, Epilepsy and COVID-19, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1404-1408. doi: 10.5923/j.ajmms.20241405.56.
1. Introduction
- One of the complications associated with COVID-19 are neurological manifestations that can affect the nervous system. These can be seen in both patients who are severely ill and those who have no obvious signs of the disease. Neurologic manifestations include headaches, dizziness, impaired coordination, speech and vision, as well as seizures and loss of consciousness. [1,2,3] In addition, COVID-19 can have an impact on people's mental health. Many people feel stress and anxiety due to the risk of illness, limitations in daily life, loss of loved ones, and uncertainty about the future. These factors can lead to the development of depression, anxiety, and other mental health disorders. Some studies also show a link between COVID-19 and long-term neurological effects. Some patients who have had the disease report memory impairment.To investigate the incidence, risk factors, mechanisms, diagnosis, treatment and prognosis of seizures and epilepsy in patients with covid-19. We also aimed to investigate the potential impact of covid-19 on the management and quality of life of patients with existing epilepsy.
2. Materials and Methods
- For this review, we systematically searched 35 articles in PubMed, Web of Science, and Scopus databases using the following keywords: (covid OR coronavirus OR SARS-CoV-2) AND (epilepsy OR seizure OR convulsion). We limited our search to articles published between January 2020 and May 2023 and excluded duplicates, reviews, letters, and comments. We also checked the reference list of selected articles for additional relevant sources.As mentioned above, COVID-19 may affect the nervous system and cause various neurological manifestations. Several studies have been conducted to investigate this issue. One study published in The Lancet Neurology found that 36.4% of patients hospitalized with COVID-19 had neurological manifestations. This included headaches, dizziness, seizures, and impaired consciousness. The majority of patients with neurologic manifestations showed changes on magnetic resonance imaging of the brain. Another study published in JAMA Neurology found that COVID-19 can cause acute brain damage, which can lead to seizures, impaired consciousness, and death. The study also found that COVID-19 can cause acute myelitis, which is an inflammatory disease of the spinal cord. Patients with more severe infection had neurological manifestations such as acute cerebrovascular disease ([0.8%]), impaired consciousness (13 [14.8%] and skeletal muscle damage [19.3%] [1].However, it is also known that neurological complications, including seizures and epileptic conditions, may occur in some patients, especially those who have had a severe course of the disease. These complications can be related to the central nervous system and can occur either as a direct result of the virus directly affecting the brain or as a result of the body's immune responses to the infection. Seizures and epileptic seizures can occur in patients with COVID-19 at any time, including during hospitalization, after discharge, and even after full recovery. Seizures and epileptic seizures may be the first manifestations of COVID-19, and can sometimes begin before other symptoms appear. Patients who survive COVID-19 and have epileptic seizures may have a prolonged recovery and require long-term therapy. [2]Pathogenesis effects of COVID-19 on the nervous system Mechanisms of COVID-19 effects on the nervous system. In this review article, we will present the opinions and studies of world scientists on the effects of COVID 19 infection on epilepsy.Epilepsy is a neurological disorder that manifests itself as sudden and unexpected episodes of seizures and loss of consciousness. It can be caused by a variety of reasons, including infections, head injuries, tumors, and genetic disorders. Recently, scientists have discovered that COVID-19 may be another cause of the development and progression of epilepsy.The study analyzed data from 24,000 patients who had COVID-19. Researchers found that the risk level for developing epilepsy after COVID-19 nearly doubles compared to the general population. In addition, patients who developed COVID-19 with complications such as pneumonia had an even higher risk of developing epilepsy. The study also showed that the level of epilepsy risk after COVID-19 depended on the severity of the disease. Patients who had severe COVID-19 had twice the risk of developing epilepsy than those who had a mild form of the disease. Although the association between COVID-19 and epilepsy requires further research, the results of this meta-analysis emphasize the importance of monitoring neurological symptoms in patients who have had COVID-19. In addition, this study may help to develop strategies for the prevention and treatment of epilepsy in patients who have undergone COVID-19. [3] Overall, the results of this study represent an important contribution to our understanding of the association between COVID-19 and neurological complications such as epilepsy and emphasize the need for additional research in this area.COVID-19 may be associated with new cases of epilepsy. Several studies have shown that patients with COVID-19 have had cases of de novo epilepsy, that is, epilepsy that develops for the first time without prior symptoms. Some patients with COVID-19 may have seizures. Seizures can be one of the symptoms of COVID-19, and they can occur in patients with no prior history of epilepsy. And it may also worsen epilepsy control in patients with a prior history of epilepsy. Some studies have shown that epilepsy patients infected with COVID-19 may experience worsening epilepsy control. Some medications used to treat COVID-19 may affect epilepsy. For example, remdesivir, one of the drugs used to treat COVID-19, may increase the risk of seizures.
3. Results and Discussions
- Immune mechanisms may play a role in the link between COVID-19 and epilepsy. Some studies have shown that patients with COVID-19 had increased levels of neuron-associated antibodies, which may be associated with the development of epilepsy. [4].At the moment, studying the effect of antibodies on epilepsy after COVID-19 is an active area of research, but definitive conclusions have yet to be formulated. Some studies have shown that COVID-19 patients may have an increased risk of developing epilepsy, but the reasons for this phenomenon are not fully understood. Theoretically, the formation of antibodies in response to infection can cause inflammatory processes that can damage brain cells and increase the risk of epilepsy.Recently, scientists have discovered that COVID-19 can cause epileptic seizures in some patients. This mechanism is related to the direct effect of the virus on the brain as well as the body's immune response to the infection. In this article, we will review the mechanisms that underlie epilepsy after COVID-19 and discuss some of the studies that support this link. There is also a suggestion that COVID-19 may increase the risk of epilepsy because the virus can cause hypoxia (oxygen deprivation) and increased immune system activity, which can lead to brain cell damage.Once infected with COVID-19, the virus begins to multiply in the body, triggering an immune response. It is possible for the virus to enter the brain through the bloodstream or through olfactory receptors in the nose. This can lead to inflammation in the brain, which can cause epileptic seizures. Studies have also shown that an immune response to COVID-19 can lead to epilepsy. In response to infection, the immune system begins to produce antibodies and other substances that can cause inflammation in the brain. This inflammation can damage nerve cells and cause epileptic seizures. The mechanisms that underlie epilepsy after COVID-19 are still not fully understood. For example, authors Garg RK, Paliwal VK, Gupta A, et al. state that Covid-19 can cause various neurological complications including brain inflammation and neuronal damage. COVID-19 infection may affect the nervous system through several mechanisms including direct virus exposure to nervous tissue, hypoxia, cytokine storm, immunomodulation, thromboembolism and other factors. (Garg RK, Paliwal VK, Gupta A 2020). [18]However, in most cases, epileptic seizures after COVID-19 are related to direct exposure of the virus to the brain or to the immune response to infection. Although epilepsy after COVID-19 is not a recognized problem, it can still be a serious complication in some patients. Therefore, it is important to pay attention to any epileptic seizures that may occur after COVID-19 infection. Research in this area is still ongoing, and scientists are trying to better understand the mechanisms that underlie epilepsy after COVID-19. This may help to develop new treatments and prevent this complication in patients with COVID-19. [7]Several studies conducted in 2020 have found that patients who have had COVID-19 may have an increased risk of developing epilepsy. For example, a study published in the journal Epilepsia found that 13% of 125 patients who underwent COVID-19 developed new epileptic seizures. Another study published in the journal Seizure found that 6% of 509 patients who underwent COVID-19 developed epileptic activity in EEG monitoring. [8,9] However, it should be noted that these studies have limitations such as small sample size and lack of control groups. Also, further studies are needed to elucidate the mechanisms involved in the development of epilepsy in COVID-19 patients. Overall, it can be concluded that COVID-19 may increase the risk of developing epilepsy in some patients. Further studies are needed to better assess this risk and to elucidate the mechanisms associated with this effect. Several studies conducted in different countries (e.g., China, Italy, and India) have shown that some patients on COVID-19 experience seizures and epileptic seizures. In one study conducted in China, 1.4% of patients with COVID-19 had seizures and 0.5% had epileptic seizures. In another study conducted in Italy, 15% of patients who were on ventilator had seizures [1,10,11]. However, recent studies also suggest that in some COVID-19 patients, antibodies may have a protective effect and prevent the development of epilepsy. Overall, more studies are needed to more accurately assess the effect of antibodies on the development of epilepsy after COVID-19. However, it is not yet clear how SARS-CoV-2 can induce epilepsy. There is speculation that it may be related to a cytokine storm that causes inflammation in the body and can damage brain cells. There is also a possible link between COVID-19 and some other factors that may contribute to epilepsy, such as stress, lack of sleep, and side effects of medications that are used to treat COVID-19.Effect of COVID-19 on the pathogenesis of epilepsy:
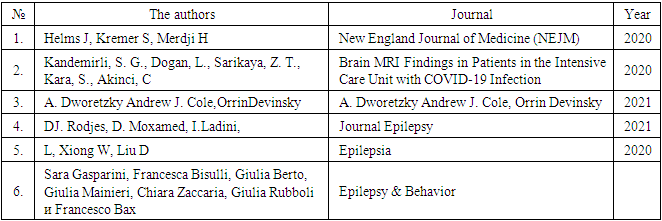 Thus, while there is currently no definitive data on how COVID-19 may affect the pathogenesis of epilepsy, there is some research available. According to studies, the most common occurrence in patients with COVID-19 is the development of new epilepsy or exacerbation of existing epilepsy. This can occur either during the course of the disease or after the disease is over. That said, exacerbations of epilepsy can occur in both patients with severe COVID-19 and those who have had a mild course of the disease. Other studies show that COVID-19 can cause damage to blood vessels in the brain, which can also cause epileptic seizures. Damage to blood vessels can lead to impaired blood flow in the brain, which can damage nerve cells and cause epileptic seizures. [6] For example, in the article "COVID-19 and Epilepsy: A Systematic Review" (published in Frontiers in Neurology in 2020), the authors analyzed the information available at the time about the effects of COVID-19 on epilepsy. It is noted that some patients with COVID-19 may experience worsening of epilepsy or new epileptic seizures. Some studies have also found that COVID-19 can cause inflammation in the brain, which can lead to epileptiform seizures. Inflammation can occur because the virus can enter the brain through the bloodstream or nervous system. [10,16]Another article published in the journal Epilepsy & Behavior in 2021 describes the case of an epileptic patient who experienced an exacerbation of epilepsy after COVID-19 disease. The authors discuss possible mechanisms that may explain the link between COVID-19 and epilepsy, including brain inflammation and lack of oxygen.Although the association between COVID-19 and epilepsy requires further study, it is already known that patients with epilepsy are at risk for severe COVID-19 and should be strictly followed for prevention.In addition, the article "COVID-19 and Epilepsy: Clinical Outcomes from the COV-EPILEPSY Registry" (published in the journal Epilepsy & Behavior in 2021) describes the results of a study based on a registry of epilepsy patients who were infected with COVID-19. The study identified several factors that may increase the risk of a severe course of COVID-19 in patients with epilepsy, including the presence of comorbidities such as diabetes and obesity, and the use of certain antiepileptic drugs. [12]Some studies have described the clinical case of five patients with epilepsy who were confirmed to have COVID-19 disease. Here are some of the facts they described:- All five patients had a history of epilepsy and all were on antiepileptic therapy.- Three patients had worsening epileptic seizures due to COVID-19 disease.- One patient had epileptic seizures for the first time after COVID-19 disease.- All five patients showed electroencephalogram (EEG) changes such as increased activity and/or changes in oscillation frequency.- Two patients showed brain magnetic resonance imaging (MRI) changes associated with an inflammatory response.It is noted that these findings emphasize the need for further investigation of the relationship between COVID-19 and epilepsy, and the importance of monitoring patients with epilepsy in the context of a COVID-19 pandemic. [13]Several studies have shown that coronavirus infection may be associated with the development of epilepsy or exacerbation of existing cases of this condition. One study, published in the journal Epilepsia in 2021, found that patients with COVID-19 who had neurological complications, such as Guillain-Barré disease or cerebral palsy, had a higher risk of developing epilepsy. [14]Another study, the Chinese Journal of Neurology in August 2021. This study examined the medical records of 304 patients with COVID-19 who were hospitalized in a hospital in Wuhan, China at the beginning of the pandemic.The study found that 11 of the 304 patients (3.6%) had epileptic seizures. It also found that patients with epileptic seizures had higher rates of other neurological complications such as impaired consciousness, Guillain-Barré disease and brain damage compared to those who did not have epileptic seizures. Conducted in China, reports that patients who received COVID-19 and were hospitalized had a higher incidence of epilepsy than patients who did not receive COVID-19. [15]Study authors include researchers from various universities and medical centers around the world, including Yale University, University of Cincinnati, China National University, and others. The studies used a variety of methods, including analysis of patient medical records, neurophysiologic studies, and observation of patients with COVID-19.New onset acute symptomatic seizure and risk factors in coronavirus disease 2019: a retrospective multicenter study" describes the results of a study conducted at several medical centers in China to investigate the risks and factors associated with the occurrence of new onset acute symptomatic seizures in patients with COVID-19. It is stated that 24 (0.5%) of 5,374 patients with COVID-19 had new acute symptomatic seizures. Most of them (87.5%) had seizures within the first two weeks of COVID-19 onset. According to L. Xiong, W. Liu et al. found that the presence of severe COVID-19, elevated C-reactive protein (CRP) and elevated blood levels of lactate dehydrogenase (LDH) were associated with an increased risk of new acute symptomatic seizures in patients with COVID-19.The authors also note that most patients with COVID-19 and new acute symptomatic seizures had other neurologic symptoms such as headache, somnolence, and impaired consciousness. (L. Xiong, W. Liu 2020). [17]Effects of COVID-19 on neurophysiologic activity.In addition to the effect of coronavirus infection on the course of epilepsy, it has also been observed to have many effects on neurophysiologic state. The effect of Covid-19 on neurophysiologic activity in the brain is a topic that is attracting increasing attention from researchers.Studying the neurophysiologic changes induced by Covid-19 is challenging because the mechanisms leading to these changes can be diverse. Some studies have shown that Covid-19 can induce brain inflammation, which can lead to neuronal damage and decreased functional brain activity and in EEG increased delta waves. These facts are mentioned in several scientific publications. However, some studies have shown that the virus can lead to increased levels of glutamate, a substance that is a neurotransmitter and plays an important role in the transmission of nerve impulses. Glutamate levels may be elevated due to the inflammatory process in the brain caused by COVID-19. This can lead to over-activation of nerve cells and epileptic seizures." [5]Also according to the opinions of Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, et al, published in the journal Neurology in 2020, states that Covid-19 can cause neurological symptoms such as headaches, impaired consciousness, and epileptic seizures, which may indicate the effects of the virus on the nervous system. (Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E) [19] However, it should be noted that research in this area is ongoing and not all mechanisms of Covid-19's effects on the nervous system are fully understood at this time.Recent studies have shown that COVID-19 can cause various neurological disorders, including epilepsy. In addition, patients with COVID-19 who have epileptic seizures may exhibit changes in the electroencephalogram (EEG). A.V. Lebedova et al. investigated clinical, neurophysiologic, and psychological parameters in three groups of patients: with epilepsy after COVID-19, with epilepsy without COVID-19, and without epilepsy after COVID-19. They found that patients with epilepsy after COVID-19 had an increase in epileptiform activity on the EEG, an increase in the frequency of rare epileptic seizures, an increase in the sympathetic nervous system's influence on heart rate, and an increase in the severity of anxiety and depression. The authors conclude that these results may help in assessing the neuropsychiatric status of patients with epilepsy after COVID-19 and in developing optimal directions for treatment and prevention of the disease. Following the study, Lambrecq et al. conducted a literature review and discussed the electroencephalographic changes in epilepsy associated with COVID-19.
Thus, while there is currently no definitive data on how COVID-19 may affect the pathogenesis of epilepsy, there is some research available. According to studies, the most common occurrence in patients with COVID-19 is the development of new epilepsy or exacerbation of existing epilepsy. This can occur either during the course of the disease or after the disease is over. That said, exacerbations of epilepsy can occur in both patients with severe COVID-19 and those who have had a mild course of the disease. Other studies show that COVID-19 can cause damage to blood vessels in the brain, which can also cause epileptic seizures. Damage to blood vessels can lead to impaired blood flow in the brain, which can damage nerve cells and cause epileptic seizures. [6] For example, in the article "COVID-19 and Epilepsy: A Systematic Review" (published in Frontiers in Neurology in 2020), the authors analyzed the information available at the time about the effects of COVID-19 on epilepsy. It is noted that some patients with COVID-19 may experience worsening of epilepsy or new epileptic seizures. Some studies have also found that COVID-19 can cause inflammation in the brain, which can lead to epileptiform seizures. Inflammation can occur because the virus can enter the brain through the bloodstream or nervous system. [10,16]Another article published in the journal Epilepsy & Behavior in 2021 describes the case of an epileptic patient who experienced an exacerbation of epilepsy after COVID-19 disease. The authors discuss possible mechanisms that may explain the link between COVID-19 and epilepsy, including brain inflammation and lack of oxygen.Although the association between COVID-19 and epilepsy requires further study, it is already known that patients with epilepsy are at risk for severe COVID-19 and should be strictly followed for prevention.In addition, the article "COVID-19 and Epilepsy: Clinical Outcomes from the COV-EPILEPSY Registry" (published in the journal Epilepsy & Behavior in 2021) describes the results of a study based on a registry of epilepsy patients who were infected with COVID-19. The study identified several factors that may increase the risk of a severe course of COVID-19 in patients with epilepsy, including the presence of comorbidities such as diabetes and obesity, and the use of certain antiepileptic drugs. [12]Some studies have described the clinical case of five patients with epilepsy who were confirmed to have COVID-19 disease. Here are some of the facts they described:- All five patients had a history of epilepsy and all were on antiepileptic therapy.- Three patients had worsening epileptic seizures due to COVID-19 disease.- One patient had epileptic seizures for the first time after COVID-19 disease.- All five patients showed electroencephalogram (EEG) changes such as increased activity and/or changes in oscillation frequency.- Two patients showed brain magnetic resonance imaging (MRI) changes associated with an inflammatory response.It is noted that these findings emphasize the need for further investigation of the relationship between COVID-19 and epilepsy, and the importance of monitoring patients with epilepsy in the context of a COVID-19 pandemic. [13]Several studies have shown that coronavirus infection may be associated with the development of epilepsy or exacerbation of existing cases of this condition. One study, published in the journal Epilepsia in 2021, found that patients with COVID-19 who had neurological complications, such as Guillain-Barré disease or cerebral palsy, had a higher risk of developing epilepsy. [14]Another study, the Chinese Journal of Neurology in August 2021. This study examined the medical records of 304 patients with COVID-19 who were hospitalized in a hospital in Wuhan, China at the beginning of the pandemic.The study found that 11 of the 304 patients (3.6%) had epileptic seizures. It also found that patients with epileptic seizures had higher rates of other neurological complications such as impaired consciousness, Guillain-Barré disease and brain damage compared to those who did not have epileptic seizures. Conducted in China, reports that patients who received COVID-19 and were hospitalized had a higher incidence of epilepsy than patients who did not receive COVID-19. [15]Study authors include researchers from various universities and medical centers around the world, including Yale University, University of Cincinnati, China National University, and others. The studies used a variety of methods, including analysis of patient medical records, neurophysiologic studies, and observation of patients with COVID-19.New onset acute symptomatic seizure and risk factors in coronavirus disease 2019: a retrospective multicenter study" describes the results of a study conducted at several medical centers in China to investigate the risks and factors associated with the occurrence of new onset acute symptomatic seizures in patients with COVID-19. It is stated that 24 (0.5%) of 5,374 patients with COVID-19 had new acute symptomatic seizures. Most of them (87.5%) had seizures within the first two weeks of COVID-19 onset. According to L. Xiong, W. Liu et al. found that the presence of severe COVID-19, elevated C-reactive protein (CRP) and elevated blood levels of lactate dehydrogenase (LDH) were associated with an increased risk of new acute symptomatic seizures in patients with COVID-19.The authors also note that most patients with COVID-19 and new acute symptomatic seizures had other neurologic symptoms such as headache, somnolence, and impaired consciousness. (L. Xiong, W. Liu 2020). [17]Effects of COVID-19 on neurophysiologic activity.In addition to the effect of coronavirus infection on the course of epilepsy, it has also been observed to have many effects on neurophysiologic state. The effect of Covid-19 on neurophysiologic activity in the brain is a topic that is attracting increasing attention from researchers.Studying the neurophysiologic changes induced by Covid-19 is challenging because the mechanisms leading to these changes can be diverse. Some studies have shown that Covid-19 can induce brain inflammation, which can lead to neuronal damage and decreased functional brain activity and in EEG increased delta waves. These facts are mentioned in several scientific publications. However, some studies have shown that the virus can lead to increased levels of glutamate, a substance that is a neurotransmitter and plays an important role in the transmission of nerve impulses. Glutamate levels may be elevated due to the inflammatory process in the brain caused by COVID-19. This can lead to over-activation of nerve cells and epileptic seizures." [5]Also according to the opinions of Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, et al, published in the journal Neurology in 2020, states that Covid-19 can cause neurological symptoms such as headaches, impaired consciousness, and epileptic seizures, which may indicate the effects of the virus on the nervous system. (Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E) [19] However, it should be noted that research in this area is ongoing and not all mechanisms of Covid-19's effects on the nervous system are fully understood at this time.Recent studies have shown that COVID-19 can cause various neurological disorders, including epilepsy. In addition, patients with COVID-19 who have epileptic seizures may exhibit changes in the electroencephalogram (EEG). A.V. Lebedova et al. investigated clinical, neurophysiologic, and psychological parameters in three groups of patients: with epilepsy after COVID-19, with epilepsy without COVID-19, and without epilepsy after COVID-19. They found that patients with epilepsy after COVID-19 had an increase in epileptiform activity on the EEG, an increase in the frequency of rare epileptic seizures, an increase in the sympathetic nervous system's influence on heart rate, and an increase in the severity of anxiety and depression. The authors conclude that these results may help in assessing the neuropsychiatric status of patients with epilepsy after COVID-19 and in developing optimal directions for treatment and prevention of the disease. Following the study, Lambrecq et al. conducted a literature review and discussed the electroencephalographic changes in epilepsy associated with COVID-19.4. Conclusions
- In particular, the authors note that during epileptic seizures, patients with COVID-19 may exhibit increased amplitude and frequency of delta waves (0.5-4 Hz) in the EEG, as well as increased high-frequency waves (greater than 30 Hz), which may indicate the presence of focal epileptic activity. (Lambrecq 2021) [20]. It is also worth noting that some patients with COVID-19 who have no previously diagnosed epilepsy may develop epileptic seizures as a result of exposure of the brain to the virus. In such cases, an EEG may be helpful in diagnosing and determining the type of epileptic activity. However, it should be noted that data on EEG changes in COVID-19-associated epilepsy are still limited. Most studies have been conducted on a small sample of patients, so further studies are needed to confirm these findings.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML